Abstract
Self-rated mental health (SRMH), a single item asking individuals to evaluate their mental or emotional health, is included in some surveys as an indicator of risk for mental disorders and to monitor population health, yet little longitudinal research examines how well it predicts future outcomes. Following a life course perspective, the current longitudinal study of 502 Canadian high school seniors tracked into midlife examined to what extent SRMH at ages 20, 25, and 32 years predicted depressive symptoms at ages 43 and 50. Hierarchical linear regressions showed that lower SRMH at age 25 and at 32 years was a significant predictor of higher levels of depressive symptoms at ages 43 and 50, even when controlling for sex, participant education, marital/cohabitation status, self-rated physical health, and baseline depressive symptoms. The results provide evidence that SRMH assessed during the transition to adulthood may be useful as a broad and powerful measure of risk for mental health problems decades into the future.
Similar content being viewed by others
Introduction
Mental health at any point in the lifespan is an important concern for individuals, families, communities, and public health professionals and policymakers. Self-rated mental health (SRMH), a one-item measure asking individuals to evaluate their mental or emotional health on a scale from “poor” to “excellent”, is included in some national surveys as an indicator of general risk for mental disorders and to monitor population health (e.g., Canadian Community Health Survey, Capaldi et al., 2021; Israel National Health Study, Levinson & Kaplan, 2014; U.S. Medical Expenditure Panel Survey, Nguyen et al., 2015). Although this item has been increasingly used since the mid-1990s (Ahmad et al., 2014), it is an understudied measure of well-being (McAlpine et al., 2018). We know that poorer SRMH is concurrently associated with depression, psychological distress, and other measures of mental health problems (Ahmad et al., 2014; Fleishman & Zuvekas, 2007; Hoff et al., 1997; Mawani & Gilmour, 2010), but little is understood about how well it foretells future mental health. Linking earlier SRMH with later mental health issues could inform healthcare research and policy and also provide insight into the predictive validity of this one-item measure. As such, there is a critical need for longitudinal studies (Ahmad et al., 2014; McAlpine et al., 2018). The objective of the current longitudinal study is to assess the predictive validity of SRMH by examining to what extent SRMH in the transition to adulthood (age 20 and 25) and early adulthood (age 32) predicts age 43 and age 50 depressive symptoms, an important indicator of midlife mental health.
The usefulness of SRMH for anticipating future mental health problems rests on the underlying construct it measures, a topic of ongoing discussion (Hoff et al., 1997; Levinson & Kaplan, 2014; Magwene et al., 2017). Research shows that while poor SRMH is correlated significantly with psychiatric diagnoses, it does not serve as a proxy for specific mental illnesses. SRMH may capture generalized psychological unease or distress, and it could pick up on subclinical symptoms that have yet to solidify into a particular disturbance such as depression or anxiety (Ahmad et al., 2014; Casu & Gremigni, 2019; Fleishman & Zuvekas, 2007; Hoff et al., 1997). Some researchers have argued in favor of SRMH as a measure of subjective well-being or mental health more than of mental illness (Levinson & Kaplan, 2014; Lombardo et al., 2018). Furthermore, SRMH appears to be an indicator of broad perceptions of one’s mental health, shaped by factors additional to any symptoms (e.g., physical health and limitations, life circumstances). These perceptions are believed to play an important role in help seeking, treatment compliance, and recovery from mental health conditions (Mawani & Gilmour, 2010; McAlpine et al., 2018; Nguyen et al., 2015; Zuvekas & Fleishman, 2008). Our examination of the longer-term association between SRMH in the 20s and 30s and depressive symptoms in midlife will add to knowledge about SRMH as an indicator of developing mental health problems.
A life course perspective on mental health
Our study is guided by a life course perspective on mental health. A core tenet is that human development is a lifelong process in which experiences of individuals in their familial, social, economic, and historical contexts are antecedents that set the stage for later experiences and well-being (Crosnoe & Elder, 2004; Shanahan, 2000). As such, understanding linkages between indicators of mental health across life stages is an important objective requiring longitudinal research over decades. A related assumption is that transitional periods, in which individuals may experience multiple role changes and challenges, provide opportunities for and threats to well-being, highlighting, for example, the transition to adulthood (which takes place through the 20s) as an important period of some vulnerability for the emergence of mental health problems (George, 1999). A life course approach considers risk (e.g., low socioeconomic status) and protective factors (e.g., social support) in describing pathways to mental health in adulthood. Poorer mental health is likely when there is an accumulation over time of risks along with few resources or protections that can mitigate the risks and promote mental health. Finally, a life course perspective assumes human agency, that is, that individuals are capable of actively making decisions about their futures and show resilience, although there are significant social structural constraints (e.g., gender bias, racism, poverty) that can place obstacles in the way and lead to psychopathology (Crosnoe & Elder, 2004; George, 1999; Mechanic & McAlpine, 2011; Shanahan, 2000).
Mental health in the transition to adulthood to early adulthood to midlife
Preceded by competencies gained and adversities experienced in childhood and adolescence, the transition to adulthood is a key period during which young people may access and acquire further resources that set them on a path toward a healthy and stable adulthood or they may flounder due to actions, cumulative vulnerabilities, or new circumstances that negatively affect their futures (Krahn et al., 2015; Masten & Tellegen, 2012). Developmental advances such as improved perspective taking and regulation of emotions are necessary for adapting to the demands of adulthood, which include developmental tasks such as leaving home, completing one’s education, finding a romantic partner, securing employment, establishing financial independence, and becoming a parent (Krahn et al., 2015; Schulenberg et al., 2004). The demands of this period may exceed available resources for meeting them. Indeed, a U.S. longitudinal study of 22- to 77-year-olds followed for 20 years revealed that daily stress exposure and stress reactivity were highest among individuals in their 20s, which declined as they aged into their 30s and 40s (Almeida et al., 2022). Anxiety, depression, and substance use disorders often emerge in the transition to adulthood, with troubling prevalence rates (George, 1999; Tanner et al., 2007). A 10-year longitudinal study of a Norwegian sample, for example, found that the 12-month prevalence of any mental disorder on the Munich Composite International Diagnostic Interview (M-CIDI; Wittchen & Pfister, 1997) was 32.2% of women and 19.8% of men among participants in their 20s. Anxiety disorders were most common in both sexes, followed by depressive disorders for women and alcohol use disorders for men (Gustavson et al., 2018).
Although longitudinal research following people from their 20s into early adulthood (their 30s) is scarce, the Almeida et al. (2022) study suggests that early adulthood may be relatively less stressful. In support, Gustavson et al. (2018) found that the 12-month prevalence of any mental disorder declined by the time women (25.3%) and men (12.9%) were in their 30s. Furthermore, according to scores on the Structured Diagnostic Interview for Psychopathologic Somatic Syndromes (SPIKE; Angst & Dobler-Mikola, 1985), the prospective Zurich Cohort Study documented decreased 12-month prevalence rates for major depression, minor depression, and depressive symptoms for participants in their 30s compared to their high points in the 20s (Merikangas et al., 2003). While depression may decrease on average into early adulthood, there is also stability in mental health problems from the 20s into the 30s. A diagnosis of anxiety or depressive disorder in the 20s, for example, increases by manyfold the risk of a repeat diagnosis in the 30s (Gustavson et al., 2018). Nevertheless, accomplishments and competencies gained during the transition to adulthood (e.g., fulfilling educational and employment expectations; getting married) may offset some of its risks, leading to positive mental health in early adulthood and beyond (Howard et al., 2010; Johnson et al., 2017; Masten et al., 2010; Mossakowski, 2011).
Midlife, which is generally considered to encompass ages 40 to 60 (Lachman et al., 2015), follows early adulthood and poses both opportunities for and risks to well-being. In midlife many people may experience the positive social and emotional impacts of their childrearing years and work productivity. At the same time, challenges such as launching children, caring for aging parents, maintaining a career, planning for retirement, and coping with emerging physical health issues can be turning points for worsening mental health (Infurna et al., 2020). Although there is little support for a generalized “midlife crisis” (Galambos et al., 2020), the longitudinal Dunedin Birth Cohort Study showed that by age 45 nearly everyone will have experienced at least one mental disorder (Caspi et al., 2020), meeting criteria of the Diagnostic and Statistical Manual of Mental Disorders (e.g., DSM-5; American Psychiatric Association, 2013). Major depressive episodes (MDEs) are especially common, with a lifetime prevalence in the U.S. National Comorbidity Survey Replication of about one in five in the 18–49-year-old age group (Kessler et al., 2010), as assessed by the CIDI (Kessler & Ustün, 2004). Furthermore, Infurna et al. (2020) concluded that middle-aged adults, particularly in some segments of the population (e.g., lower SES, women) have elevated rates of depression and distress compared to younger and older adults. As such, it is important to identify markers of distress earlier in life that may foreshadow depressive symptoms in midlife. SRMH in the transition to adulthood or early adulthood might signal the potential for future depression.
Correlates of self-rated mental health
SRMH is commonly assessed with only one item, but this item may be a potent subjective indicator that provides insight into self-awareness and feelings about one’s well-being (McAlpine et al., 2018). A scoping review of the literature found that poorer SRMH was associated with psychological distress and serious mental health conditions such as major depression, based on a variety of interview and questionnaire instruments (Ahmad et al., 2014). Mawani and Gilmour (2010), for example, reported that a national sample of Canadians (age 15 and above) who experienced an MDE in the past month, identified by scores on the CIDI, had 26 times the odds of rating their mental health as poor/fair compared to those with no MDE in the past month. Similarly, participants with high levels of psychological distress on the K-6 (Kessler et al., 2002) were 36 times more likely to report poor/fair SRMH compared to those with few symptoms of psychological distress (Mawani & Gilmour, 2010). In a sample of Canadian adolescents in British Columbia, Sawatzky et al. (2010) documented a significant association between SRMH and depressive symptoms, assessed with 12 items from the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977). In a sample of older (ages 60 to 98) Korean Americans residing in New York City, SRMH was a significant predictor of three different measures of depressive symptoms (CESD-10, Andresen et al., 1994; PHQ-9, Kroenke et al., 2001; Geriatric Depression Scale–Short Form, Sheikh & Yesavage, 1986), after controlling for variables such as education, gender, and marital status (Jang et al., 2012).
Poorer SRMH is also related to lower life satisfaction, sense of community, and belongingness (Ahmad et al., 2014; Lombardo et al., 2018; Palis et al., 2018; Sawatzky et al., 2010), higher experience of family violence (Farhat et al., 2022), and subjectively poorer physical health and the presence of chronic physical conditions (Fleishman & Zuvekas, 2007; McAlpine et al., 2018; Sawatzky et al., 2010). SRMH in Canada was lower during the COVID-19 pandemic than before (Capaldi et al., 2021), and individuals who reported lower SRMH were also more likely to use health and mental health services (Ahmad et al., 2014; McAlpine et al., 2018; Nguyen et al., 2015). As a holistic assessment of one’s mental health, SRMH may be useful for screening and potentially identifying those in need of treatment (Casu & Gremigni, 2019; Mawani & Gilmour, 2010; McAlpine et al., 2018).
A paucity of longitudinal research on SRMH limits knowledge about how well it forecasts future well-being, information that is essential for understanding mental health across the life cycle as well as for evaluating the predictive value of this single item. In one exception, a prospective study of a community sample of adults in New Haven, Connecticut showed that participants with poor SRMH were significantly more likely than those with better SRMH to experience an MDE in the next 12 months (assessed with the DIS; Robins et al., 1981), controlling for confounders such as age, gender, and depression at baseline (Hoff et al., 1997). In a U.S. sample of adults with depression (based on the PHQ-2; Kroenke et al., 2003) or severe psychological distress on the K6 at baseline, participants who rated their SRMH as good/very good/excellent had 30% lower odds of experiencing depression or serious psychological distress one year later, controlling for sociodemographic characteristics, mental health care utilization, and initial symptoms (McAlpine et al., 2018). In U.S. students tracked across their first year of university, higher SRMH at baseline predicted lower loneliness in fall and spring semesters on a brief version of the UCLA Loneliness Scale (Roberts et al., 1993), less anxiety in fall and spring (Generalized Anxiety Disorders 7-item Scale; Spitzer et al., 2006), and higher self-reported GPA in the fall semester; SRMH was not related to depressive symptoms (CESD-10; Andresen et al., 1994) in either semester (Jones & Schreier, 2021). In a prospective cohort study of French participants (ages 23 to 93 years), average SRMH was higher before the COVID-19 pandemic than during lockdown, with women, young to middle-aged adults (23 to 49 years), and the elderly (age 70 and over) more negatively affected (Ramiz et al., 2021). Finally, in a U.S. sample of caregivers for the elderly there were steeper declines in SRMH over two years among those who initially reported lower SRMH (Haug et al., 1999). These few longitudinal studies suggest that single-item SRMH might be sensitive to emerging mental health problems, but we do not know whether SRMH predicts well-being more than two years into the future.
Given cross-sectional results supporting a link between SRMH, on the one hand, and major depression and depressive symptoms, on the other (e.g., Mawani & Gilmour, 2010; Sawatzky et al., 2010), along with some longitudinal evidence that SRMH predicts future episodes of major depression and psychological distress (Hoff et al., 1997; McAlpine et al., 2018), it makes sense to ask to what extent SRMH in the transition to adulthood and early adulthood predicts depressive symptoms in midlife. SRMH may provide a window into distress that does not meet formal criteria for psychopathology but that may be a harbinger of future depressive symptoms.
The current study
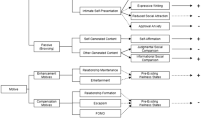
Influenced by a life course perspective, we examine to what extent single-item SRMH measured in the same individuals at two points during the critical transition to adulthood (i.e., ages 20 and 25) and once in early adulthood (i.e., age 32) anticipates depressive symptoms up to 30 years later in middle adulthood (i.e., ages 43 and 50). The data are drawn from a sample of high school students living in a city in western Canada who were surveyed repeatedly over three decades. First, we assess the relative strength of SRMH scores in the transition to adulthood and early adulthood for predicting midlife depressive symptoms without controlling for possible confounding variables. Second, we examine the impact of SRMH, controlling for participants’ sex, whether participants attained a university degree by age 43 or 50, marital status and self-rated physical health (SRPH) at ages 43 or 50, and depressive symptoms at baseline.
Confounding variables were selected because they could be associated with SMRH and/or depressive symptoms and were common controls in previous SRMH studies (e.g., Ahmad et al., 2014; Hoff et al., 1997). Sex of participant is controlled because women are more likely than men to experience major depression (e.g., Hoff et al., 1997; Kessler et al., 2010), and a few studies have found poorer SRMH among women (Assari & Lankarani, 2017; Cohen & Patten, 2005). We control for whether participants held a university degree, an indicator of socioeconomic status (SES), as higher education and SES are related to better SRMH (Assari & Lankarani, 2017; Jang et al., 2012; Su et al., 2021; Zuvekas & Fleishman, 2008). Married people and those with partners may have better SRMH than non-partnered individuals, suggesting the importance of marital status (Chiu et al., 2017; Hoff et al., 1997; McAlpine et al., 2018). SRPH is controlled due to significant positive correlations of SRMH with SRPH (Levinson & Kaplan, 2014; Sawatzky et al., 2010). Finally, Hoff et al. (1997) showed that in the New Haven Catchment Study, the best predictor of a depressive episode in the following year was major depression at baseline. Thus, baseline (age 18) depressive symptomatology is controlled to determine whether SRMH indicators in the transition to adulthood are robust enough to explain variability in midlife depressive symptoms once adolescent depression is also in the model. Controlling for possible confounding variables provides a conservative test of the SRMH-depressive symptoms connection across decades.
Method
Participants
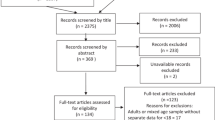
In Spring 1985 (baseline; Wave 1), 983 Grade 12 students (age 18) were surveyed in six public high schools selected to represent middle- and lower-income neighborhoods in Edmonton, Alberta as part of the Edmonton Transitions Study (ETS). Questionnaires completed in class included indicators of family background, educational and work experiences, and well-being. Over 90% (n = 894) consented to be contacted to participate in the future. Follow-up questionnaires were mailed to consenters in 1986 (age 19; n = 665 returned), and again in 1987 (age 20; n = 547), 1989 (age 22; n = 504), and 1992 (age 25; n = 404) but only to those who participated in each previous wave. In 1999, follow-up telephone surveys targeted all consenting Wave 1 participants (age 32; n = 509), as did telephone and web-based surveys in 2010 (age 43; n = 405), and 2017 (age 50; n = 404). Of the original sample (n = 983), 20% participated only at Wave 1, 18% completed all eight waves, and 42% completed between four and seven waves. This study received research ethics approval prior to each data collection; the most recent approval (June 26, 2017) was granted by the University of Alberta Research Ethics Board 2 (application title: Transitions to Midlife: 32 Year Follow-up of the Class of 1985; protocol number: Pro00074272).
Given our focus on midlife depressive symptoms and the fact that the Center for Epidemiologic Studies 10-item Depression Scale (CESD-10; Andresen et al., 1994) was administered only at age 43 and age 50, the study sample was filtered to include 502 individuals who had CESD-10 scores available at age 43 and/or age 50: n = 303 with the CESD-10 at age 43 and 50; n = 99 only at age 43; and n = 100 with the CESD-10 only at age 50. Table 1 presents demographic characteristics at baseline for the original full sample as well as the reduced sample of 502 participants used for analyses in the current study. These figures show participants were predominately White, born in Canada, and living in households where no parent held a university degree. Census data (McVey & Kalbach, 1995) showed that the original full sample was representative of western Canadian urban youth born in 1967 on parents’ education, immigration status, and ethnicity. By midlife (age 43 or 50), 40% of the participants had attained a university (e.g., bachelor’s) degree or higher. Three-fourths were married or cohabiting at age 43 (76%) and age 50 (77%), and the majority were parents (age 43: 78%; age 50: 82%). A large majority were employed at age 43 and 50 (92% and 91%, respectively) with about 2% unemployed (looking for work) at each age.
Comparisons of participants included in the current study sample (n = 502) with excluded participants (n = 481) were conducted on the key variables used in our regression analyses. A four-item measure of depressive symptoms at age 18 was not significantly different for continuing participants versus those who attrited. SRMH was not assessed until age 20, so a baseline comparison could not be made, but included and excluded participants did not differ on SRMH at ages 20, 25, or 32 years, nor did they differ significantly on SRPH at those ages. With respect to control variables, women and individuals with at least one university-educated parent were more likely to participate in midlife (age 43 and/or 50).
Measures
Depressive symptoms
At ages 43 and 50, the mean of 10 items (Andresen et al., 1994) from the 20-item Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977) assessed “how often in the past few months” respondents experienced symptoms of depression such as feeling “depressed” or “lonely.” Items were evaluated on a scale from 1 (never) to 5 (almost always). Internal consistency was high at age 43 (α = 0.87) and age 50 (α = 0.87). The CESD-10 has been widely used and validated in diverse samples around the world as a screening instrument for probable clinical depression (e.g., Baron et al., 2017). Because we modified the timeframe of symptoms (over a few months rather than a week), the response scale, and the scoring (calculating a mean rather than total) to suit our survey format, we interpret the scale score as a continuous measure with higher scores indicating more frequent relatively recent depressive symptoms.
Self-rated mental health (SRMH)
Beginning in 1987 when participants were age 20, we asked how healthy they felt “mentally” in the past few months on a scale from 1 (very unhealthy) to 5 (very healthy). This item was adapted from the 1983 Edmonton Area Survey (Population Research Laboratory, 2015), which predated the increased use of single-item SRMH measures in surveys in the 1990s and 2000s. As such, our response scale differs from more recently used SRMH items, which are typically rated on a scale ranging from “poor” to “excellent” (Ahmad et al., 2014). SRMH at ages 20, 25, and 32 are used in the current study to predict midlife CESD-10 scores.
Control variables
Sex was coded as 0 (female) or 1 (male). Participant education, based on highest level of education reported at either age 43 or 50, was dichotomized, with 1 = university degree or higher. Marital status was coded at age 43 and age 50 as a binary variable, with 1 = married or cohabiting.
Self-rated physical health (SRPH) was assessed at age 43 and 50 by asking how healthy participants felt “physically” in the past few months on a scale from 1 (very unhealthy) to 5 (very healthy), parallel to our SRMH item and similar to SRPH as measured in other studies (Jones & Schreier, 2021; Levinson & Kaplan, 2014; Sawatzky et al., 2010).
At age 18, the mean of four items from the 20-item CES-D assessed baseline depressive symptoms (“depressed,” “lonely,” “talked less than usual,” and “people were unfriendly”) in the past few months on a scale from 1 (never) to 5 (almost always). As shown in previous research with ETS participants, internal consistency of the four-item scale was acceptable (α = 0.68; Galambos et al., 2006). In the current sample within time, this four-item scale correlated significantly (p < 0.001) with the full CESD-10 at age 43 (r = 0.83) and age 50 (r = 0.87).
Analytic plan
For each outcome (CESD-10 at age 43 and at age 50) two regression models were estimated. In the first model, SRMH items at three earlier ages were included as predictors: CES-D Age 43 or Age 50 = a + B1(SRMH Age 20) + B2(SRMH Age 25) + B3(SRMH Age 32), where a = constant. In the second model, control variables were added to the set of SRMH items: CES-D Age 43 or 50 = a + B1(SRMH Age 20) + B2(SRMH Age 25) + B3(SRMH Age 32) + B4(Sex) + B5 (Education) + B6(Concurrent Marital Status, Age 43 or 50) + B7(Concurrent SRPH, Age 43 or 50) + B8(Depressive symptoms Age 18).
Missing data and multiple imputation
Missing data ranged from 0% to 39.64% (see Table 2), and most missing values were due to individuals not participating at a given wave rather than to item non-response. To handle missing data, and in accordance with recommended procedures, multiple imputation (MI) with auxiliary variables maximized the use of all observed data for those with CESD-10 scores at age 43 and/or 50. MI takes many copies of a dataset and imputes (or assigns scores for) the missing values in each copy using a model based on observed data. Then the substantive analyses (e.g., the regressions described above) are conducted on each of the imputed datasets, with the parameters combined to generate the final estimates. MI is generally considered superior to mean substitution or complete cases analysis as it is more likely to lead to non-biased inferences (Graham, 2009; Lee et al., 2016: Schlomer et al., 2010).
Our imputation model included 36 auxiliary variables selected because they were known or likely to be associated with SRMH, CESD-10 scores, the control variables, or missingness (e.g., parent education, immigration status, happiness at baseline). The inclusion of a large number of carefully chosen auxiliary variables is an optimal strategy for reducing bias and increasing power (Graham, 2009; Schlomer et al., 2010). Thirty imputed datasets were generated with 100 iterations, and regression models were run for all 30, with the estimates pooled. Significance was set at 0.05 (two-tailed). SPSS 28.0.1 was used for all analyses.
MI assumes that data are missing at random. The lack of significant differences between continuers and attriters on key study variables (baseline depressive symptoms, SRMH and SRPH scores), along with the inclusion of possible predictors of missingness in the imputation and analytic (e.g., sex) models, support the missing at random criterion (Graham, 2009; Lee et al., 2016).
Results
Table 2 presents descriptive statistics for each measure. On average, and consistent with a non-clinical sample, participants did not report high levels of depressive symptoms on the CESD-10 at ages 43 or 50, although depressive symptoms at age 18 were higher, consistent with earlier research on this sample (Johnson et al., 2021). SRMH and SRPH mean scores indicated that participants felt quite healthy mentally and physically at all ages, but there was substantial variability across participants.
Table 3 presents correlations among the measures. SRMH at ages 20, 25, and 32 showed significant small to moderate intercorrelations. Higher SRMH at ages 20, 25, and 32 were weakly to moderately associated with lower depressive symptoms in midlife (i.e., CESD-10 at ages 43 and 50). Among control variables, sex was related to CESD-10 only at age 50, with men less likely to report depressive symptoms. A university education was related to a lower CESD-10 score only at age 43. Marriage or cohabitation in midlife was associated with higher SRMH at some earlier points and with lower CESD-10 scores in midlife, while better SRPH was consistently associated with better SRMH and lower CESD-10 scores. Finally, higher depressive symptoms at age 18 was related to lower SRMH at all ages and to higher midlife CESD-10 scores.
Table 4 presents the results of the regression analyses. Considering Model 1, which explained 19% of the variance in CESD-10 at age 43, higher SRMH at ages 25 and 32 predicted lower CESD-10 scores. Model 2 explained 39% of the variance in age 43 CESD-10 symptoms, with age 25 and 32 SRMH again attaining significance. A university education, being married or cohabiting, reporting better physical health, and showing lower depressive symptoms at age 18 predicted lower CESD-10 scores at age 43.
With age 50 CESD-10 scores as the criterion, higher SRMH at ages 25 and 32 predicted lower depressive symptoms at age 50 in both models. Model 1 explained 18% of the variance and Model 2 explained 29% of the variance in age 50 CESD-10. Being married or cohabiting, reporting better SRPH, and lower depressive symptoms scores at age 18 predicted lower CESD-10 scores at age 50.
Discussion
The results of this study showed that lower SRMH, assessed with a single item, forecast depressive symptoms up to 25 years into the future. The predictive strength of single-item SRMH assessed in the middle of the transition to adulthood (age 25) and in early adulthood (age 32) is remarkable, particularly considering that the import of SRMH held when controlling for sex, depressive symptoms at age 18, educational level, and concurrently measured marital status and SRPH in midlife. The results are interpretable from a life course perspective, which highlights the likelihood of connections between early and later mental health experiences. Self-assessment that one’s mental health may not be in good shape constitutes a risk particularly if it becomes a continuing part of one’s narrative in the 20s and early 30s. We concur with McAlpine et al. (2018) in their assessment that SRMH may be a powerful construct.
Whereas SRMH explained a significant 18 to 19 percent of the variance in depressive symptoms in midlife, the control variables explained an additional 10 to 20 percent. Having a university education, being married or cohabiting, reporting better physical health, and reporting fewer depressive symptoms in high school appeared to protect against midlife depressive symptoms. Furthermore, bivariate correlations showed that better SRMH at ages 25 and 32 was linked with having a marital/romantic partner at age 50, and SRMH at ages 20, 25, and 32 were positively correlated with SRPH at ages 43 and 50 (see Table 3). Consistent with a life course perspective, SRMH in the transition to adulthood and early adulthood may have cascading effects on other circumstances in young people’s lives, which ultimately carry through to midlife – and likely beyond.
The fact that SRMH early in the transition to adulthood (i.e., age 20) did not predict midlife depressive symptoms is of interest. The early 20s is a period of instability in living, financial, romantic, educational, and employment situations (Krahn et al., 2015; Masten et al., 2010), and possibly, of improving mental health on average as young people meet developmental challenges and begin to settle into their roles (Galambos et al., 2006; Howard et al., 2010). It could be that SRMH is too unstable when lives are in flux to be a reliable predictor of mental health problems decades later. Indeed, correlations (Table 3) showed there was somewhat stronger stability in SRMH from age 25 to 32 (r = 0.32) than from age 20 to age 25 (r = 0.22). And SRMH at age 25 and age 32 was more strongly correlated with midlife depressive symptoms (rs between -0.31 and -0.36) than was SRMH at age 20 (rs of -0.19 and -0.17 for age 43 and age 50 depressive symptoms, respectively). This does not mean that SRMH in the early 20s is irrelevant. It may be an important harbinger of difficulties in the shorter term for individuals early in the transition to adulthood (see e.g., Jones & Schreier, 2021), which could spill over into well-being in their later 20s.
Questions about the meaning of SRMH, and what it measures, remain. The factors that shape individuals’ constructions and interpretations of their overall mental health may be many, and they may also differ from person to person. Given that specific disorders like major depression or generalized anxiety disorder can wax and wane over time (Caspi et al., 2021), SRMH might provide a broad but important glimpse into psychological health, useful for tracking the well-being of individuals through life’s stages as they encounter hills and valleys on the way. As many people with mental health issues do not seek professional help or wait years until they do (Wang et al., 2005), SRMH could be an early marker of developing problems, constituting a good screening tool for use by clinicians (Casu & Gremigni, 2019), in addition to its utility for monitoring population health.
Recently, Allen et al. (2022) called for more research on the reliability and validity of single-item measures, arguing that such items have a poor and probably undeserved reputation (see also Fisher et al., 2016). Our longitudinal results suggest there is merit to using single-item SRMH in research and possibly clinical applications. It could be that, like the better known and well-studied self-rated global health item that is robust enough to predict eventual morbidity and mortality (Benyamini et al., 2011; Idler & Benyamini, 1997), SRMH will earn its place among short, easy-to-administer, and meaningful tools.
Limitations
Although this prospective study has considerable strength, including multiple waves at which SRMH was measured and its representativeness of youth in western cities in Canada at baseline, there are limitations. First, because SRMH was first measured in the ETS prior to its more common usage in survey research, our response scale ranged from very unhealthy to very healthy rather than from poor to excellent. It is unclear whether this difference is consequential, but the substantive results (i.e., its positive associations with the CESD-10) suggest our item may perform similarly to others in more recent studies. Second, to better fit into the format of our survey, the timeframe and response scale of the CESD-10 was modified. We believe our continuous measure provides important insight into the recent frequency of depressive symptoms in a non-clinical sample but we were unable to conduct analyses to determine whether earlier SRMH predicted a probable diagnosis of major depression in midlife. Third, as is typical with a three-decade longitudinal study, attrition resulted in missing data. To ensure the validity of our results, we followed current best practices for managing missing data, one of which is to conduct MI with many auxiliary variables. This strategy uses all observed data and produces less biased estimates than complete cases analysis or mean substitution (Graham, 2009; Lee et al., 2016). Finally, because the sample is largely White the results may not be generalizable to other racialized groups. Research shows, for example, that SRMH may be more strongly related to mental health conditions and health service utilization in White than in Black and Hispanic samples (McAlpine et al., 2018; Zuvekas & Fleishman, 2008).
Conclusion
In the last 25 or 30 years, single-item SRMH has appeared increasingly in population health surveys as a measure of well-being, psychological distress, and mental health problems and disorders. Although it is a broad measure not interchangeable with psychiatric diagnoses, the literature shows that it does appear to tie into symptoms that may reflect serious mental health conditions as well as possibly emerging mental health problems. Most research on SRMH has been cross-sectional rather than longitudinal, and the few prospective studies that are published have not followed participants for more than one or two years. By taking a life course perspective on SRMH and examining whether SRMH in the transition to adulthood and early adulthood foretells depressive symptoms in midlife, the current study provides a unique view into the value of SRMH as an indicator of developing mental health problems. The finding that lower SRMH predicted higher depressive symptoms up to 25 years later, after controlling for life events such as marriage and achieving a university education, is remarkable and represents a unique contribution to the literature. SRMH is an indicator deserving of further empirical attention.
References
Ahmad, F., Jhajj, A. K., Stewart, D. E., Burghardt, M., & Bierman, A. S. (2014). Single item measures of self-rated mental health: A scoping review. BMC Health Services Research, 14, 398. https://doi.org/10.1186/1472-6963-14-398
Allen, M. S., Iliescu, D., & Greiff, S. (2022). Single item measures in psychological science: A call to action. European Journal of Psychological Assessment, 38(1), 1–5. https://doi.org/10.1027/1015-5759/a000699
Almeida, D. M, Rush, J., Mogle, J. Piazza, J. R., Cerino, E., & Charles, S. T. (2022). Longitudinal change in daily stress across 20 years of adulthood: Results from the National Study of Daily Experiences. Developmental Psychology. Advance online publication. https://doi.org/10.1037/dev0001469
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Association.
Andresen, E. M., Malmgren, J. A., Carter, W. B., & Patrick, D. L. (1994). Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). American Journal of Preventive Medicine, 10(2), 77–84. https://doi.org/10.1016/s0749-3797(18)30622-6
Angst, J., & Dobler-Mikola,. (1985). The Zurich Study: A prospective epidemiological study of depressive, neurotic and psychosomatic syndromes. IV: Recurrent and non-recurrent brief depression. European Archives of Psychiatry and Neurological Sciences, 234(6), 408–416. https://doi.org/10.1007/BF00386060
Assari, S., & Lankarani, M. M. (2017). Demographic and socioeconomic determinants of physical and mental self-rated health across 10 ethnic groups in the United States. International Journal of Epidemiologic Research, 3(12), 185–193. https://doi.org/10.15171/ijer.2017.02
Baron, E. C., Davies, T., & Lund, C. (2017). Validation of the 10-item Centre for Epidemiological Studies Depression Scale (CES-D-10) in Zulu, Xhosa and Afrikaans populations in South Africa. BMC Psychiatry, 17, 6. https://doi.org/10.1186/s12888-016-1178-x
Benyamini, Y., Blumstein, T., Murad, H., & Lerner-Geva, L. (2011). Changes over time from baseline poor self-rated health: For whom does poor self-rated health not predict mortality? Psychology & Health, 26(11), 1446–1462. https://doi.org/10.1080/08870446.2011.559231
Capaldi, C. A., Liu, L., & Dopko, R. L. (2021). Positive mental health and perceived change in mental health among adults in Canada during the second wave of the COVID-19 pandemic. Health Promotion and Chronic Disease Prevention in Canada, 41(11). https://doi.org/10.24095/hpcdp.41.11.05
Caspi, A., Houts, R. M., Ambler, A., Danese, A., Elliott, M. L., Hariri, A., Harrington, H., Hogan, S., Poulton, R., Ramrakha, S., Rasmussen, L. J. H., Reuben, A., Richmond-Rakerd, L., Sugden, K., Wertz, J., Williams, B. S., & Moffitt, T. E. (2020). Longitudinal assessment of mental health disorders and comorbidities across 4 decades among participants in the Dunedin Birth Cohort Study. JAMA Network Open, 3(4), e203221. https://doi.org/10.1001/jamanetworkopen.2020.3221
Casu, G., & Gremigni, P. (2019). Is a single-item measure of self-rated mental health useful from a clinimetric perspective? Psychotherapy and Psychosomatics, 88(3), 177–178. https://doi.org/10.1159/000497373
Chiu, M., Rahman, F., Kurdyak, P., Cairney, J., Jembere, N., & Vigod, S. (2017). Self-rated health and mental health of lone fathers compared with lone mothers and partnered fathers: A population-based cross-sectional study. Journal of Epidemiology and Community Health, 71(5), 417–423. https://doi.org/10.1136/jech-2016-208005
Cohen, J. S., & Patten, S. (2005). Well-being in residency training: A survey examining resident physician satisfaction both within and outside of residency training and mental health in Alberta. BMC Medical Education, 5, 21. https://doi.org/10.1186/1472-6920-5-21
Crosnoe, R., & Elder, G. H., Jr. (2004). From childhood to the later years: Pathways of human development. Research on Aging, 26(6), 623–654. https://doi.org/10.1177/0164027504268491
Farhat, S. M. M., Berbiche, D., & Vasiliadis, H. (2022). Family violence associated with self-rated health, satisfaction with life, and health service use in primary care older adults. Journal of Interpersonal Violence, 37(5–6), 2487–2509. https://doi.org/10.1177/0886260520938513
Fisher, G. G., Mathews, R. A., & Gibbons, A. M. (2016). Developing and investigating the use of single-item measures in organizational research. Journal of Occupational Health Psychology, 21(1), 3–23. https://doi.org/10.1037/a0039139
Fleishman, J. A., & Zuvekas, S. H. (2007). Global self-rated mental health: Associations with other mental health measures and with role function. Medical Care, 45(7), 602–609. https://doi.org/10.1097/MLR.0b013e31803bb4b0
Galambos, N. L., Barker, E. T., & Krahn, H. J. (2006). Depression, self-esteem, and anger in emerging adulthood: Seven-year trajectories. Developmental Psychology, 42(2), 350–365. https://doi.org/10.1037/0012-1649.42.2.350
Galambos, N. L., Krahn, H. J., Johnson, M. D., & Lachman, M. E. (2020). The U shape of happiness across the life course: Expanding the discussion. Perspectives on Psychological Science, 15(4), 898–912. https://doi.org/10.1177/1745691620902428
George, L. K. (1999). Life-course perspectives on mental health. In C. S. Aneshensel & J. C. Phelan (Eds.), Handbook of the sociology of mental health (pp. 565–583). Kluwer Academic/Plenum Publishers. https://doi.org/10.1007/0-387-36223-1_27
Graham, J. W. (2009). Missing data analysis: Making it work in the real world. Annual Review of Psychology, 60, 549–576. https://doi.org/10.1146/annurev.psych.58.110405.085530
Gustavson, K., Knudsen, A. K., Nesvåg, R., Knudsen, G. P., Vollset, S. E., & Reichborn-Kjennerud, T. (2018). Prevalence and stability of mental disorders among young adults: Findings from a longitudinal study. BMC Psychiatry, 18, 1. https://doi.org/10.1186/s12888-018-1647-5
Haug, M. R., Ford, A. B., Stange, K. C., Noelker, L. S., & Gaines, A. D. (1999). Effect of giving care on caregivers’ health. Research on Aging, 21(4), 515–538. https://doi.org/10.1177/0164027599214001
Hoff, R., Bruce, M., Kasl, S., & Jacobs, S. (1997). Subjective ratings of emotional health as a risk factor for major depression in a community sample. British Journal of Psychiatry, 170(2), 167–172. https://doi.org/10.1192/bjp.170.2.167
Howard, A. L., Galambos, N. L., & Krahn, H. J. (2010). Paths to success in young adulthood from mental health and life transitions in emerging adulthood. International Journal of Behavioral Development, 34(6), 538–546. https://doi.org/10.1177/0165025410365803
Idler, E. L., & Benyamini, Y. (1997). Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior, 38(1), 21–37. https://doi.org/10.2307/2955359
Infurna, F. J., Gerstorf, D., & Lachman, M. E. (2020). Midlife in the 2020s: Opportunities and challenges. American Psychologist, 75(4), 470–485. https://doi.org/10.1037/amp0000591
Jang, Y., Park, N. S., Kim, G., Kwag, K. H., Roh, S., & Chiriboga, D. A. (2012). The association between self-rated mental health and symptoms of depression in Korean American older adults. Aging & Mental Health, 16(4), 481–485. https://doi.org/10.1080/13607863.2011.628981
Johnson, M. D., Galambos, N. L., & Krahn, H. J. (2021). Family context, life transitions, and subjective well-being from age 18 to 50 years. Developmental Psychology, 57(11), 1968–1980. https://doi.org/10.1037/dev0001243
Johnson, M. D., Krahn, H. J., & Galambos, N. L. (2017). Better late than early: Marital timing and subjective well-being in midlife. Journal of Family Psychology, 31(5), 635–641. https://doi.org/10.1037/fam0000297
Jones, E. J., & Schreier, H. M. C. (2021). Self-rated mental and physical health are prospectively associated with psychosocial and academic adjustment to college. Journal of American College Health. Advance online publication. https://doi.org/10.1080/07448481.2021.1904956.
Kessler, R. C., Andrews, G., Colpe, L. J., Hiripi, E., Mroczek, D. K., Normand, S.-L.T., Walters, E. E., & Zaslavsky, A. M. (2002). Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine, 32(6), 959–976. https://doi.org/10.1017/s0033291702006074
Kessler, R. C., Birnbaum, H., Bromet, E., Hwang, I., Sampson, N., & Shahly, V. (2010). Age differences in major depression: Results from the National Comorbidity Survey Replication (NCS-R). Psychological Medicine, 40(2), 225–237. https://doi.org/10.1017/S0033291709990213
Kessler, R. C., & Ustün, T. B. (2004). The World Mental Health (WMH) Survey Initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). International Journal of Methods in Psychiatric Research, 13(2), 93–121. https://doi.org/10.1002/mpr.168
Krahn, H. J., Howard, A. L., & Galambos, N. L. (2015). Exploring or floundering? The meaning of employment and educational fluctuations in emerging adulthood. Youth and Society, 47(2), 245–266. https://doi.org/10.1177/0044118X12459061
Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2003). The Patient Health Questionnaire-2: Validity of a two-item depression screener. Medical Care, 41(11), 1284–1292. https://doi.org/10.1097/01.MLR.0000093487.78664.3C
Lachman, M. E., Teshale, S., & Agrigoroaei, S. (2015). Midlife as a pivotal period in the life course: Balancing growth and decline at the crossroads of youth and old age. International Journal of Behavioral Development, 39(1), 20–31. https://doi.org/10.1177/0165025414533223
Lee, K. J., Roberts, G., Doyle, L. W., Anderson, P. J., & Carlin, J. B. (2016). Multiple imputation for missing data in a detailed case study involving imputation of missing outcome data. International Journal of Social Research Methodology, 19(5), 575–591. https://doi.org/10.1080/13645579.2015.1126486
Levinson, D., & Kaplan, G. (2014). What does self rated mental health represent? Journal of Public Health Research, 3(287), 122–127. https://doi.org/10.4081/jphr.2014.287
Lombardo, P., Jones, W., Wang, L., Shen, X., & Goldner, E. M. (2018). The fundamental association between mental health and life satisfaction: Results from successive waves of a Canadian national survey. BMC Public Health, 18, 342. https://doi.org/10.1186/s12889-018-5235-x
Magwene, E., Quiñones, A. R., Marshall, G. L., Makaroun, L. K., & Thielke, S. (2017). Older adults rate their mental health better than their general health. Journal of Public Health Research, 6(2), 967. https://doi.org/10.4081/jphr.2017.967
Masten, A. S., Desjardins, C. D., McCormick, C. M., Kuo, S.I.-C., & Long, J. D. (2010). The significance of childhood competence and problems for adult success in work: A developmental cascade analysis. Development and Psychopathology, 22(3), 679–694. https://doi.org/10.1017/S0954579410000362
Masten, A. S., & Tellegen, A. (2012). Resilience in developmental psychopathology: Contributions of the Project Competence Longitudinal Study. Development and Psychopathology, 24(2), 345–361. https://doi.org/10.1017/S095457941200003X
Mawani, F. N., & Gilmour, H. (2010). Validation of self-rated mental health. Health Reports, 21(3), 61–75. Statistics Canada, Catalogue no. 82-003-XPE. https://www150.statcan.gc.ca/n1/pub/82-003-x/82-003-x2009003-eng.pdf.
McAlpine, D. D., McCreedy, E., & Alang, S. (2018). The meaning and predictive value of self-rated mental health among persons with a mental health problem. Journal of Health and Social Behavior, 59(2), 200–214. https://doi.org/10.1177/0022146518755485
McVey, W., Jr., & Kalbach, W. (1995). Canadian population. Nelson Canada.
Mechanic D., & McAlpine D.D. (2011). Mental health and aging: A life-course perspective. In R. Settersten & J. Angel (Eds.), Handbook of sociology of aging (pp. 477–493). Springer. https://doi.org/10.1007/978-1-4419-7374-0_30
Merikangas, K. R., Zhang, H., Avenevoli, S., Acharyya, S., Neuenschwander, M., & Angst, J. (2003). Longitudinal trajectories of depression and anxiety in a prospective community study. Archives of General Psychiatry, 60(10), 993–1000. https://doi.org/10.1001/archpsyc.60.9.993
Mossakowski, K. N. (2011). Unfulfilled expectations and symptoms of depression among young adults. Social Science & Medicine, 73(5), 729–7363. https://doi.org/10.1016/j.socscimed.2011.06.021
Nguyen, M. T., Chan, W. Y., & Keeler, C. (2015). The association between self-rated mental health status and total health care expenditure: A cross-sectional analysis of a nationally representative sample. Medicine, 94(35), e1410. https://doi.org/10.1097/MD.0000000000001410
Palis, H., Marchand, K., & Oviedo-Joekes, E. (2018). The relationship between sense of community belonging and self-rated mental health among Canadians with mental or substance use disorders. Journal of Mental Health, 29(2), 168–175. https://doi.org/10.1080/09638237.2018.1437602
Population Research Laboratory. (2015). Edmonton Area Survey, 1983 [Code book]. University of Alberta Libraries Dataverse, V3. https://doi.org/10.7939/DVN/10582
Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. https://doi.org/10.1177/014662167700100306
Ramiz, L., Contrand, B., Castro, M. Y. R., Dupuy, M., Lu, L., Sztal-Kutas, C., & Lagarde, E. (2021). A longitudinal study of mental health before and during COVID-19 lockdown in the French population. Globalization and Health, 17, 29. https://doi.org/10.1186/s12992-021-00682-8
Roberts, R. E., Lewinsohn, P. M., & Seeley, J. R. (1993). A brief measure of loneliness suitable for use with adolescents. Psychological Reports, 72(3_suppl), 1379–1391. https://doi.org/10.2466/pr0.1993.72.3c.1379
Robins, L. N., Helzer, J. E., Croughan, J. L., & Ratcliff, K. S. (1981). National Institute of Mental Health Diagnostic Interview Schedule: Its history, characteristics, and validity. Archives of General Psychiatry, 38(4), 381–389. https://doi.org/10.1001/archpsyc.1981.01780290015001
Sawatzky, R., Ratner, P. A., Johnson, J. L., Kopec, J. A., & Zumbo, B. D. (2010). Self-reported physical and mental health status and quality of life in adolescents: A latent variable mediation model. Health and Quality of Life Outcomes, 8, 17. https://doi.org/10.1186/1477-7525-8-17
Schlomer, G. L., Bauman, S., & Card, N. A. (2010). Best practices for missing data management in counseling psychology. Journal of Counseling Psychology, 57(1), 1–10. https://doi.org/10.1037/a0018082
Schulenberg, J. E., Sameroff, A. J., & Cicchetti, D. (2004). The transition to adulthood as a critical juncture in the course of psychopathology and mental health. Development and Psychopathology, 16(4), 799–806. https://doi.org/10.1017/S0954579404040015
Shanahan, M. J. (2000). Pathways to adulthood in changing societies: Variability and mechanisms in life course perspective. Annual Review of Sociology, 26, 667–692. https://doi.org/10.1146/annurev.soc.26.1.667
Sheikh, J. I., & Yesavage, J. A. (1986). Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. Clinical Gerontologist: The Journal of Aging and Mental Health, 5(1–2), 165–173. https://doi.org/10.1300/J018v05n01_09
Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. https://doi.org/10.1001/archinte.166.10.1092
Su, Y., D’Arcy, C., Caron, J., & Meng, X. (2021). Increased income over time predicts better self-perceived mental health only at a population level but not for individual changes: An analysis of a longitudinal cohort using cross-lagged models. Journal of Affective Disorders, 292, 487–495. https://doi.org/10.1016/j.jad.2021.05.118
Tanner, J. L., Reinherz, H. Z., Beardslee, W. R., Fitzmaurice, G. M., Leis, J. A., & Berger, S. R. (2007). Change in prevalence of psychiatric disorders from ages 21 to 30 in a community sample. Journal of Nervous and Mental Disease, 195(4), 298–306. https://doi.org/10.1097/01.nmd.0000261952.13887.6e
Wang, P. S., Berglund, P., Olfson, M., Pincus, H. A., Wells, K. B., & Kessler, R. C. (2005). Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 603–613. https://doi.org/10.1001/archpsyc.62.6.603
Wittchen, H. U., & Pfister, H. (1997). DIA-X interviews (M-CIDI): Manual fur screening - Verfahren und interview. Swets & Zeitlinger.
Zuvekas, S. H., & Fleishman, J. A. (2008). Self-rated mental health and racial/ethnic disparities in mental health service use. Medical Care, 46(9), 915–923. https://doi.org/10.1097/MLR.0b013e31817919e5
Acknowledgements
Data were collected by the Population Research Laboratory, University of Alberta.
Funding
This research was funded by grants from the Social Sciences and Humanities Research Council of Canada, Alberta Advanced Education, and the University of Alberta.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors have no relevant financial or non-financial interests to disclose.
Ethics Approval
Ethics approval was obtained for all waves of this study from the University of Alberta (most recent approval was granted June 2017; Pro00074272; “Transitions to midlife: 32 year follow-up of the class of 1985”). Informed consent was obtained for all individuals participating at each wave.
Data availability
The data used in the analyses for the current study are available from the corresponding author on reasonable request.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Galambos, N.L., Johnson, M.D. & Krahn, H.J. Self-rated mental health in the transition to adulthood predicts depressive symptoms in midlife. Curr Psychol 42, 30223–30234 (2023). https://doi.org/10.1007/s12144-022-04081-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-022-04081-z