Abstract
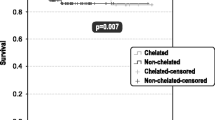
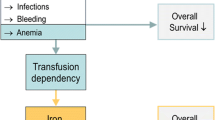
Acquired aplastic anemia (AA) is the most common condition linked to transfusion dependence. We conducted a cohort study to explore patterns of the dynamic evolution of iron burden, and to identify the risk factors for iron overload (IO) in 550 AA patients. Of the participants, 13 % presented with IO when diagnosed, including 7 % of patients without a history of transfusion and 22 % of those receiving transfusions. Male patients [hazard ratio (HR) = 3.85, 95 % confidence interval (CI) 1.77–8.36], adults (HR = 3.04, 95 % CI 1.21–7.63), and patients with high transfusion burdens (more than eight units; HR = 11.30, 95 % CI 4.45–28.70) experienced a significantly higher risk of IO. Furthermore, we found a sharply increasing risk of IO within the first 2 years, especially in males, patients with large number of lifetime transfusions, and patients not responding to treatment. More interestingly, after transfusion independence, a significant seesaw effect between erythropoiesis and iron burden was not noted until 6 months later, which continued over 3 years. In contrast to female patients, children, and patients with lower transfusion burdens, male subjects, adults, and subjects with high transfusion burdens experienced a pattern of slow decline in iron burden. AA incurred a high risk of progression to IO and showed distinct patterns in the evolution of iron burden. In light of these data, we offer suggestions for decision-making regarding who should undergo iron chelation and when.





Similar content being viewed by others
References
Yong NS. Current concepts in the pathophysiology and treatment of aplastic anemia. Hematology Am Soc Hematol Educ Program. 2013;2013:76–81.
Scheinberg P, Young NS. How I treat acquired aplastic anemia. Blood. 2012;120:1185–96.
Marsh JC, Ball SE, Cavenagh J, Darbyshire P, Dokal I, Gordon-Smith EC, British Committee for Standards in Hematology, et al. Guidelines for the diagnosis and management of aplastic anemia. Br J Haematol. 2009;147:43–70.
Brittenham GM. Iron-chelating therapy for transfusional iron overload. N Eng J Med. 2011;364:146–56.
Holffbrand AV, Taher A, Cappellini MD. How I treat transfusional iron overload. Blood. 2012;120:3657–69.
Malcovati L, Porta MG, Pascutto C, Invernizzi R, Boni M, Travaglino E, et al. Prognostic factors and life expectancy in myelodysplastic syndromes classified according to WHO criteria: a basis for clinical decision making. J Clin Oncol. 2005;23:7594–603.
Jabbour E, Kantarjian HM, Koller C, Taher A. Red blood cell transfusions and iron overload in the treatment of patients with myelodysplastic syndromes. Cancer. 2008;112:1089–95.
Delea TE, Hagiwara M, Phatak PD. Retrospective study of the association between transfusion frequency and potential complications of iron overload in patients with myelodysplastic syndrome and other acquired hematopoietic disorders. Curr Med Res Opin. 2009;25:139–47.
Remacha AF, Arrizabalaga B, Del Cañizo C, Sanz G, Villegas A. Iron overload and chelation therapy in patients with low-risk myelodysplastic syndromes with transfusion requirements. Ann Hematol. 2010;89:147–54.
Adams RL, Bird RJ. Safety and efficacy of deferasirox in the management of transfusion-dependent patients with myelodysplastic syndrome and aplastic anemia: a perspective review. Ther Adv Hematol. 2013;4:93–102.
Butler A, Patton WN. Iron chelation therapy in myelodysplastic syndromes: we need more evidence, not more guidelines. Intern Med J. 2012;42:481–4.
Camitta BM, Thomas ED, Nathan DG, Gale RP, Kopecky KJ, Rappeport JM, et al. A prospective study of androgens and bone marrow transplantation for treatment of severe aplastic anemia. Blood. 1979;53:504–14.
Lee JW, Yoon SS, Shen ZX, Ganser A, Hsu HC, Habr D, EPIC study investigators, et al. Iron chelation therapy with deferasirox in patients with aplastic anemia: a subgroup analysis of 116 patients from the EPIC trial. Blood. 2010;116:2448–54.
Li X, Shi J, Ge M, Shao Y, Huang J, Huang Z, et al. Outcomes of optimized over standard protocol of rabbit antithymocyte globulin for severe aplastic anemia: a single-center experience. PLoS One. 2013;8:e56648.
Zheng Y, Liu Y, Chu Y. Immunosuppressive therapy for acquired severe aplastic anemia (SAA): a prospective comparison of four different regimens. Exp Hematol. 2006;34:826–31.
Li X, Shao Y, Ge M, Shi J, Huang J, Huang Z, et al. A promising immunosuppressive strategy of cyclosporine alternately combined with levamisole is highly effective for moderate aplastic anemia. Ann Hematol. 2013;92:1239–47.
Fleming RE, Ponka P. Iron overload in human disease. N Engl J Med. 2012;366:348–59.
Pullarkat V. Objectives of iron chelation therapy in myelodysplastic syndromes: more than meets the eye? Blood. 2009;114:5251–5.
Speeckaert MM, Speeckaert R, Delanghe JR. Biological and clinical aspects of soluble transferrin receptor. Crit Rev Clin Lab Sci. 2010;47:213–28.
Skikne BS. Serum transferrin receptor. Am J Hematol. 2008;83:872–5.
Takatoku M, Uchiyama T, Okamoto S, Kanakura Y, Sawada K, Tomonaga M, et al. Japanese National Research Group on idiopathic bone marrow failure syndromes. Retrospective nationwide survey of Japanese patients with transfusion-dependent MDS and aplastic anemia highlights the negative impact of iron overload on morbidity/mortality. Eur J Haematol. 2007;78:487–94.
Ashida T, Kawano A, Yamada E, Ide D, Sugano C, Kato Y, et al. Relationship between red blood cell transfusion volume and posttransfusional iron overload in hematological diseases. Rinsho Ketsueki. 2013;54:365–9.
Lee JW. Iron chelation therapy in myelodysplastic syndromes and aplastic anemia: a review of experience in South Korea. Int J Hematol. 2008;88:16–23.
Acknowledgments
The authors acknowledge all of the doctors and nurses at the Therapeutic Centre for Anemic Diseases and the team of researchers at the Clinical Laboratory Centre for their professional assistance. This work was supported by grants from the National Natural Science Foundation of China (No. 81370606, No. 81300388), the Peking Union Medical College Youth Fund (No. 3332013153).
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
P. Jin and J. Wang contributed equally in this study and should be considered co-first authors.
About this article
Cite this article
Jin, P., Wang, J., Li, X. et al. Evolution of iron burden in acquired aplastic anemia: a cohort study of more than 3-year follow-up. Int J Hematol 101, 13–22 (2015). https://doi.org/10.1007/s12185-014-1708-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-014-1708-6