Abstract
Objective
The objective of this study was to determine whether there there are any associations between time of admission and mortality rates in the pediatric intensive care unit.
Methods
We analyzed retrospectively 210 consecutive admissions to the PICU from November 2005 to April 2006 for patients aged 1 mth to 18 yr.
Results
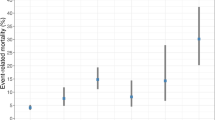
There was no significant difference for overall mortality rates between weekend and weekday admissions (12.2% vs 17.4%, p=0.245), and daytime and evening admissions (11.3 % vs 15.4%, p=0.254). There was also no significant difference between different admission times for within 24 hours, 48 hours and 72 hours mortality rates.
Conclusions
In respect of the overall mortality rates, it can be said that in a closed system PICU management under the control of a pediatric intensivist there is no association between time of admission and mortality rates.
Similar content being viewed by others
References
Carmel S, Rowan K. Variation in intensive care unit outcomes: a search for the evidence on organizational factors. Curr Opin Crit Care 2001; 7: 284–296.
Blunt MC, Burchett KR. Out of hours consultant cover and case-mix-adjusted mortality in intensive care. Lancet 2000; 356: 735–736.
Goh AY, Lum LC, Abdel-Latif ME. Impact of 24 hour critical care physician staffing on case-mix adjusted mortality in paediatric intensive care. Lancet 2001; 357: 445–446.
Carson SS, Stocking C, Podsadecki T, Christenson J, Pohlman A, MacRae S et al. Effects of organizational change in the medical intensive care unit of a teaching hospital: a comprasion of “open” and “closed” formats. J Am Med Assoc 1996; 276: 322–328.
Stephansson O, Dickman PW, Johansson ALV, Kieler H, Cnattingius S. Time of birth and risk of intrapartum and early neonatal death. Epidemiology 2003; 14: 218–222.
Hamilton P, Restrepo E. Weekend birth and higher neonatal mortality: a problem of patient acuity or quality of care? J Obstet Gynecol Neonatal Nurs 2003; 32: 724–733
Domenighetti G, Paccaud F. The night—a dangerous time to be born? Br J Obstet Gynaecol 1986; 12: 1262–1267.
Hendry RA. The weekend—a dangerous time to be born? Br J Obstet Gynaecol 1981; 88: 1200–1203.
Morales IJ, Peters SG, Afessa B. Hospital mortality rate and length of stay in patients admitted at night to the intensive care unit. Crit Care Med 2003; 31: 858–863.
Wunsch H, Mapstone J, Brady T, Hanks R, Rowan K. Hospital mortality associated with day and time of admission o intensive care units. Intensive Care Med 2004; 30: 895–901.
Barnett MJ, Kaboli PJ, Sirio CA et al. Day of the week of intensive care admission and patient outcomes: A multisite regional evaluation. Med Care 2002; 40: 530–539.
Bell CM, Redelmeier DA. Mortality among patients admitted to hospital on weekends as compared with weekdays. N Engl J Med 2001; 345: 663–668.
Hixson ED, Davis S, Morris S, Harrison AM. Do weekends or evenings matter in a pediatric intensive care unit? Pediatr Crit Care Med 2005; 6: 523–530.
Arias Y, Taylor DS, Marcin JP. Association between evening admission and higher mortality rates in the pediatric intensive care unit. Pediatrics 2004; 113: 530–534.
Slater A, Shann F, Pearson G. Pediatric Index of Mortality (PIM) Study Group. PIM2: a revised version of the pediatric index of mortality. Intensive Care Med 2003; 29: 278–285.
Hosmer DW, Lemeshow S. Applied Loistic Regression. 2nd ed. New York; Wiley, 2000.
Fogelholm R, Murros K, Rissanen A, Ilmavirta M. Factors delaying hospital admission after acute stroke. Stroke 1996; 27: 398–400.
Ottesen MM, Kober L, Jorgensen S, Topr-Pedersen C. Determinanats of delay between symptoms and hospital admission in 5978 patients with myocardial infarction. Eur Heart J 1996; 17: 429–437.
Mitra AK, Rahman MM, Fuchs GJ. Risk factors and gender differentials for death among children hospitalized with diarrhoea in Bangladesh. J Health Popul Nutr 2000; 18: 151–156.
Turkey Demographic and Health Survey TDHS-2003. Hacettepe University institute of population studies. http://www.hips.hacettepe.edu.tr/tnsa2003eng
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Arslankoylu, A.E., Bayrakci, B. & Oymak, Y. Admission time and mortality rates. Indian J Pediatr 75, 691–694 (2008). https://doi.org/10.1007/s12098-008-0130-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-008-0130-6