Abstract
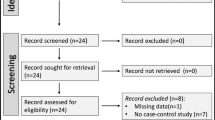
The diagnosis of plasmablastic lymphoma (PBL), plasmablastic myeloma (PBM), and plasmablastic neoplasm (PBN) may be arbitrary in some cases because these entities can be indistinct. We conducted this scoping review to investigate heterogeneity in diagnostic criteria used in previous studies and validate the diagnostic results of previous diagnostic algorithms and the algorithm we developed, which also includes diagnosis of PBN. Using the PRISMA Extension for Scoping Reviews, we analyzed literature published between September 2017 and April 2020. We identified a total of 163 cases (128 PBL, 32 PBM, and 3 PBN) from 77 case reports and 8 case series. We found that diagnostic criteria in the literature varied for PBL but were consistent for PBM. Our algorithm was the first attempt to include PBN in a complete structure. The results of the three diagnostic algorithms varied significantly. Hematologists and pathologists should pay more attention to the differential diagnosis of PBL, PBM, and PBN.




Similar content being viewed by others
References
Vega F, Chang CC, Medeiros LJ, Udden MM, Cho-Vega JH, Lau CC, et al. Plasmablastic lymphomas and plasmablastic plasma cell myelomas have nearly identical immunophenotypic profiles. Mod Pathol. 2005;18:806–15.
Castillo JJ, Bibas M, Miranda RN. The biology and treatment of plasmablastic lymphoma. Blood. 2015;125:2323–30.
Han X, Duan M, Hu L, Zhou D, Zhang W. Plasmablastic lymphoma: review of 60 Chinese cases and prognosis analysis. Medicine (Baltimore). 2017;96:e5981.
Opyrchal M, Figanbaum T, Ghosh A, Rajkumar V, Caples S. Spontaneous tumor lysis syndrome in the setting of B-cell lymphoma. Case Rep Med. 2010;2010:610969.
Omari S, Khalafallah A, Ayesh M, Matalka I, Al-Hadithi R. High serum erythropoietin and ferritin levels in conjunction with anemia response in malignant lymphoma. Mediterr J Hematol Infect Dis. 2011;3:e2011018.
Weeks AC, Kimple ME. Spontaneous tumor lysis syndrome: a case report and critical evaluation of current diagnostic criteria and optimal treatment regimens. J Investig Med High Impact Case Rep. 2015;3:2324709615603199.
Wesemüller W, Taverna C. Spontaneous tumor lysis syndrome. Case Rep Oncol. 2020;13:1116–24.
Chen P, Li B, Zhuang W, Huang H, Zhang H, Fu J. Multiple bone lesions and hypercalcemia presented in diffuse large B cell lymphoma: mimicking multiple myeloma? Int J Hematol. 2010;91:716–22.
Abdullah HMA, Ellithi M, Waqas Q, Cunningham A, Oliver T. Hypercalcaemia, renal dysfunction, anaemia and bone lesions (CRAB) do not always represent multiple myeloma: diffuse large B cell lymphoma presenting with CRAB symptoms in a 69-year-old man. BMJ Case Rep. 2019;12:e229070.
McKenna RWKR, Kuehl WM, Harris NL, et al. Plasma cell neoplasms. WHO classification of tumours of haematopoietic and lymphoid tissues. Lyon: IARC Press; 2017. p. 241–53.
Thumallapally N, Meshref A, Mousa M, Terjanian T. Solitary plasmacytoma: population-based analysis of survival trends and effect of various treatment modalities in the USA. BMC Cancer. 2017;17:13.
Campo ESH, Harris NL. Plasmablastic lymphoma. WHO classification of tumours of haematopoietic and lymphoid tissues. Lyon: IARC Press; 2017. p. 321–2.
Ahn JS, Okal R, Vos JA, Smolkin M, Kanate AS, Rosado FG. Plasmablastic lymphoma versus plasmablastic myeloma: an ongoing diagnostic dilemma. J Clin Pathol. 2017;70:775–80.
Chen B-J, Chuang S-S. Lymphoid neoplasms with plasmablastic differentiation: a comprehensive review and diagnostic approaches. Adv Anat Pathol. 2020;27:61–74.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–73.
Peters MDJ, Godfrey C, McInerney P, Soares CB, Khalil H, Parker D. Scoping Reviews (2020 version). In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis. JBI; 2020. https://synthesismanual.jbi.global. https://doi.org/10.46658/JBIMES-20-12.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Delecluse HJ, Anagnostopoulos I, Dallenbach F, Hummel M, Marafioti T, Schneider U, et al. Plasmablastic lymphomas of the oral cavity: a new entity associated with the human immunodeficiency virus infection. Blood. 1997;89:1413–20.
Kyle RA, Gertz MA, Witzig TE, Lust JA, Lacy MQ, Dispenzieri A, et al. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc. 2003;78:21–33.
Larsen JT, Kumar SK, Dispenzieri A, Kyle RA, Katzmann JA, Rajkumar SV. Serum free light chain ratio as a biomarker for high-risk smoldering multiple myeloma. Leukemia. 2013;27:941–6.
Rafei H, El-Bahesh E, Finianos A, Liu ML, Schechter GP. Plasmablastic lymphoma: case report of prolonged survival of an advanced human immunodeficiency patient and literature review. Case Rep Hematol. 2017;2017:9561013.
do Vale DA, Rogado CM, de Carvalho DLC, Trierveiler M, Ortega KL. Oral plasmablastic lymphoma as the first manifestation of AIDS. An Bras Dermatol. 2017;92:110–2.
Arora N, Gupta A, Sadeghi N. Durable complete remission with combination chemotherapy and bortezomib in HIV-associated plasmablastic lymphoma. BMJ Case Rep. 2017;2017:bcr-2017-222063.
Beltran BE, Quiñones P, Sanchez G, Paredes A, Moises C, Cotrina E, et al. Primary cutaneous plasmablastic lymphoma in an immunocompetent patient: is it associated with an indolent course? Leuk Lymphoma. 2018;59:1753–5.
Zarifi C, Deutsch S, Dullet N, Mukherjee KK, Mukherjee A, Abubaker F. An enlarging pacemaker pocket: a case report of a plasmablastic lymphoma arising as a primary tumor around a cardiac pacemaker and systematic literature review of various malignancies arising at the pacemaker pocket. J Cardiol Cases. 2018;17:41–3.
Annunziata S, Cuccaro A, Caldarella C, Leccisotti L, Hohaus S. 11C-methionine-avid plasmablastic lymphoma. Clin Nucl Med. 2017;42:872–3.
Bloch E, Robinson F. Orbital plasmablastic lymphoma. Clin Case Rep. 2018;6:222–3.
Hadžisejdić I, Babarović E, Vranić L, Duletić Načinović A, Lučin K, Krašević M, et al. Unusual presentation of plasmablastic lymphoma involving ovarian mature cystic teratoma: a case report. Diagn Pathol. 2017;12:83.
Hatzimichael E, Papathanasiou K, Zerdes I, Flindris S, Papoudou-Bai A, Kapsali E. Plasmablastic lymphoma with coexistence of chronic lymphocytic leukemia in an immunocompetent patient: a case report and mini-review. Case Rep Hematol. 2017;2017:2861596.
Qu G, Yu G, Liu J, Sun D, Wang T, Sui X. Gastric plasmablastic lymphoma: case report and review literature. Int J Clin Exp Med. 2017;10:15544–50.
Gosavi AV, Deshmukh BD, Ramteerthakar NA, Sulhyan KR. Cytodiagnosis of extraoral plasmablastic lymphoma in an HIV-positive paediatric patient—a case report and review of the literature. J Clin Diagn Res. 2018;12:ED18–20.
Lukić S, Dragaševi S, Zgradić S, Todorović M, Djuranović S, Andjelić B, et al. Plasmablastic lymphoma as a rare cause of subocclusive events—case report and review of the literature. Vojnosanit Pregl. 2019;76:1297–300.
Migliavacca M, Assanelli A, Ponzoni M, Pajno R, Barzaghi F, Giglio F, et al. First occurrence of plasmablastic lymphoma in adenosine deaminase-deficient severe combined immunodeficiency disease patient and review of the literature. Front Immunol. 2018;9:113.
Ghosh G, Jacob V, Wan D. Plasmablastic lymphoma in a patient with Crohn’s disease after extensive immunosuppressive therapy. Clin Gastroenterol Hepatol. 2018;16:e41–2.
Koizumi Y, Imadome K-I, Ota Y, Minamiguchi H, Kodama Y, Watanabe D, et al. Dual threat of Epstein-Barr Virus: an autopsy case report of HIV-positive plasmablastic lymphoma complicating EBV-associated hemophagocytic lymphohistiocytosis. J Clin Immunol. 2018;38:478–83.
Yamamoto S, Yasuda Y, Sakai Y. Plasmablastic lymphoma presenting as a ureteral polypoid mass. Indian J Urol. 2018;34:152–4.
Marrero WD, Cruz-Chacón A, Castillo C, Cabanillas F. Successful use of bortezomib-lenalidomide combination as treatment for a patient with plasmablastic lymphoma. Clin Lymphoma Myeloma Leuk. 2018;18:e275–7.
Broccoli A, Nanni L, Stefoni V, Agostinelli C, Argnani L, Cavo M, et al. A patient with plasmablastic lymphoma achieving long-term complete remission after thalidomide-dexamethasone induction and double autologous stem cell transplantation: a case report. BMC Cancer. 2018;18:645.
Ise M, Kageyama H, Ikebe D, Araki A, Kumagai K, Itami M. Transformation of double-hit follicular lymphoma to plasmablastic lymphoma: a partial role of MYC gene rearrangement. J Clin Exp Hematop. 2018;58:128–35.
Khan UT, Racu-Amoasii I, Arumainathan A, Meswani U, Pettitt AR, Menon G. Central nervous system plasmablastic lymphoma evolving from polyclonal plasmacytosis. Br J Haematol. 2018;183:345.
Shi J, Bodo J, Zhao X, Durkin L, Goyal T, Meyerson H, et al. SLAMF7 (CD319/CS1) is expressed in plasmablastic lymphoma and is a potential diagnostic marker and therapeutic target. Br J Haematol. 2019;185:145–7.
Diaz R, Amalaseelan J, Imlay-Gillespie L. Plasmablastic lymphoma masquerading solitary plasmacytoma in an immunocompetent patient. BMJ Case Rep. 2018;2018:bcr-2018-225374.
Moramarco A, Marenco M, La Cava M, Lambiase A. Radiological-pathological correlation in plasmablastic lymphoma in an immunocompromised patient. Case Rep Ophthalmol Med. 2018;2018:4746050.
Bouchla A, Papageorgiou SG, Tsakiraki Z, Glezou E, Pavlidis G, Stavroulaki G, et al. Plasmablastic lymphoma in an immunocompetent patient with MDS/MPN with ring sideroblasts and thrombocytosis-a case report. Case Rep Hematol. 2018;2018:2525070.
Pérez-Mendoza A, Zárate-Guzmán AM, Lázaro-Pacheco IB, Navarrete-Pérez JJ. Plasmablastic lymphoma of the rectum, a rare cause of lower gastrointestinal bleeding: a case report. Rev Gastroenterol Mex. 2019;84:519–20.
Rhoades R, Gong J, Palmisiano N, Alpdogan O. Primary central nervous system plasmablastic lymphoma in an HIV-positive patient. BMJ Case Rep. 2019;12:e226755.
Sharma P, Sreedharanunni S, Koshy A, Prakash G, Sachdeva M, Malhotra P. Plasmablastic lymphoma of bone marrow: report of a rare case and immunohistochemistry based approach to the diagnosis. Indian J Pathol Microbiol. 2019;62:107–10.
Kessler AJ, Marcellino BK, Niglio SA, Petersen BE, Malone AK. A rare presentation of HIV-negative plasmablastic lymphoma: a diagnostic dilemma. Case Rep Hematol. 2019;2019:2907317.
Pudzeis J, Henrard C, Meurisse N. Intestinal intussusception in adults, atypical and potentially dramatic. Rev Med Liege. 2019;74:68–70.
Shin OR, Hyeon J, Kang SB, Kim JO. Plasmablastic lymphoma presenting with ileocecal intussusception in an immunocompetent patient. Korean J Intern Med. 2020;35(4):1018–9.
Yamada T, Hara T, Goto N, Iwata H, Tsurumi H. Follicular lymphoma suggested to transform into EBV-negative plasmablastic lymphoma. Int J Hematol. 2019;109:723–30.
Mohd I, Gajbhiye SS, Verma R, Sardhara J. Solitary primary central nervous system plasmablastic lymphoma in a young immunocompetent female: report on an extremely rare entity with review of literature. Asian J Neurosurg. 2019;14:541–6.
Roberts SJ, McNally B, Rosser JA, Willard N, Golitz L, Wisell J. Diverse clinical and histopathologic features of cutaneous post-transplant lymphoproliferative disorders: a presentation of two cases. Australas J Dermatol. 2019;60:e317–21.
Franchin M, Amaglio C, Cervarolo MC, Piffaretti G, Uccella S, Iovino D, et al. Plasmablastic lymphoma presenting as a brachial artery aneurysm associated with haemodialysis arteriovenous access ligation in a renal transplant patient. J Vasc Access. 2020;21:120–4.
Damlaj M, Alzayed M, Alahmari B, Alhejazi A, Alaskar A, Alzahrani M. Therapeutic potential of checkpoint inhibitors in refractory plasmablastic lymphoma. Clin Lymphoma Myeloma Leuk. 2019;19:e559–63.
Geethakumari PR, Markantonis J, Shah JL, Alsuwaidan A, Shahab I, Chen W, et al. Breast implant-associated plasmablastic lymphoma: a case report and discussion of the literature. Clin Lymphoma Myeloma Leuk. 2019;19:e568–72.
Moazez C, Amar S. A unique case of testicular plasmablastic lymphoma in a patient with human immunodeficiency virus. Cureus. 2019;11:e4839.
Shetty D, Shetty P, Dinkar C. Plasmablastic lymphoma in the paranasal sinus in a HIV positive patient: a rare entity. Malta Med J. 2019;31:39–43.
Bindra BS, Ramineni G, Sattar Y, Khillan R. CD-20 negative plasmablastic lymphoma lurking in the shadow of a leiomyoma—diagnosis and management. Cureus. 2019;11:e5217.
Karataş S, Çift T, Şal V, Tekelioğlu M, Ton Ö. Unusual uterine metastasis of plasmablastic lenfoma: a case report. Eur Res J. 2019;5:1020–3.
Umeanaeto O, Gamboa J, Diaz J, Nawar Hakim M, Corral J, Philipovskiy A, et al. Incorporating bortezomib in the management of plasmablastic lymphoma. Anticancer Res. 2019;39:5003–7.
Yordanova K, Stilgenbauer S, Bohle RM, Lesan V, Thurner L, Kaddu-Mulindwa D, et al. Spontaneous regression of a plasmablastic lymphoma with MYC rearrangement. Br J Haematol. 2019;186:e203–7.
Scott JH, Bains APS, Lindsay TD, Zhao X, Bromberg ME. Severe type B lactic acidosis in a rare and aggressive HIV-related lymphoma. Case Rep Crit Care. 2019;2019:4642925.
Atallah-Yunes SA, Murphy D, Abdelmalak R, Mantle L, Ali SS. Plasmablastic lymphoma achieving sustained remission with antiretroviral therapy alone. Eur J Haematol. 2019;103:620–2.
Perkins JN, Chi AW, Patel NJ. Plasmablastic lymphoma of the nasal septum. JAMA Otolaryngol Head Neck Surg. 2019;145:868.
Rodrigues AI, Cabeçadas J, Martins Fernandes R, Viana Coelho M, Sousa C. Plasmablastic lymphoma of the maxillary sinus. Intern Emerg Med. 2019;14:1337–8.
Al Shaarani M, Shackelford RE, Master SR, Mills GM, AlZubaidi Y, Mamilly A, et al. Plasmablastic lymphoma, a rare entity in bone marrow with unusual immunophenotype and challenging differential diagnosis. Case Rep Hematol. 2019;2019:1586328.
Bots EMT, Opperman J, Bassa F, Koegelenberg CFN. An endotracheal plasmablastic lymphoma. Respiration. 2019;98:546–50.
Chen N, Perez M, Mims M. Epstein-Barr virus primary infection complicated by hemophagocytic lymphohistiocytosis and plasmablastic lymphoma in a HIV-negative patient. Case Rep Hematol. 2019;2019:7962485.
Valenzuela J, Yeaney GA, Hsi ED, Azzato EM, Peereboom DM, Singh AD. Large B-cell lymphoma of the uvea: histopathologic variants and clinicopathologic correlation. Surv Ophthalmol. 2020;65:361–70.
Ando K, Imaizumi Y, Kobayashi Y, Niino D, Hourai M, Sato S, et al. Bortezomib- and lenalidomide-based treatment of refractory plasmablastic lymphoma. Oncol Res Treat. 2020;43:112–6.
Raychaudhuri R, Qualtieri J, Garfall AL. Axicabtagene ciloleucel for CD19+ plasmablastic lymphoma. Am J Hematol. 2020;95:E28-e30.
Abdulla HM, Cohn S. AIDS-associated esophageal plasmablastic lymphoma. Clin Gastroenterol Hepatol. 2021;19:A18.
Deshmukh R, Abhyankar P, Mhapuskar A, Varpe H. Intraoral plasmablastic lymphoma as a primary oral manifestation: a case report and review of literature. J Oral Maxillofac Pathol. 2020;24:S91–6.
Gasljevic G, Grat M, Kloboves Prevodnik V, Grcar Kuzmanov B, Gazic B, Lovrecic L, et al. Chronic lymphocytic leukemia with divergent Richter’s transformation into a clonally related classical Hodgkin’s and plasmablastic lymphoma: a case report. Case Rep Oncol. 2020;13:120–9.
Scott BL, Dominguez AR, Nguyen KD. Violaceous nodules in an HIV-positive man. Dermatol Online J. 2020. https://doi.org/10.5070/D3262047421.
Chikeka I, Grossman M, Deng C, Jacob AT, Husain S. Plasmablastic lymphoma in an HIV patient with cutaneous presentation: a case of remarkable remission in a typically refractory disease. JAAD Case Rep. 2020;6:161–5.
Debord C, Bourcier J, Subiger F, Leclair F, Touzeau C, Gastinne T, et al. Fluctuating plasmacytosis in an immunocompetent woman leading a diagnosis of plasmablastic lymphoma. Ann Hematol. 2020. https://doi.org/10.1007/s00277-020-03989-5.
Chee ARY, Ng TF, Lam SJP, Wright M, Leahy MF. An unusual case of plasmablastic lymphoma presenting as dermatomyositis. Clin Case Rep. 2020. https://doi.org/10.1002/ccr3.2787.
Costello CM, Maly CJ, Snider S, Severson KJ, DiCaudo DJ, Rosenthal AC, et al. Immunosuppression-associated primary cutaneous plasmablastic lymphoma secondary to romidepsin. JAAD Case Rep. 2020;6:19–22.
Agarwal P, Nigam AS, Kumar V, Marwah S, Singh P. Plasmablastic light chain myeloma presenting as pancytopenia: an unusual presentation. Natl Med J India. 2017;30:266–7.
Kumar S, Bhutani N, Bhargawa S, Kataria SP, Sen R. Extra-skeletal plasmablastic myeloma presenting as palatal growth—an unusual entity. Int J Surg Case Rep. 2017;41:423–6.
Majhi U, Sundersingh S, Murhekar K, Radha K. Extramedullary sarcomatoid variant of plasmablastic plasmacytoma. J Cancer Res Ther. 2017;13:1078–9.
Morris RW, Kumar V, Saad AG. Anaplastic plasmacytoma: a rare tumor presenting as a pathological fracture in a younger adult. Skeletal Radiol. 2018;47:995–1001.
Chang ST, Hsieh YC, Kuo CC, Chuang SS. Colonic CD30 positive plasmablastic plasmacytoma masquerading as anaplastic large cell lymphoma. Pathology. 2018;50:668–70.
Saburi M, Ogata M, Itani K, Kohno K, Soga Y, Kondo Y, et al. Rare concurrent indolent B-cell lymphoma and plasmablastic transformation of myeloma. J Clin Exp Hematop. 2018;58:175–9.
Ding W, Tan Y, Qian Y, Xue W, Wang Y, Xi C, et al. Primary plasmablastic plasmacytoma in the stomach of an immunocompetent adult: a case report. Medicine (Baltimore). 2019;98:e14235.
Habermehl GK, Chesser JD, Theil KS, Rogers HJ. Very unusual expression of multiple aberrant T-cell markers in plasmablastic plasma cell myeloma. Int J Lab Hematol. 2019;41:e89–91.
Bansal D, Singh N, Agrawal N, Mehta A. Plasmablastic lymphoma versus EBV-positive myeloma. Indian J Hematol Blood Transfus. 2019;35:567–9.
Iosif E, Rees C, Beeslaar S, Shamali A, Lauro R, Kyriakides C. Gastrointestinal bleeding as initial presentation of extramedullary plasma cell neoplasms: a case report and review of the literature. World J Gastrointest Endosc. 2019;11:308–21.
Varricchio S, Pagliuca F, Travaglino A, Gallo L, Villa MR, Mascolo M. Cutaneous localization of plasmablastic multiple myeloma with heterotopic expression of CD3 and CD4: skin involvement revealing systemic disease. J Cutan Pathol. 2019;46:619–22.
Chung A, Liedtke M. Cutaneous plasmablastic plasmacytoma. Blood. 2019;134:2116.
Arter ZL, Miles D, Mignano S, Cordaro D, Roswarski J. Plasmablastic IgM multiple myeloma with hypocellular bone marrow. Ann Hematol. 2020;99:895–6.
Suarez-Londono JA, Rohatgi A, Antoine-Pepeljugoski C, Braunstein MJ. Aggressive presentation of plasmablastic myeloma. BMJ Case Rep. 2020;13:e234436.
Yoshihara K, Yoshihara S, Matsuda I, Imado T, Matsuo S, Okada M, et al. Treatment strategy in a patient showing borderline features between plasmablastic lymphoma and plasmablastic myeloma harboring a 17p deletion. Ann Hematol. 2020;99:1405–7.
Yang W, Zhang X-J, Wang H-C, Yang G-Y, Xu X-F. IgD-λ multiple myeloma accompanying with elevated AFP level: a case report and literature review. Int J Clin Exp Med. 2018;11:5176–80.
Tymon-Rosario JR, Shi Y, DiVito J, Aksel SO, Gressel GM. Blastic variant of plasma cell myeloma mimicking squamous cell carcinoma of the uterine cervix in a super-morbidly obese female. Gynecol Oncol Rep. 2019;29:34–7.
Dittus C, Grover N, Ellsworth S, Tan X, Park SI. Bortezomib in combination with dose-adjusted EPOCH (etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin) induces long-term survival in patients with plasmablastic lymphoma: a retrospective analysis. Leuk Lymphoma. 2018;59:2121–7.
Pan Z, Chen M, Zhang Q, Wang E, Yin L, Xu Y, et al. CD3-positive plasmablastic B-cell neoplasms: a diagnostic pitfall. Mod Pathol. 2018;31:718–31.
Gravelle P, Péricart S, Tosolini M, Fabiani B, Coppo P, Amara N, et al. EBV infection determines the immune hallmarks of plasmablastic lymphoma. Oncoimmunology. 2018;7:e1486950.
Tabata R, Tabata C, Uesugi H, Takei Y. Highly aggressive plasmablastic neoplasms in patients with rheumatoid arthritis treated with methotrexate. Int Immunopharmacol. 2019;68:213–7.
Bhattacharyya S, Bains APS, Sykes DL, Iverson BR, Sibgatullah R, Kuklani RM. Lymphoid neoplasms of the oral cavity with plasmablastic morphology-a case series and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019;128:651–9.
Liu Y, Jelloul F, Zhang Y, Bhavsar T, Ho C, Rao M, et al. Genetic basis of extramedullary plasmablastic transformation of multiple myeloma. Am J Surg Pathol. 2020. https://doi.org/10.1097/PAS.0000000000001459.
Li YJ, Li JW, Chen KL, Li J, Zhong MZ, Liu XL, et al. HIV-negative plasmablastic lymphoma: report of 8 cases and a comprehensive review of 394 published cases. Blood Res. 2020;55:49–56.
Garcia-Reyero J, Martinez Magunacelaya N, Gonzalez de Villambrosia S, Loghavi S, Gomez Mediavilla A, Tonda R, et al. Genetic lesions in MYC and STAT3 drive oncogenic transcription factor overexpression in plasmablastic lymphoma. Haematologica. 2021;106:1120–8.
Al Tabaa Y, Tchernonog E, Faurie P, Cottereau AS, Monjanel H, Bonnet A, et al. Post-treatment positron emission tomography-computed tomography is highly predictive of outcome in Plasmablastic lymphoma. Eur J Nucl Med Mol Imaging. 2018;45:1705–9.
Ambrosio MR, Mundo L, Gazaneo S, Picciolini M, Vara PS, Sayed S, et al. MicroRNAs sequencing unveils distinct molecular subgroups of plasmablastic lymphoma. Oncotarget. 2017;8:107356–73.
Arora N, Eule C, Gupta A, Li HC, Sadeghi N. Clinicopathologic features, management, and outcomes of plasmablastic lymphoma: a 10-year experience. Am J Hematol. 2019;94:E127–9.
Castillo JJ, Guerrero-Garcia T, Baldini F, Tchernonog E, Cartron G, Ninkovic S, et al. Bortezomib plus EPOCH is effective as frontline treatment in patients with plasmablastic lymphoma. Br J Haematol. 2019;184:679–82.
Chen L, Zhang JS, Liu DG, Cui D, Meng ZL. An algorithmic approach to diagnose haematolymphoid neoplasms in effusion by combining morphology, immunohistochemistry and molecular cytogenetics. Cytopathology. 2018;29:10–21.
Deng XZ, Li WH, Wang YL. Plasmablastic lymphoma combined with gastric cancer: report of one case and review of literature. J Leukemia Lymphoma. 2017;26:287–9.
Fan Z, Li J, Yi P, Li K, Li J, Zhou Q, et al. Case report on 5 plasmablastic lymphoma patients and literature review by retrospective analysis. Anti-Tumor Pharm. 2018;8:124–8.
Feng J, Xu L, Dong H-J, Zhang N, Bai Q-X, Liang R, et al. Clinicopathological characteristics and prognosis analysis of the patients with plasmablastic lymphoma. Zhongguo Shi Yan Xue Ye Xue Za Zhi. 2018;26:1350–4.
Focà E, Cavaglià G, Rusconi S, Cascavilla A, Cenderello G, Re A, et al. Survival in HIV-infected patients with lymphoma according to the choice of antiretroviral treatment: an observational multicentre study. HIV Med. 2018. https://doi.org/10.1111/hiv.12624.
Huang TX, Fu HY, Chen Y, Liu TB. Anaplastic plasmacytoma: report of one case and review of literature. J Leukemia Lymphoma. 2018;27:183–6.
Hübel K, Re A, Boumendil A, Finel H, Hentrich M, Robinson S, et al. Autologous stem cell transplantation for HIV-associated lymphoma in the antiretroviral and rituximab era: a retrospective study by the EBMT Lymphoma Working Party. Bone Marrow Transplant. 2019;54:1625–31.
Kusuke N, Custódio M, de Sousa S. Oral lesion as the primary diagnosis of non-Hodgkin’s lymphoma: a 20-year experience from an oral pathology service and review of the literature. Eur Arch Otorhinolaryngol. 2019;276:2873–9.
Meer S, Perner Y, McAlpine ED, Willem P. Extraoral plasmablastic lymphomas in a high human immunodeficiency virus endemic area. Histopathology. 2020;76:212–21.
Miao L, Guo N, Feng Y, Rao H, Wang F, Huang Q, et al. High incidence of MYC rearrangement in human immunodeficiency virus-positive plasmablastic lymphoma. Histopathology. 2020;76:201–11.
Montes-Moreno S, Martinez-Magunacelaya N, Zecchini-Barrese T, De Villambrosía SG, Linares E, Ranchal T, et al. Plasmablastic lymphoma phenotype is determined by genetic alterations in MYC and PRDM1. Mod Pathol. 2017;30:85–94.
Mpunga T, Znaor A, Uwizeye FR, Uwase A, Munyanshongore C, Franceschi S, et al. A case-control study of HIV infection and cancer in the era of antiretroviral therapy in Rwanda. Int J Cancer. 2018;143:1348–55.
Phipps C, Yeoh KW, Lee YS, Nagarajan C, Gopalakrishnan S, Ho LP, et al. Durable remission is achievable with localized treatment and reduction of immunosuppression in limited stage EBV-related plasmablastic lymphoma. Ann Hematol. 2017;96:1959–60.
Qunaj L, Castillo JJ, Olszewski AJ. Survival of patients with CD20-negative variants of large B-cell lymphoma: an analysis of the National Cancer Data Base. Leuk Lymphoma. 2018;59:1375–83.
Ramos JC, Sparano J, Moore PC, Siegel E, Lee JY, Reid EG, et al. A randomized trial of EPOCH-based chemotherapy with vorinostat for highly aggressive HIV-associated lymphomas: updated results evaluating impact of diagnosis-to-treatment interval (DTI) and Pre-Protocol systemic therapy on outcomes. Blood. 2019;134:1588.
Ramos JC, Sparano JA, Moore PC, Cesarman E, Reid EG, Rubinstein PG, et al. AMC075: a randomized phase II trial of vorinostat with R-EPOCH in aggressive HIVrelated NHL. J Clin Oncol. 2018;36:7573.
Rudresha AH, Khandare PA, Lokanatha D, Linu AJ, Suresh Babu MC, Lokesh KN, et al. HIV/AIDS-related lymphoma: perspective from a regional cancer center in India. Blood Res. 2019;54:181–8.
Sampath R, Manipadam M, Nair S, Viswabandya A, Zachariah A. HIV-associated lymphoma: a 5-year clinicopathologic study from India. Indian J Pathol Microbiol. 2019;62:73–8.
Singh BM, Belurkar S, Bishnu A, Shetty T, Pavithra P. Primary central nervous system effusion plasmablastic lymphoma in immunocompromised patient: A rare phenomenon. Asian J Pharm Clin Res. 2018;11:6–7.
Weber V, Helling K. Matthias C [HIV-associated plasmablastic lymphoma of the paranasal sinuses : an incidental finding]. HNO. 2018;66:144–7.
Zuze T, Ellis GK, Kasonkanji E, Kaimila B, Nyasosela R, Nyirenda R, et al. Modified EPOCH for high-risk non-Hodgkin lymphoma in sub-Saharan Africa. Cancer Med. 2020;9:77–83.
Zuze T, Painschab MS, Seguin R, Kudowa E, Kaimila B, Kasonkanji E, et al. Plasmablastic lymphoma in Malawi. Infect Agent Cancer. 2018;13:22.
Hwang J, Suh CH, Won Kim K, Kim HS, Armand P, Huang RY, et al. The incidence of Epstein-Barr virus-positive diffuse large B-cell lymphoma: a systematic review and meta-analysis. Cancers (Basel). 2021;13:1785.
Chang ST, Liao YL, Lu CL, Chuang SS, Li CY. Plasmablastic cytomorphologic features in plasma cell neoplasms in immunocompetent patients are significantly associated with EBV. Am J Clin Pathol. 2007;128:339–44.
Yan J, Wang J, Zhang W, Chen M, Chen J, Liu W. Solitary plasmacytoma associated with Epstein-Barr virus: a clinicopathologic, cytogenetic study and literature review. Ann Diagn Pathol. 2017;27:1–6.
Alexandrakis MG, Passam FH, Kyriakou DS, Dambaki K, Niniraki M, Stathopoulos E. Ki-67 proliferation index: correlation with prognostic parameters and outcome in multiple myeloma. Am J Clin Oncol. 2004;27:8–13.
Gastinne T, Leleu X, Duhamel A, Moreau AS, Franck G, Andrieux J, et al. Plasma cell growth fraction using Ki-67 antigen expression identifies a subgroup of multiple myeloma patients displaying short survival within the ISS stage I. Eur J Haematol. 2007;79:297–304.
Firsova MV, Mendeleeva LP, Kovrigina AM, Solovev MV, Savchenko VG. Plasmacytoma in patients with multiple myeloma: morphology and immunohistochemistry. BMC Cancer. 2020;20:346.
Lu TX, Liang JH, Miao Y, Fan L, Wang L, Qu XY, et al. Epstein-Barr virus positive diffuse large B-cell lymphoma predict poor outcome, regardless of the age. Sci Rep. 2015;5:12168.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology B-Cell Lymphomas. Version 4.2021. Accessed 2021 Jul 28
Greipp PR, Raymond NM, Kyle RA, O’Fallon WM. Multiple myeloma: significance of plasmablastic subtype in morphological classification. Blood. 1985;65:305–10.
Morscio J, Dierickx D, Nijs J, Verhoef G, Bittoun E, Vanoeteren X, et al. Clinicopathologic comparison of plasmablastic lymphoma in HIV-positive, immunocompetent, and posttransplant patients: single-center series of 25 cases and meta-analysis of 277 reported cases. Am J Surg Pathol. 2014;38:875–86.
Palumbo A, Avet-Loiseau H, Oliva S, Lokhorst HM, Goldschmidt H, Rosinol L, et al. Revised international staging system for multiple myeloma: a report from international myeloma working group. J Clin Oncol. 2015;33:2863–9.
Kim JE, Kim YA, Kim WY, Kim CW, Ko YH, Lee GK, et al. Human immunodeficiency virus-negative plasmablastic lymphoma in Korea. Leuk Lymphoma. 2009;50:582–7.
Hagiwara S, Nagai H, Tanaka J, Okada S. The current state of human immunodeficiency virus-associated lymphoma in Japan: a nationwide retrospective study of the Japanese Society of Hematology Blood Disease Registry. Int J Hematol. 2019;110:244–9.
Tchernonog E, Faurie P, Coppo P, Monjanel H, Bonnet A, Algarte Génin M, et al. Clinical characteristics and prognostic factors of plasmablastic lymphoma patients: analysis of 135 patients from the LYSA group. Ann Oncol. 2017;28:843–8.
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
12185_2021_3211_MOESM1_ESM.tif
Supplemental Figure 1 Our diagnostic algorithm. PBL plasmablastic lymphoma, PBM plasmablastic myeloma, PBN plasmablastic neoplasm, + positive, - negative (TIF 2239 KB)
12185_2021_3211_MOESM2_ESM.tif
Supplemental Figures 2 Ahn’s diagnostic algorithm. PBL plasmablastic lymphoma, PBM plasmablastic myeloma, myeloma-defining signs of hypercalcemia, renal disease, and anemia, and bone lesions, EBER Epstein-Barr virus-encoded small RNA, + positive, - negative (TIF 2711 KB)
12185_2021_3211_MOESM3_ESM.tif
Supplemental Figures 3 Chen’s diagnostic algorithm. PBL plasmablastic lymphoma, PBM plasmablastic myeloma, BM bone marrow, PC plasma cells, CRAB hypercalcemia, renal failure, anemia, and lytic bone lesions, EBER Epstein–Barr virus-encoded small RNA, + positive, - negative (TIF 1708 KB)
About this article
Cite this article
Mori, H., Fukatsu, M., Ohkawara, H. et al. Heterogeneity in the diagnosis of plasmablastic lymphoma, plasmablastic myeloma, and plasmablastic neoplasm: a scoping review. Int J Hematol 114, 639–652 (2021). https://doi.org/10.1007/s12185-021-03211-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-021-03211-w