Abstract
Objectives
To determine the role of mean platelet volume (MPV) and uric acid levels in the diagnosis of neonatal sepsis (NS).
Methods
A total of 146 newborns with suspected NS were prospectively included in the study and infants without NS (n = 142) were assigned as controls. The patients were divided into three groups: Group I (n = 64): clinical NS, Group II (n = 82): culture-proven NS, and Group III (n = 142): healthy controls.
Results
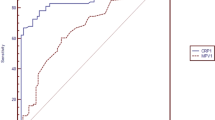
The patients in Group II had the highest C-reactive protein (CRP) levels (54.6 ± 5.4 mg/L), lowest platelet counts (199,329 ± 135,952/mm3) and lowest uric acid levels (2.6 ± 1.8 mg/dL) when compared to Groups I and III (p < 0.05, for all comparisons). MPV values were higher in Group I (10.6 ± 1.1 fL) and Group II (10.4 ± 0.9 fL) when compared to Group III (9.2 ± 1.2 fL) (p = 0.001), although there was no difference between Groups I and II. Area under curve (AUC) values for CRP, MPV, and uric acid were 0.92 (p = 0.001), 0.76 (p = 0.001) and 0.28 (p = 0.001), respectively. The diagnostic cut-off values for CRP and MPV were 9.5 mg/dL and 10.4 fL. Sensitivity and specificity of MPV in NS were 54 % and 82 % respectively. When combined with CRP its sensitivity and specificity increased to 89 % and 79 % respectively.
Conclusions
The combined use of CRP and MPV should be considered in the early diagnosis of NS, but uric acid levels may only be utilized as an additional tool to support diagnosis. CRP is shown to be more sensitive and specific than MPV and uric acid in diagnosing neonatal sepsis.

Similar content being viewed by others
References
Edwards MS, Baker CJ. Sepsis in the newborn. In: Gershon AA, Hotez PJ, Katz SL, eds. Krugman’s Infectious Diseases of Children. 11th ed. Philadelphia: Mosby; 2004. pp. 545–61.
Weinberg GA, Powel KR. Laboratory aids for diagnosis of neonatal sepsis. In: Remington JS, Klein JO, eds. Infectious Diseases of the Fetus and Newborn Infant. Philadelphia: WB Saunders; 2001. pp. 1327–44.
Meem M, Modak JK, Mortuza R, Morshed M, Islam MS, Saha SK. Biomarkers for diagnosis of neonatal infections: a systematic analysis of their potential as a point-of-care diagnostics. J Glob Health. 2011;1:201–9.
Sola-Visner M, Sallmon H, Brown R. New insights into the mechanisms of nonimmune thrombocytopenia in neonates. Semin Perinatol. 2009;33:43–51.
Guida JD, Kunig AM, Leef KH, McKenzie SE, Paul DA. Platelet count and sepsis in very low birth weight neonates: Is there an organism-specific response? Pediatrics. 2003;111:1411–5.
Patrick CH, Lazarchick J. The effect of bacteremia on automated platelet measurements in neonates. Am J Clin Pathol. 1990;93:391–4.
Kapoor K, Basu S, Das BK, Bhatia BD. Lipid peroxidation and antioxidants in neonatal septicemia. J Trop Pediatr. 2006;52:372–5.
Dilli D, Oğuz ŞS, Dilmen U, Köker MY, Kızılgün M. Predictive values of neutrophil CD64 expression compared with interleukin-6 and C-reactive protein in early diagnosis of neonatal sepsis. J Clin Lab Anal. 2010;24:363–70.
Gyawali N, Sanjana RK. Bacteriological profile and antibiogram of neonatal septicemia. Indian J Pediatr. 2013;80:371–4.
Eshwara VK, Sasi A, Munim F, Purkayastha J, Lewis LE, Mukhopadhyay C. Neonatal meningitis and sepsis by chryseobacterium indologenes: a rare and resistant bacterium. Indian J Pediatr. 2013. doi:10.1007/s12098-013-1040-9.
Hofer N, Zacharias E, Müller W, Resch B. An update on the use of C-reactive protein in early-onset neonatal sepsis: Current insights and new tasks. Neonatology. 2012;102:25–36.
Roberts I, Murray NA. Neonatal thrombocytopenia: Causes and management. Arch Dis Child Fetal Neonatal Ed. 2003;88:359–64.
Kaufman D. Fungal infection in the very low birthweight infant. Curr Opin Infect Dis. 2004;17:253–9.
Benjamin Jr DK, Ross K, McKinney Jr RE, Benjamin DK, Auten R, Fisher RG. When to suspect fungal infection in neonates: A clinical comparison of Candida albicans and Candida parapsilosis fungemia with coagulase negative staphylococcal bacteremia. Pediatrics. 2000;106:712–8.
Ververidis M, Kiely EM, Spitz L, Drake DP, Eaton S, Pierro A. The clinical significance of thrombocytopenia in neonates with necrotizing enterocolitis. J Pediatr Surg. 2001;36:799–803.
Scheifele DW, Olsen EM, Pendray MR. Endotoxinemia and thrombocytopenia during neonatal necrotizing enterocolitis. Am J Clin Pathol. 1985;83:227–9.
O’Connor TA, Ringer KM, Gaddis ML. Mean platelet volume during coagulase-negative staphylococcal sepsis in neonates. Am J Clin Pathol. 1993;99:69–71.
Cekmez F, Tanju IA, Canpolat FE, Aydinoz S, Aydemir G, Karademir F, et al. Mean platelet volume in very preterm infants: A predictor of morbidities? Eur Rev Med Pharmacol Sci. 2013;17:134–7.
Giannaki G, Rizos D, Xyni K, Sarandakou A, Protonotariou E, Phocas I, et al. Serum soluble E- and L-selectin in the very early neonatal period. Early Hum Dev. 2000;60:149–55.
Victor VM, Rocha M, Esplugues JV, De la Fuente M. Role of free radicals in sepsis: Antioxidant therapy. Curr Pharm Des. 2005;11:3141–58.
Sanodze NE, Sanikidze TV, Uberi NP, Zhvaniia MA. Role of oxygen-nitrogen stress in neonatal sepsis. Georgian Med News. 2006;133:78–81.
Yang KD, Chen MZ, Teng RJ, Yang MY, Liu HC, Chen RF, et al. A model to study antioxidant regulation of endotoxemia-modulated neonatal granulopoiesis and granulocyte apoptosis. Pediatr Res. 2000;48:829–34.
Batra S, Kumar R, Kapoor AK, Ray G. Alterations in antioxidant status during neonatal sepsis. Ann Trop Paediatr. 2000;20:27–33.
Hooman N, Mehrazma M, Nakhaii S, Otukesh H, Moradi-Lakeh M, Dianati-Maleki N, et al. The value of srum uric acid as a mortality prediction in critically ill children. Iran J Pediatr. 2010;20:323–9.
Contributions
BA, DD, AZ: Concept and design, data analysis and interpretation, manuscript preparation, revision and final approval; NK, SB, NO; Concept and design, collection of data, manuscript preparation, revision and final approval. NO will act as guarantor for this paper.
Conflict of Interest
None.
Role of Funding Source
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aydın, B., Dilli, D., Zenciroğlu, A. et al. Mean Platelet Volume and Uric Acid Levels in Neonatal Sepsis. Indian J Pediatr 81, 1342–1346 (2014). https://doi.org/10.1007/s12098-014-1417-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-014-1417-4