Abstract
Among survivor’s patients with cancer, sexual dysfunction (SD) is a common treatment-related disturbance that significantly affects their quality of life. The disorder can be a short-term effect, but frequently it can be permanent and patients often do not receive adequate support to overcome the problem. The characteristics of SD may differ depending on the type of neoplasm and oncological treatment. The most common long-term effects are those related to treatment-induced menopause, ablative oncologic surgery, and altered gonadal function. Breast, prostate, and gynecologic cancers are the tumors most commonly associated with disturbances in sexual health, although there is evidence of SD in patients with other types of neoplasms. It is necessary for the healthcare team caring for oncological patients to be aware of the characteristics of sexual dysfunction in this population. This will make it possible to offer patients a comprehensive and personalized approach to improve their quality of life.
Similar content being viewed by others
Data availability
Not applicable.
References
Krouwel EM, Albers LF, Nicolai MPJ, Putter H, Osanto S, Pelger RCM, et al. Discussing sexual health in the medical oncologist’s practice: exploring current practice and challenges. J Cancer Educ. 2020;35(6):1072–88.
Carter J, Lacchetti C, Andersen BL, Barton DL, Bolte S, Damast S, et al. Journal of clinical oncology. J Clin Oncol. 2017;36:492–511. https://doi.org/10.1200/JCO.2017.
Walker LM, Wiebe E, Turner J, Driga A, Andrews-Lepine E, Ayume A, et al. The oncology and sexuality, intimacy, and survivorship program model: an integrated, multi-disciplinary model of sexual health care within oncology. J Cancer Educ. 2021;36(2):377–85.
Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Piñeros M, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144(8):1941–53.
Sánchez F, Pérez Conchillo M, Borrás Valls JJ, Gómez Llorens O, Aznar Vicentee J. Caballero Martín de las Mulas A. Diseño y validación del cuestionario de función sexual de la Mujer (FSM). Aten Primaria. 2004;34(6):286–94.
Bober SL, Varela VS. Sexuality in adult cancer survivors: challenges and intervention. J Clin Oncol. 2012;30(30):3712–9.
Figueroa-Martín L, Duarte-Clíments G, Sánchez-Gómez MB, Ruyman B-B. Abordaje de la sexualidad en atención primaria: ¿qué valorar? Ene. 2015. https://doi.org/10.4321/S1988-348X2015000200006.
Lewis RW, Fugl-Meyer KS, Bosch R, Fugl-Meyer AR, Laumann EO, Lizza E, et al. Epidemiology/risk factors of sexual dysfunction. J Sex Med. 2004;1(1):35–9.
Cakar B, Karaca B, Uslu R. Sexual dysfunction in cancer patients: a review. J Buon. 2013;18(4):818–23.
McCabe MP, Sharlip ID, Lewis R, Atalla E, Balon R, Fisher AD, et al. Incidence and prevalence of sexual dysfunction in women and men: a consensus statement from the fourth international consultation on sexual medicine 2015. J Sex Med. 2016;13(2):144–52.
Salter CA, Mulhall JP. Oncosexology. Urol Clin North Am. 2021;48(4):591–602.
Lovelace DL, McDaniel LR, Golden D. Long-term effects of breast cancer surgery, treatment, and survivor care. J Midwifery Womens Health. 2019;64(6):713–24.
Stulz A, Lamore K, Montalescot L, Favez N, Flahault C. Sexual health in colon cancer patients: a systematic review. Psychooncology. 2020;29(7):1095–104.
Tramacere F, Lancellotta V, Casà C, Fionda B, Cornacchione P, Mazzarella C, et al. Assessment of sexual dysfunction in cervical cancer patients after different treatment modality: a systematic review. Medicina. 2022;58(9):1223.
Celentano V, Cohen R, Warusavitarne J, Faiz O, Chand M. Sexual dysfunction following rectal cancer surgery. Int J Colorectal Dis. 2017;32(11):1523–30.
Jackson SE, Wardle J, Steptoe A, Fisher A. Sexuality after a cancer diagnosis: a population-based study. Cancer. 2016;122(24):3883–91.
Wallington DG, Holliday EB. Preparing patients for sexual dysfunction after radiation for anorectal cancers: a systematic review. Pract Radiat Oncol. 2021;11(3):193–201.
Sánchez-Sánchez F, Ferrer-Casanova C, Ponce-Buj B, Sipán-Sarrión Y, Jurado-López AR, San Martin-Blanco C, et al. Design and validation of a male sexual function questionnaire. SEMERGEN. 2020;46(7):441–7.
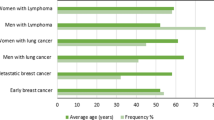
Ospina Serrano AV, Maximiano C, de Sanchez CBI, Torrente M, Mendez M, Sanchez JC, et al. Sexual dysfunction in patients with cancer: Results from the CLARIFY project. J Clin Oncol. 2023;41(16):12094–12094.
Shifren JL, Monz BU, Russo PA, Segreti A, Johannes CB. Sexual problems and distress in United States women. Obstet Gynecol. 2008;112(5):970–8.
Basson R. Sexual desire and arousal disorders in women. N Engl J Med. 2006;354(14):1497–506.
Sousa Rodrigues Guedes T, Barbosa Otoni Gonçalves Guedes M, de Castro Santana R, Costa da Silva JF, Almeida Gomes Dantas A, Ochandorena-Acha M, et al. Sexual Dysfunction in Women with Cancer: A Systematic Review of Longitudinal Studies. Int J Environ Res Public Health. 2022; 19(19).
Rodrigues-Machado N, Quintana MJ, Gómez-Gómez R, Bonfill-Cosp X. Sexual function in women with breast cancer: an evidence map of observational studies. Int J Environ Res Public Health. 2022;19(21):13976.
Jing L, Zhang C, Li W, Jin F, Wang A. Incidence and severity of sexual dysfunction among women with breast cancer: a meta-analysis based on female sexual function index. Support Care Cancer. 2019;27(4):1171–80.
Clayton AH, Valladares Juarez EM. Female sexual dysfunction. Med Clin North Am. 2019;103(4):681–98.
Gozzi E, La Manna AR, Rossi L, Colonna M, Ulgiati MA, Romagnoli L, et al. What hides beneath the scar: sexuality and breast cancer what women don’t say: a single-center study. Clin Ter. 2022;173(4):342–6.
Fingeret MC, Teo I, Epner DE. Managing body image difficulties of adult cancer patients: Lessons from available research. Cancer. 2014;120(5):633–41.
Dusetzina SB, Alexander GC, Freedman RA, Huskamp HA, Keating NL. Trends in co-prescribing of antidepressants and tamoxifen among women with breast cancer, 2004–2010. Breast Cancer Res Treat. 2013;137(1):285–96.
Bober SL, Reese JB, Barbera L, Bradford A, Carpenter KM, Goldfarb S, et al. How to ask and what to do. Curr Opin Support Palliat Care. 2016;10(1):44–54.
Sarna L. Women with lung cancer: impact on quality of life. Qual Life Res. 1993;2(1):13–22.
Duma N, Acharya R, Wei Z, Seaborne L, Heisler C, Fidler MJ, et al. MA14.04 sexual health assessment in women with lung cancer (SHAWL) study. J Thorac Oncol. 2022;17(9):93–4.
Basson R. Women’s sexual dysfunction: revised and expanded definitions. Can Med Assoc J. 2005;172(10):1327–33.
Tiefer L. A new view of women’s sexual problems: why new? Why now? J Sex Res. 2001;38(2):89–96.
Cella D, Yount S, Rothrock N, Gershon R, Cook K, Reeve B, et al. The patient-reported outcomes measurement information system (PROMIS). Med Care. 2007;45(5):S3-11.
Huyghe E, Sui D, Odensky E, Schover LR. Needs assessment survey to justify establishing a reproductive health clinic at a comprehensive cancer center. J Sex Med. 2009;6(1):149–63.
Rosen CBJHSLR. The female sexual function index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26(2):191–208.
Flynn KE, Lin L, Cyranowski JM, Reeve BB, Reese JB, Jeffery DD, et al. Development of the NIH PROMIS® sexual function and satisfaction measures in patients with cancer. J Sex Med. 2013;10(Supplement_1):43–52.
Maiorino MI, Chiodini P, Bellastella G, Giugliano D, Esposito K. Sexual dysfunction in women with cancer: a systematic review with meta-analysis of studies using the female sexual function index. Endocrine. 2016;54(2):329–41.
Johannes CB, Araujo AB, Feldman HA, Derby CA, Kleinman KP, McKinlay JB. Incidence of erectile dysfunction in men 40 to 69 years old: longitudinal results from the Massachusetts male aging study. J Urol. 2000;163(2):460–3.
Rosen RC, Fisher WA, Eardley I, Niederberger C, Nadel A, Sand M. The multinational men’s attitudes to life events and sexuality (MALES) study: I. Prevalence oSf erectile dysfunction and related health concerns in the general population. Curr Med Res Opin. 2004;20(5):607–17.
Schover LR. Sexual quality of life in men and women after cancer. Climacteric. 2019;22(6):553–7.
Loi M, Wortel RC, Francolini G, Incrocci L. Sexual function in patients treated with stereotactic radiotherapy for prostate cancer: a systematic review of the current evidence. J Sex Med. 2019;16(9):1409–20.
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49(6):822–30.
Thomas HN, Thurston RC. A biopsychosocial approach to women’s sexual function and dysfunction at midlife: a narrative review. Maturitas. 2016;87:49–60.
Barbera L, Zwaal C, Elterman D, McPherson K, Wolfman W, Katz A, et al. Interventions to address sexual problems in people with cancer. Curr Oncol. 2017;24(3):192–200.
Carter J, Lacchetti C, Andersen BL, Barton DL, Bolte S, Damast S, et al. Interventions to address sexual problems in people with cancer: American society of clinical oncology clinical practice guideline adaptation of cancer care ontario guideline. J Clin Oncol. 2018;36(5):492–511.
Stephenson RA, Mori M, Hsieh YC, Beer TM, Stanford JL, Gilliland FD, et al. Treatment of erectile dysfunction following therapy for clinically localized prostate cancer: patient reported use and outcomes from the surveillance, epidemiology, and end results prostate cancer outcomes study. J Urol. 2005;174(2):646–50.
Pang K, Pan D, Xu H, Ma Y, Wang J, Xu P, et al. Advances in physical diagnosis and treatment of male erectile dysfunction. Front Physiol. 2023;9:13.
Montorsi F, Padma-Nathan H, Glina S. Erectile function and assessments of erection hardness correlate positively with measures of emotional well-being, sexual satisfaction, and treatment satisfaction in men with erectile dysfunction treated with sildenafil citrate (Viagra®). Urology. 2006;68(3):26–37.
Schover LR, Fouladi RT, Warneke CL, Neese L, Klein EA, Zippe C, et al. The use of treatments for erectile dysfunction among survivors of prostate carcinoma. Cancer. 2002;95(11):2397–407.
Miller DC, Wei JT, Dunn RL, Montie JE, Pimentel H, Sandler HM, et al. Use of medications or devices for erectile dysfunction among long-term prostate cancer treatment survivors: potential influence of sexual motivation and/or indifference. Urology. 2006;68(1):166–71.
Brotto LA, Yule M, Breckon E. Psychological interventions for the sexual sequelae of cancer: a review of the literature. J Cancer Surviv. 2010;4(4):346–60.
Carter J, Goldfrank D, Schover LR. Simple strategies for vaginal health promotion in cancer survivors. J Sex Med. 2011;8(2):549–59.
Denlinger CS, Carlson RW, Are M, Baker KS, Davis E, Edge SB, et al. Survivorship: sexual dysfunction (Female), version 1.2013. J Natl Compr Cancer Netw. 2014;12(2):184–92.
Caruso S, Intelisano G, Farina M, Di Mari L, Agnello C. The function of sildenafil on female sexual pathways: a double-blind, cross-over, placebo-controlled study. Eur J Obstet Gynecol Reprod Biol. 2003;110(2):201–6.
Caruso S, Intelisano G, Lupo L, Agnello C. Premenopausal women affected by sexual arousal disorder treated with sildenafil: a double-blind, cross-over, placebo-controlled study. BJOG. 2001;108(6):623–8.
Lindau ST, Gavrilova N. Sex, health, and years of sexually active life gained due to good health: evidence from two US population based cross sectional surveys of ageing. BMJ. 2010;340(mar09 2):c810–c810.
Ratner ES, Foran KA, Schwartz PE, Minkin MJ. Sexuality and intimacy after gynecological cancer. Maturitas. 2010;66(1):23–6.
Bernard S, Tandon P, Waters A, Selmani S, Wiebe E, Turner J, et al. Preferences, barriers and facilitators regarding virtual pelvic healthcare in individuals with gynaecological cancers: protocol for a patient-oriented, mixed-methods study. BMJ Open. 2023;13(1): e067606.
Venkataramu V, Ghotra H, Chaturvedi S. Management of psychiatric disorders in patients with cancer. Indian J Psychiatry. 2022;64(8):458.
Arthur EK, Menon U, Reese JB, Browning K, Overcash J, Rose K, et al. Profiles of women’s adjustment after cancer based on sexual and psychosocial wellbeing: results of a cluster analysis. BMC Cancer. 2022;22(1):1003.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
AVO reports consultant fees from AstraZeneca, Bristol Myers Squibb Company, Pfizer, Merck, Takeda Oncology and Roche; and support for attending meetings and/or travel from Pfizer, Roche, MSD, and Janssen.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ospina Serrano, A.V. Overview of sexual dysfunction in patients with cancer. Clin Transl Oncol 25, 3369–3377 (2023). https://doi.org/10.1007/s12094-023-03311-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-023-03311-5