Abstract
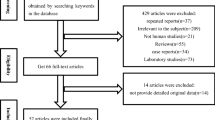
Pharyngocutaneous fistula is the leading complication following total laryngectomy. It delays complementary treatments, speech rehabilitation and oral feeding. Despite evolving medical care, fistula incidence remains high. There is no consensus regarding which patients are at higher risk for fistula development. This article comprised a literature review about risk factors for fistula development. All articles published on an on-line database (PUBMED™) using MESH terms “larynx cancer” and “fistula” in a 5-year period (January 1st, 2014 to January 27th, 2019) were included. Further articles were selected due to expert suggestion by one of the senior surgeons. Only articles written in Portuguese or English were included. Animal studies were excluded. 151 articles were selected and abstracts analysed. 82 articles were selected for full text revision. 32 were later excluded because they described single clinical cases, experimental surgical technics, irrelevant data or poor methodology. Final selection comprised 50 studies: 9 systematic reviews, one non-systematic review, 34 unicentric and 4 multicentric retrospective analysis and two prospective studies. There is no consensus regarding risk factors for fistula development. Patients submitted to salvage surgery for advanced disease seem to be at greater risk. Bad nutritional status is a logical contributor, but the ideal surrogate marker is still missing. Several variables are inconsistently pointed as risk factors and should be abandoned unless proved otherwise. There are no standard scores for fistula occurrence despite being a common complication following surgery.
Similar content being viewed by others
References
Cecatto SB, Soares MM, Henriques T, Monteiro E, Moura CIFP (2014) Predictive factors for the postlaryngectomy pharyngocutaneous fistula development: systematic reviewBraz J Otorhinolaryngol 80(2):167–77
Mattioli F, Bettini M, Molteni G, Piccinini A, Valoriani F, Gabriele S et al (2015) Analysis of risk factors for pharyngocutaneous fistula after total laryngectomy with particular focus on nutritional status. Acta Otorhinolaryngol Ital 35(4):243–248
Suzuki S, Yasunaga H, Matsui H, Horiguchi H, Fushimi K, Yamasoba T (2016) Pharyngocutaneous fistula and delay in free oral feeding after pharyngolaryngectomy for hypopharyngeal cancer. Head Neck 38(S1):E625–E630
Scotton WJ, Nixon IJ, Pezier TF, Cobb R, Joshi A, Urbano TG et al (2014) Time interval between primary radiotherapy and Salvage laryngectomy: a predictor of pharyngocutaneous fistula formation. Eur Arch Oto-Rhino-Laryngology 271(8):2277–2283
Lebo NL, Caulley L, Alsaffar H, Corsten MJ, Johnson-Obaseki S (2017) Peri-operative factors predisposing to pharyngocutaneous fistula after total laryngectomy: Analysis of a large multi-institutional patient cohort. J Otolaryngol - Head Neck Surg 46(1):1–8
Sugiyama N, Takao S, Suzuki E, Kimata Y (2017) Risk factors for wound complications in head and neck reconstruction: 773 free jejunal reconstruction procedures after total pharyngolaryngoesophagectomy. Head Neck 39(10):2057–2069
Lansaat L, van der Noort V, Bernard SE, Eerenstein SEJ, Plaat BEC, Langeveld TAPM et al (2018) Predictive factors for pharyngocutaneous fistulization after total laryngectomy: a Dutch Head and Neck Society audit. Eur Arch Oto-Rhino-Laryngology [Internet] 275(3):783–794
Liang JW, Li ZD, Li SC, Fang FQ, Zhao YJ, Li YG (2015) Pharyngocutaneous fistula after total laryngectomy: a systematic review and meta-analysis of risk factors. Auris Nasus Larynx 42(5):353–359
Timmermans AJ, Lansaat L, Theunissen EAR, Hamming-Vrieze O, Hilgers FJM, Van Den Brekel MWM (2014) Predictive factors for pharyngocutaneous fistulization after total laryngectomy. Ann Otol Rhinol Laryngol 123(3):153–161
Šifrer R, Aničin A, Pohar MP, Žargi M, Pukl P, Soklič T et al (2016) Pharyngocutaneous fistula: the incidence and the risk factors. Eur Arch Oto-Rhino-Laryngology 273(10):3393–3399
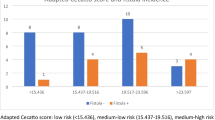
Cecatto SB, Monteiro-Soares M, Henriques T, Monteiro E, Moura CIFP (2015) Derivation of a clinical decision rule for predictive factors for the development of pharyngocutaneous fistula postlaryngectomy. Braz J Otorhinolaryngol 81(4):394–401
Dedivitis RA, Aires FT, Cernea CR, Brandão LG (2015) Pharyngocutaneous fistula after total laryngectomy: Systematic review of risk factors. Head Neck 37(11):1691–1697
Casasayas M, Sansa A, García-Lorenzo J, López M, Orús C, Peláez X et al (2019) Pharyngocutaneous fistula after total laryngectomy: multivariate analysis of risk factors and a severity-based classification proposal. Eur Arch Oto-Rhino-Laryngology 276(1):143–151
Benson EM, Hirata RM, Thompson CB, Ha PK, Fakhry C, Saunders JR et al (2015) Pharyngocutaneous fistula after total laryngectomy: a single-institution experience, 2001–2012. Am J Otolaryngol 36(1):24–31
Busoni M, Deganello A, Gallo O (2015) Fistola faringocutanea dopo laringectomia totale: Analisi dei fattori di rischio, della prognosi e delle modalità di trattamento. Acta Otorhinolaryngol Ital 35(6):400–405
Morton RP, Mehanna H, Hall FT, McIvor NP (2007) Prediction of pharyngocutaneous fistulas after laryngectomy. Otolaryngol - Head Neck Surg 136(4 SUPPL.):46–49
Kim YH, Roh JL, Choi SH, Nam SY, Kim SY (2019) Prediction of pharyngocutaneous fistula and survival after salvage laryngectomy for laryngohypopharyngeal carcinoma. Head Neck 41(9):3002–3008
Knuf KM, Maani CV, Cummings AK (2018) Clinical agreement in the American society of anesthesiologists physical status classification. Perioper Med 7(1):1–6
Sayles M, Grant DG (2014) Preventing pharyngo-cutaneous fistula in total laryngectomy: A systematic review and meta-analysis. Laryngoscope 124(5):1150–1163
Kiliç C, Tuncel U, Cömert E (2015) Pharyngocutaneous fistulae after total laryngectomy: analysis of the risk factors and treatment approaches. B-ENT 11(2):95–100
Bozkurt G, Elhassan HA, Mahmutoğlu AS, Çelebi İ, Mcleod RWJ, Soytaş P et al (2018) Neck muscle mass index as a predictor of post-laryngectomy wound complications. Ann Otol Rhinol Laryngol 127(11):841–847
Piccirillo JF, Lacy PD, Basu A, Spitznagel EL (2002) Development of a new head and neck cancer-specific comorbidity index. Arch Otolaryngol - Head Neck Surg 128(10):1172–1179
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Süslü N, Senirli RT, Günaydn RÖ, Özer S, Karakaya J, Şefik HA (2015) Pharyngocutaneous fistula after salvage laryngectomy. Acta Otolaryngol 135(6):615–621
Formeister EJ, Sean Alemi A, El-Sayed I, George JR, Ha P, Daniel Knott P et al (2018) Shorter interval between radiation therapy and salvage laryngopharyngeal surgery increases complication rates following microvascular free tissue transfer. Am J Otolaryngol - Head Neck Med Surg 39(5):548–552
Basheeth N, O’Leary G, Sheahan P (2014) Pharyngocutaneous fistula after salvage laryngectomy: Impact of interval between radiotherapy and surgery, and performance of bilateral neck dissection. Head Neck 36(4):580–584
Pezier TF, Nixon IJ, Scotton W, Joshi A, Guerrero-Urbano T, Oakley R et al (2014) Should elective neck dissection be routinely performed in patients undergoing salvage total laryngectomy? J Laryngol Otol 128(3):279–283
Walton B, Vellucci J, Patel PB, Jennings K, McCammon S, Underbrink MP (2018) Post-Laryngectomy stricture and pharyngocutaneous fistula: review of techniques in primary pharyngeal reconstruction in laryngectomy. Clin Otolaryngol 43(1):109–116
Aydin S, Taskin U, Orhan I, Altas B, Ege SS, Yucebas K et al (2014) The impact of pharyngeal repair time and suture frequency on the development of pharyngocutaneous fistula after total laryngectomy. J Craniofac Surg 25(3):775–779
Dedivitis RA, Aires FT, Pfuetzenreiter EG, Castro MAF, Guimarães AV (2014) Stapler suture of the pharynx after total laryngectomy. Acta Otorhinolaryngol Ital 34(2):94–98
Aires FT, Dedivitis RA, Castro MAF, Bernardo WM, Cernea CR, Brandão LG (2014) Efficacy of stapler pharyngeal closure after total laryngectomy: a systematic review. Head Neck [Internet] 36(5):739–742
Ismi O, Unal M, Vayisoglu Y, Yesilova M, Helvaci I, Gorur K et al (2017) Stapler esophageal closure during total laryngectomy. J Craniofac Surg 28(1):e35-40
Guimarães AV, Aires FT, Dedivitis RA, Kulcsar MAV, Ramos DM, Cernea CR et al (2016) Efficacy of pectoralis major muscle flap for pharyngocutaneous fistula prevention in salvage total laryngectomy: a systematic review. Head Neck 38(1):e2317–e2321
Gilbert MR, Sturm JJ, Gooding WE, Johnson JT, Kim S (2014) Pectoralis major myofascial onlay and myocutaneous flaps and pharyngocutaneous fistula in salvage laryngectomy. Laryngoscope 124(12):2680–2686
Gendreau-Lefèvre A-K, Audet N, Maltais S, Thuot F (2015) Prophylactic pectoralis major muscle flap in prevention of pharyngocutaneous fistula in total laryngectomy after radiotherapy. Head Neck 37(9):1233–1238
Paleri V, Drinnan M, Van Den Brekel MWM, Hinni ML, Bradley PJ, Wolf GT et al (2014) Vascularized tissue to reduce fistula following salvage total laryngectomy: A systematic review. Laryngoscope 124(8):1848–1853
Anschütz L, Nisa L, Elicin O, Bojaxhiu B, Caversaccio M, Giger R (2016) Pectoralis major myofascial interposition flap prevents postoperative pharyngocutaneous fistula in salvage total laryngectomy. Eur Arch Oto-Rhino-Laryngol 273(11):3943–3949
Yeh DH, Sahovaler A, Fung K (2017) Reconstruction after salvage laryngectomy. Oral Oncol 75:22–27
Chiesa Estomba CM, González García JA, Sistiaga Suarez JA, Thomas Arrizabalaga I, Larruscain Sarasola E, Altuna MX (2018) Efficacy of the myofascial pectoralis major flap in the reduction of salivary fistulas after salvage total laryngectomy. Acta Otorrinolaringol Esp 69(2):99–104
Sharma S, Chaukar DA, Laskar SG, Kapre N, Deshmukh A, Pai P et al (2016) Role of the pectoralis major myofascial flap in preventing pharyngocutaneous fistula following salvage laryngectomy. J Laryngol Otol 130(9):860–864
Sittitrai P, Srivanitchapoom C, Reunmakkaew D (2018) Prevention of pharyngocutaneous fistula in salvage total laryngectomy: Role of the pectoralis major flap and peri-operative management. J Laryngol Otol 132(3):246–251
Sayles M, Koonce SL, Harrison L, Beasley N, McRae AR, Grant DG (2014) Pharyngo-cutaneous fistula complicating laryngectomy in the chemo-radiotherapy organ-preservation epoch. Eur Arch Oto-Rhino-Laryngology 271(6):1765–1769
Mizrachi A, Zloczower E, Hilly O, Shvero J, Shpitzer T, Feinmesser R et al (2016) The role of pectoralis major flap in reducing the incidence of pharyngocutaneous fistula following total laryngectomy: a single-centre experience with 102 patients. Clin Otolaryngol 41(6):809–812
Cömert E, Tunçel TMT, Kiliç C, Cengiz AB, Sencan Z et al (2014) Pectoralis major myofascial flap in salvage laryngectomy. J Laryngol Otol 128(8):714–719
Aires FT, Dedivitis RA, Petrarolha SMP, Bernardo WM, Cernea CR, Brandão LG (2015) Early oral feeding after total laryngectomy: a systematic review. Head Neck 37(10):1532–1535
Timmermans AJ, Lansaat L, Kroon GVJ, Hamming-Vrieze O, Hilgers FJM, Van Den Brekel MWM (2014) Early oral intake after total laryngectomy does not increase pharyngocutaneous fistulization. Eur Arch Oto-Rhino-Laryngology 271(2):353–358
Süslü N, Şefik HA (2016) Early oral feeding after total laryngectomy: outcome of 602 patients in one cancer center. Auris Nasus Larynx 43(5):546–550
Kishikova L, Fleming JC (2014) Oral feeding following laryngectomy: early or delayed? Int J Surg 12(11):1137–1140. https://doi.org/10.1016/j.ijsu.2014.09.003
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
First author designed the study, collected data and drafted the article. Second and third authors reviewed the draft ans suggested additional references. First author re-wrote the draft till a consensus was reached. All authors approved the final version.
Corresponding author
Ethics declarations
Conflict of Interests
The authors have no relevant financial or non-financial interests to disclose.
Ethics Approval
This is an observational study. No ethical approval was considered necessary.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Penêda, J.F., Fernandes, J. & Monteiro, E. Risk Factors for Pharyngocutaneous Fistula Following Total Laryngectomy. Indian J Otolaryngol Head Neck Surg 75, 485–491 (2023). https://doi.org/10.1007/s12070-022-03311-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-022-03311-x