Abstract
Purpose of Review
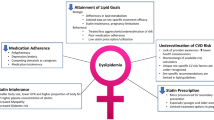
As the adverse impact of cardiovascular disease continues to afflict women around the world, the identification and treatment of risk factors to reduce cardiovascular morbidity and mortality continue to rise in priority. Dyslipidemia is a significant risk factor for coronary heart disease and should serve as a strong focus point in both primary and secondary prevention. However, women remain undertreated compared with men and receive less evidence-based therapies including cholesterol management. Some of the unique risk factors in women that contribute to cardiovascular disease have been incorporated in the current cholesterol management guidelines.
Recent Findings
The medical community and international organizations have helped reduce the annual cardiovascular mortality rates for women since 1984. However, more work remains to be completed as heart disease in women remains inadequately researched, underdiagnosed, and poorly managed. This review discusses contemporary management of dyslipidemia in women, with additional focus on special risk subgroups and integration of the new 2018 American Heart Association/American College of Cardiology Guidelines on the Management of Blood Cholesterol.
Summary
Dyslipidemia management in women constitutes a substantial portion of the foundation of both primary and secondary prevention and is essential to reducing cardiovascular events in women. The current cholesterol guidelines focus on some of the risk factors for cardiovascular disease that are unique or more common in women. This is a review of how the current cholesterol management guidelines pertain to women specifically and address sex-specific cardiovascular risk factors in women.


Similar content being viewed by others
Abbreviations
- ACC:
-
American College of Cardiology
- AHA:
-
American Heart Association
- ASCVD:
-
Atherosclerotic cardiovascular disease
- CHD:
-
Coronary heart disease
- CV:
-
Cardiovascular
- CVD:
-
Cardiovascular disease
- FH:
-
Familial hypercholesterolemia
- HDL-C:
-
High-density lipoprotein cholesterol
- HIV:
-
Human immunodeficiency virus
- LDL-C:
-
Low-density lipoprotein cholesterol
- Lp(a):
-
Lipoprotein(a)
- MetS:
-
Metabolic syndrome
- MI:
-
Myocardial infarction
- Non-HDL:
-
Non-high-density lipoprotein
- PAG:
-
Physical activity guidelines
- RA:
-
Rheumatoid arthritis
- SLE:
-
Systemic lupus erythematosus
- TG:
-
Triglyceride
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937–52.
Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63(25 Pt B):2985–3023.
Overweight & obesity: centers of disease control and prevention; 2018 [updated October 30, 2018. Available from: https://www.cdc.gov/obesity/data/prevalence-maps.html. Accessed 15 May 2019.
Eckel RH, Jakicic JM, Ard JD, de Jesus JM, Houston Miller N, Hubbard VS, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S76–99.
Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The physical activity guidelines for Americans. JAMA. 2018;320(19):2020–8.
•• Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018, 2018. https://doi.org/10.1016/j.jacc.2018.11.003. The 2018 ACC/AHA cholesterol guidelines, updated from the 2013 guidelines, relay recommendations on the clinical management of patients with elevated cholesterol levels. Algorithms for primary and secondary prevention are presented to assist with risk stratification of patients and prescription of cholesterol-reducing agents. Other new concepts include the use of coronary artery calcium scoring in patients of uncertain cardiovascular risk and the addition of PCSK-9 inhibitors to further reduce LDL levels in very high-risk patients.
Chiavaroli L, Nishi SK, Khan TA, Braunstein CR, Glenn AJ, Mejia SB, et al. Portfolio dietary pattern and cardiovascular disease: a systematic review and meta-analysis of controlled trials. Prog Cardiovasc Dis. 2018;61(1):43–53.
Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S1–45.
Long-Term Intervention with Pravastatin in Ischaemic Disease Study G. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med. 1998;339(19):1349–57.
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322.
Mehta LS, Beckie TM, DeVon HA, Grines CL, Krumholz HM, Johnson MN, et al. Acute myocardial infarction in women: a scientific statement from the American Heart Association. Circulation. 2016;133(9):916–47.
Hsue PY, Bittner VA, Betteridge J, Fayyad R, Laskey R, Wenger NK, et al. Impact of female sex on lipid lowering, clinical outcomes, and adverse effects in atorvastatin trials. Am J Cardiol. 2015;115(4):447–53.
Crilly M, Bundred P, Hu X, Leckey L, Johnstone F. Gender differences in the clinical management of patients with angina pectoris: a cross-sectional survey in primary care. BMC Health Serv Res. 2007;7:142.
Zhao M, Vaartjes I, Graham I, Grobbee D, Spiering W, Klipstein-Grobusch K, et al. Sex differences in risk factor management of coronary heart disease across three regions. Heart. 2017;103(20):1587–94.
Lichtman JH, Leifheit EC, Safdar B, Bao H, Krumholz HM, Lorenze NP, et al. Sex differences in the presentation and perception of symptoms among young patients with myocardial infarction: evidence from the VIRGO study (variation in recovery: role of gender on outcomes of young AMI patients). Circulation. 2018;137(8):781–90.
Lee PY, Alexander KP, Hammill BG, Pasquali SK, Peterson ED. Representation of elderly persons and women in published randomized trials of acute coronary syndromes. JAMA. 2001;286(6):708–13.
Bairey Merz CN, Shaw LJ, Reis SE, Bittner V, Kelsey SF, Olson M, et al. Insights from the NHLBI-Sponsored Women’s Ischemia Syndrome Evaluation (WISE) Study: part II: gender differences in presentation, diagnosis, and outcome with regard to gender-based pathophysiology of atherosclerosis and macrovascular and microvascular coronary disease. J Am Coll Cardiol. 2006;47(3 Suppl):S21–9.
Martin EA, Tan SL, MacBride LR, Lavi S, Lerman LO, Lerman A. Sex differences in vascular and endothelial responses to acute mental stress. Clin Auton Res. 2008;18(6):339–45.
Humphries KH, Izadnegahdar M, Sedlak T, Saw J, Johnston N, Schenck-Gustafsson K, et al. Sex differences in cardiovascular disease - impact on care and outcomes. Front Neuroendocrinol. 2017;46:46–70.
Murphy E. Estrogen signaling and cardiovascular disease. Circ Res. 2011;109(6):687–96.
Taddei S, Virdis A, Ghiadoni L, Mattei P, Sudano I, Bernini G, et al. Menopause is associated with endothelial dysfunction in women. Hypertension. 1996;28(4):576–82.
Rosano GM, Vitale C, Marazzi G, Volterrani M. Menopause and cardiovascular disease: the evidence. Climacteric. 2007;10(Suppl 1):19–24.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol. 2018;72(18):2231–64.
Bhatt DL, Steg PG, Miller M, Brinton EA, Jacobson TA, Ketchum SB, et al. Cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia. N Engl J Med. 2019;380(1):11–22.
• Hyun KK, Redfern J, Patel A, Peiris D, Brieger D, Sullivan D, et al. Gender inequalities in cardiovascular risk factor assessment and management in primary healthcare. Heart. 2017;103(7):492–8 Given the current environment of high sensitivity troponin, the fourth update of the universal definition of myocardial infarction clarifies the difference between myocardial infarction and myocardial injury, and it discusses circumstances in which troponin levels may be increased from non-myocardial infarction phenomena. The established myocardial infarction classification system (types 1 through 5) is still used but updated.
Jensen J, Nilas L, Christiansen C. Influence of menopause on serum lipids and lipoproteins. Maturitas. 1990;12(4):321–31.
Shufelt CL, Bairey Merz CN. Contraceptive hormone use and cardiovascular disease. J Am Coll Cardiol. 2009;53(3):221–31.
•• Aggarwal NR, Patel HN, Mehta LS, Sanghani RM, Lundberg GP, Lewis SJ, et al. Sex differences in ischemic heart disease: advances, obstacles, and next steps. Circ Cardiovasc Qual Outcomes. 2018;11(2):e004437 Dr. Agarwal et al. present a comprehensive review of sex differences in the pathophysiology, presentation, and management of heart disease in women compared to men. The paper discussed social/gender-related and and sex-specific etiologies for the variability in heart disease presentations and outcomes between men and women. In addition, the authors offer solutions to several public health challenges, such as the red dress campaign to raise community awareness, implementation of dedicated women’s heart centers, and call for sex- and gender-specific guidelines.
Khera AV, Emdin CA, Drake I, Natarajan P, Bick AG, Cook NR, et al. Genetic risk, adherence to a healthy lifestyle, and coronary disease. N Engl J Med. 2016;375(24):2349–58.
Stampfer MJ, Hu FB, Manson JE, Rimm EB, Willett WC. Primary prevention of coronary heart disease in women through diet and lifestyle. N Engl J Med. 2000;343(1):16–22.
Goldberg AC, Hopkins PN, Toth PP, Ballantyne CM, Rader DJ, Robinson JG, et al. Familial hypercholesterolemia: screening, diagnosis and management of pediatric and adult patients: clinical guidance from the National Lipid Association Expert Panel on Familial Hypercholesterolemia. J Clin Lipidol. 2011;5(3 Suppl):S1–8.
Ouyang P, Michos ED, Karas RH. Hormone replacement therapy and the cardiovascular system lessons learned and unanswered questions. J Am Coll Cardiol. 2006;47(9):1741–53.
• Mosca L, Benjamin EJ, Berra K, Bezanson JL, Dolor RJ, Lloyd-Jones DM, et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women--2011 update: a guideline from the American Heart Association. J Am Coll Cardiol. 2011;57(12):1404–23 As an update from 2007, these 2011 guidelines on cardiovascular disease prevention in women strongly weigh the benefits of practices seen in the clinical setting to help make practical recommendations. The guidelines continue to use the risk classification algorithm adopted by the previous guidelines and discuss ethnic disparities and cost-effectiveness of recommended strategies, such as statins. They recommend against the use of hormone therapy or folic acid for cardiovascular prevention and elaborate on less commonly recognized risk factors in women, such as autoimmune disease and pregnancy related complications.
Tobias DK, Stuart JJ, Li S, Chavarro J, Rimm EB, Rich-Edwards J, et al. Association of history of gestational diabetes with long-term cardiovascular disease risk in a large prospective cohort of US women. JAMA Intern Med. 2017;177(12):1735–42.
Lekoubou A, Ovbiagele B, Markovic D, Sanossian N, Towfighi A. Age, sex, and race/ethnic temporal trends in metabolic syndrome prevalence among individuals with myocardial infarction or stroke in the United States. J Neurol Sci. 2017;376:24–8.
Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation. 2018;137(12):e67–e492.
Tsimikas S. A test in context: lipoprotein(a): diagnosis, prognosis, controversies, and emerging therapies. J Am Coll Cardiol. 2017;69(6):692–711.
Tsimikas S, Fazio S, Ferdinand KC, Ginsberg HN, Koschinsky ML, Marcovina SM, et al. NHLBI working group recommendations to reduce lipoprotein(a)-mediated risk of cardiovascular disease and aortic stenosis. J Am Coll Cardiol. 2018;71(2):177–92.
Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM Jr, Kastelein JJ, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359(21):2195–207.
Mason JC, Libby P. Cardiovascular disease in patients with chronic inflammation: mechanisms underlying premature cardiovascular events in rheumatologic conditions. Eur Heart J. 2015;36(8):482–9c.
Hanna DB, Ramaswamy C, Kaplan RC, Kizer JR, Anastos K, Daskalakis D, et al. Trends in cardiovascular disease mortality among persons with HIV in new York City, 2001-2012. Clin Infect Dis. 2016;63(8):1122–9.
Feinstein MJ, Nance RM, Drozd DR, Ning H, Delaney JA, Heckbert SR, et al. Assessing and refining myocardial infarction risk estimation among patients with human immunodeficiency virus: a study by the centers for AIDS research network of integrated clinical systems. JAMA Cardiol. 2017;2(2):155–62.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Lipids
Rights and permissions
About this article
Cite this article
Varghese, T., Lundberg, G. Lipids in Women: Management in Cardiovascular Disease Prevention and Special Subgroups. Curr Cardiovasc Risk Rep 13, 20 (2019). https://doi.org/10.1007/s12170-019-0615-z
Published:
DOI: https://doi.org/10.1007/s12170-019-0615-z