Abstract
Objectives
Early diagnosis of chemotherapy-induced cardiotoxicity plays an important role in preventing heart failure. The main aim of our study was to assess left ventricular (LV) dyssynchrony measured by phase analysis of gated single-photon emission computed tomography (SPECT) as an early sign of cardiotoxicity after breast cancer chemotherapy.
Methods
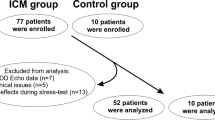
This cross-sectional study was conducted on patients with stage ≤ 3 breast cancer and no history of cardiovascular disease or diabetes. After mastectomy, the patients underwent rest gated SPECT myocardial perfusion imaging (MPI). Sixty patients with normal gated SPECT-MPI were selected and the imaging was performed after chemotherapy with doxorubicin, cyclophosphamide and paclitaxel. LV function and contractility parameters were extracted by QGS software and the results were compared with the t test method. The abnormality of at least one of the three phase analysis indices was considered as left ventricular dyssynchrony (LVD).
Results
The average LV end-systolic volume and ejection fraction (LVEF) before and after chemotherapy were (16.2 ± 8.0 ml and 21.6 ± 11.6 ml) and (73.4 ± 7.9% and 67.5 ± 9.2%) respectively, which showed a significant decrease (P < 0.05). In 2 patients (3.3%), the LVEF decreased to less than 50% after chemotherapy. The average parameters of left ventricular contractility before and after chemotherapy were, respectively, as follows: PHB (24.1 ± 7.5 and 33.8 ± 16.4), PSD (9.4 ± 6.1 and 5.7 ± 1.9) and entropy (28.9 ± 7.1 and 35.6 ± 9.7), which showed a significant increase (P < 0.05). LVD was observed in 14 patients (23.4%) after chemotherapy and prevalence of LVD was significantly higher in patients who had received a cumulative dose of doxorubicin of more than 400 mg/m2 (P = 0.005). There was no relationship between age and body mass index with the incidence of LVD after chemotherapy (P > 0.05).
Conclusion
Using phase analysis of gated SPECT-MPI, chemotherapy-induced LVD was seen in a significant number of patients with breast cancer, especially with a high cumulative dose of doxorubicin. LVD might indicate chemotherapy-induced cardiotoxicity before LVEF becomes abnormal.
Similar content being viewed by others
Data availability
Data is available on request from the corresponding author.
References
Huang J, Chan PS, Lok V, Chen X, Ding H, Jin Y, et al. Global incidence and mortality of breast cancer: a trend analysis. Aging (Albany NY). 2021;13(4):5748–803. https://doi.org/10.18632/aging.202502.
Kweon SS, Kim MG, Kang MR, Shin MH, Choi JS. Difference of stage at cancer diagnosis by socioeconomic status for four target cancers of the National Cancer Screening Program in Korea: Results from the Gwangju and Jeonnam cancer registries. J Epidemiol. 2017;27(7):299–304.
Denduluri N, Chavez-MacGregor M, Telli ML, Eisen A, Graff SL, Hassett MJ, et al. Selection of optimal adjuvant chemotherapy and targeted therapy for early breast cancer: ASCO clinical practice guideline focused update. J Clin Oncol. 2018;36(23):2433–43. https://doi.org/10.1200/JCO.2018.78.8604.
AlJaroudi WA, Hage FG. Review of cardiovascular imaging in the Journal of Nuclear Cardiology 2020: positron emission tomography, computed tomography, and magnetic resonance. J Nucl Cardiol. 2021;28:2100–11.
Fogarassy G, Fogarassyné Vathy Á, Kováts T, Hornyák L, Kenessey I, Veress G, et al. A doxorubicinkezeléshez kapcsolódó szívelégtelenség kialakulásának rizikótényezői a hazai országos adatbázisok integrált, retrospektív elemzése alapján [Analysing the risk factors of doxorubicin-associated heart failure by a retrospective study of integrated, nation-wide databases]. Orv Hetil. 2020;161(26):1094–102. https://doi.org/10.1556/650.2020.31739.
Lyon RA, Habibian M, Evertz R, Asteggiano R, Suter TM. Diagnosis and treatment of left ventricular dysfunction and heart failure in cancer patients. E-J Cardiol Practice. 2019;16(40):1–22.
Soujeri B, Singh J, Chew S, Hawkey S, Ferguson M, Lang CC. Surveillance and Incidence of Chemotherapy-Induced Cardiotoxicity in Breast Cancer: A Long Term Observational Study. Heart. 2016;102(suppl 6):A14–5.
Tajiri K, Aonuma K, Sekine I. Cardio-oncology: a multidisciplinary approach for detection, prevention and management of cardiac dysfunction in cancer patients. Jpn J Clin Oncol. 2017;47(8):678–82. https://doi.org/10.1093/jjco/hyx068.
Jeyaprakash P, Sangha S, Ellenberger K, Sivapathan S, Pathan F, Negishi K. Cardiotoxic effect of modern anthracycline dosing on left ventricular ejection fraction: a systematic review and meta-analysis of placebo arms from randomized controlled trials. J Am Heart Assoc. 2021;10(6):e018802.
Kolla BC, Roy SS, Duval S, Weisdorf D, Valeti U, Blaes A. Cardiac imaging methods for chemotherapy-related cardiotoxicity screening and related radiation exposure: current practice and trends. Anticancer Res. 2017;37(5):2445–9. https://doi.org/10.21873/anticanres.11584.
Zamorano JL, Lancellotti P, Rodriguez Muñoz D, Aboyans V, Asteggiano R, Galderisi M, ESC Scientific Document Group, et al. ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines: The Task Force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC). Eur Heart J. 2016;37(36):2768–801. https://doi.org/10.1093/eurheartj/ehw211.
Curigliano G, Cardinale D, Dent S, Criscitiello C, Aseyev O, Lenihan D, et al. Cardiotoxicity of anticancer treatments: epidemiology, detection, and management. CA Cancer J Clin. 2016;66(4):309–25. https://doi.org/10.3322/caac.21341.
Marcassa C. Neuronal damage and abnormal contraction: Is the circle of synchronicity complete? J Nucl Cardiol. 2019;26(3):880–2. https://doi.org/10.1007/s12350-017-1167-6.
Bleeker GB, Bax JJ, Steendijk P, Schalij MJ, van der Wall EE. Left ventricular dyssynchrony in patients with heart failure: pathophysiology, diagnosis and treatment. Nat Clin Pract Cardiovasc Med. 2006;3(4):213–9. https://doi.org/10.1038/ncpcardio0505.
Xu Y, Shi J, Zhao R, Zhang C, He Y, Lin J, et al. Anthracycline induced inconsistent left ventricular segmental systolic function variation in patients with lymphoma detected by three-dimensional speckle tracking imaging. Int J Cardiovasc Imaging. 2019;35(5):771–9. https://doi.org/10.1007/s10554-018-1510-2.
Singh JP, Solomon SD, Fradley MG, Barac A, Kremer KA, Beck CA, MADIT-CHIC Investigators, et al. Association of cardiac resynchronization therapy with change in left ventricular ejection fraction in patients with chemotherapy-induced cardiomyopathy. JAMA. 2019;322(18):1799–805. https://doi.org/10.1001/jama.2019.16658.
Malik D, Mittal B, Sood A, Parmar M, Kaur G, Bahl A. Left ventricular mechanical dyssynchrony assessment in long-standing type II diabetes mellitus patients with normal gated SPECT-MPI. J Nucl Cardiol. 2019;26(5):1650–8. https://doi.org/10.1007/s12350-018-1208-9.
Alvandi M, Shaghaghi Z, Aryafar V, Fariba F, Sanaei Z. The evaluation of left ventricular dyssynchrony in hypertensive patients with a preserved systolic function undergoing gated SPECT myocardial perfusion imaging. Ann Nucl Med. 2019;33(12):899–906. https://doi.org/10.1007/s12149-019-01402-4.
Hess PL, Shaw LK, Fudim M, Iskandrian AE, Borges-Neto S. The prognostic value of mechanical left ventricular dyssynchrony defined by phase analysis from gated single-photon emission computed tomography myocardial perfusion imaging among patients with coronary heart disease. J Nucl Cardiol. 2017;24(2):482–90. https://doi.org/10.1007/s12350-015-0388-9.
Mori H, Isobe S, Suzuki S, Unno K, Morimoto R, Kano N, et al. Prognostic value of left ventricular dyssynchrony evaluated by gated myocardial perfusion imaging in patients with chronic kidney disease and normal perfusion defect scores. J Nucl Cardiol. 2019;26(1):288–97. https://doi.org/10.1007/s12350-017-0889-9.
Sharir T, Hollander I, Kovalski G. Can phase analysis of gated myocardial perfusion single-photon emission computed tomography predict adverse outcome in cardiac sarcoidosis? J Nucl Cardiol. 2021;28(1):137–9. https://doi.org/10.1007/s12350-019-01744-6.
Ferrando Castagnetto R, Ferrando-Castagnetto F. Towards pre-treatment imaging prediction of chemotherapy-related cardiotoxicity. J Nucl Cardiol. 2022;29:590–3. https://doi.org/10.1007/s12350-020-02368-x.
Slomka PJ, Berman DS, Xu Y, Kavanagh P, Hayes SW, Dorbala S, et al. Fully automated wall motion and thickening scoring system for myocardial perfusion SPECT: method development and validation in large population. J Nucl Cardiol. 2012;19(2):291–302. https://doi.org/10.1007/s12350-011-9502-9.
Czaja-Ziółkowska MZ, Wasilewski JP, Głowacki J, Wygoda Z, Gąsior M. Useful assessment of myocardial viability and dyssynchrony from gated perfusion scintigraphy for better qualification for resynchronization therapy. Part 3. Kardiochir Torakochirurgia Pol. 2020;17(3):155–9. https://doi.org/10.5114/kitp.2020.99080.
Russell RR, Alexander J, Jain D, Poornima IG, Srivastava AV, Storozynsky E, et al. The role and clinical effectiveness of multimodality imaging in the management of cardiac complications of cancer and cancer therapy. J Nucl Cardiol. 2016;23(4):856–84. https://doi.org/10.1007/s12350-016-0538-8.
Reuvekamp EJ, Bulten BF, Nieuwenhuis AA, Meekes MRA, de Haan AFJ, Tolet J, et al. Does diastolic dysfunction precede systolic dysfunction in trastuzumab-induced cardiotoxicity? Assessment with multigated radionuclide angiography (MUGA). J Nucl Cardiol. 2016;23(4):824–32. https://doi.org/10.1007/s12350-015-0164-x.
Qiu C, Lin Y, Gu W, Wang J, Shao X, Zhang F, et al. Phase analysis of gated myocardial perfusion imaging for early diagnosis of cardiotoxicity caused by anthracyclines in patients with diffuse large B-cell lymphoma. Chin J Nucl Med Mol Imaging. 2019;39(10):591–6.
Jones KA, Small AD, Ray S, Hamilton DJ, Martin W, Robinson J, et al. Radionuclide ventriculography phase analysis for risk stratification of patients undergoing cardiotoxic cancer therapy. J Nucl Cardiol. 2022;1:1–9.
Valzania C, Paccagnella A, Spadotto A, Ruotolo I, Bonfiglioli R, Fallani F, et al. Early detection of cancer therapy cardiotoxicity by radionuclide angiography: an update. J Nucl Cardiol. 2023. https://doi.org/10.1007/s12350-023-03202-w.
Henriksen PA. Anthracycline cardiotoxicity: an update on mechanisms, monitoring and prevention. Heart. 2018;104(12):971–7. https://doi.org/10.1136/heartjnl-2017-312103.
McGowan JV, Chung R, Maulik A, Piotrowska I, Walker JM, Yellon DM. Anthracycline chemotherapy and cardiotoxicity. Cardiovasc Drugs Ther. 2017;31(1):63–75. https://doi.org/10.1007/s10557-016-6711-0.
Henry ML, Niu J, Zhang N, Giordano SH, Chavez-MacGregor M. Cardiotoxicity and cardiac monitoring among chemotherapy-treated breast cancer patients. JACC Cardiovasc Imaging. 2018;11(8):1084–93. https://doi.org/10.1016/j.jcmg.2018.06.005.PMID:30092967;PMCID:PMC6149535.
Acknowledgements
This study resulted from the research with ethics code/file number IR.MUK.REC.1399/176 that was approved and financed by the Kurdistan University of Medical Sciences. The authors had no conflict of interest to declare.
Funding
This study resulted from the research with ethics code/file number IR.MUK.REC.1399/176 that was approved and financed by the Kurdistan University of Medical Sciences.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Derakhshan, S., Ghaderi, B. & Roshani, D. Left ventricular mechanical dyssynchrony after chemotherapy in breast cancer patients with normal rest gated SPECT-MPI. Ann Nucl Med 38, 272–277 (2024). https://doi.org/10.1007/s12149-023-01897-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-023-01897-y