Abstract
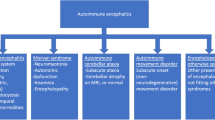
We present a panel of central nervous system (CNS) complications associated with coronavirus disease 2019 (COVID-19) and their clinical characteristics. We aim to investigate associations between neurological autoantibodies and COVID-19 patients with predominant CNS complications. In this retrospective multi-center study, we analyze neurologic complications associated with COVID-19 patients from Dec. 2022 to Feb. 2023 at four tertiary hospitals in China. CSF and/or serum in the enrolled patients were tested for autoantibodies using tissue-based assays (TBAs) and cell-based assays (CBAs). A total of 34 consecutive patients (median age was 40.5 years [range 15–83], 50% were female) were enrolled. CNS syndromes included encephalitis (n=15), encephalopathies (n=6), meningoencephalitis (n=3), ADEM (n=2), depression (n = 2), Alzheimer’s disease (n=2), Parkinson disease (n=1), and central nervous system vasculitis (n=1). Twenty-eight specimens (of 44 tested; 11/27 [40.7%] CSF, 13/17 [76.5%] serums) were confirmed by TBAs to be autoantibodies positive. However, only a few autoantibodies (1 with MOG and 1 with NMDAR) were detected by CBAs assays. Twenty-four patients received immunotherapy. After a mean time of 7.26 months of follow-up, 75.8% (25/33) of patients had good outcome (mRS score ≤2). Although no significant difference was observed between the two groups, the proportion of positive CSF autoantibodies in the poor outcomes group was higher than that in the good outcomes group (57.1% vs 31.5%, P = 0.369). Autoantibodies were frequently observed in COVID-19-associated CNS complications. The identification of these autoantibody-positive COVID-19 cases is important as they respond favorably to immunotherapy.



Similar content being viewed by others
Data Availability
The data sets generated and/or analyzed during the current study are not publicly available but can be obtained by qualified researchers from the corresponding author on reasonable request.
References
Liu J, Liu S (2020) The management of coronavirus disease 2019 (COVID-19). J Med Virol 92(9):1484–1490
Yu L, Wang C, Li X, Wang X, Kang Y, Ma X, Sun R, Sun Y et al (2023) Clinical characteristics of abruptly increased paediatric patients with Omicron BF.7 or BA.5.2 in Beijing. Virol J 20(1):209
Xiong W, Mu J, Guo J, Lu L, Liu D, Luo J, Li N, Liu J et al (2020) New onset neurologic events in people with COVID-19 in 3 regions in China. Neurology 95(11):e1479–e1487
Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, Chang J, Hong C et al (2020) Neurologic manifestations of hospitalized patients with Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol 77(6):683–690
Romero-Sanchez CM, Diaz-Maroto I, Fernandez-Diaz E, Sanchez-Larsen A, Layos-Romero A, Garcia-Garcia J, Gonzalez E, Redondo-Penas I et al (2020) Neurologic manifestations in hospitalized patients with COVID-19: The ALBACOVID registry. Neurology 95(8):e1060–e1070
Misra S, Kolappa K, Prasad M, Radhakrishnan D, Thakur KT, Solomon T, Michael BD, Winkler AS et al (2021) Frequency of neurologic manifestations in COVID-19: a systematic review and meta-analysis. Neurology 97(23):e2269–e2281
Khedr EM, Abo-Elfetoh N, Deaf E, Hassan HM, Amin MT, Soliman RK, Attia AA, Zarzour AA et al (2021) Surveillance study of acute neurological manifestations among 439 Egyptian patients with COVID-19 in Assiut and Aswan University Hospitals. Neuroepidemiology 55(2):109–118
Nersesjan V, Amiri M, Lebech AM, Roed C, Mens H, Russell L, Fonsmark L, Berntsen M et al (2021) Central and peripheral nervous system complications of COVID-19: a prospective tertiary center cohort with 3-month follow-up. J Neurol 268(9):3086–3104
Park J, Kwon YS, Kim HA, Kwon DH, Hwang J, Jang SH, Park H, Sohn SI, Choi HA, Hong JH (2021) Clinical implications of neurological comorbidities and complications in ICU patients with COVID-19. J Clin Med 10(11):2281
Paniz-Mondolfi A, Bryce C, Grimes Z, Gordon RE, Reidy J, Lednicky J, Sordillo EM, Fowkes M (2020) Central nervous system involvement by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). J Med Virol 92(7):699–702
Mina Y, Enose-Akahata Y, Hammoud DA, Videckis AJ, Narpala SR, O'Connell SE, Carroll R, Lin BC, McMahan CC, Nair G et al (2023) Deep phenotyping of neurologic postacute sequelae of SARS-CoV-2 infection. Neurol Neuroimmunol Neuroinflamm 10(4):e200097
Matschke J, Lutgehetmann M, Hagel C, Sperhake JP, Schroder AS, Edler C, Mushumba H, Fitzek A et al (2020) Neuropathology of patients with COVID-19 in Germany: a post-mortem case series. Lancet Neurol 19(11):919–929
Song E, Bartley CM, Chow RD, Ngo TT, Jiang R, Zamecnik CR, Dandekar R, Loudermilk RP et al (2021) Divergent and self-reactive immune responses in the CNS of COVID-19 patients with neurological symptoms. Cell Rep Med 2(5):100288
Meppiel E, Peiffer-Smadja N, Maury A, Bekri I, Delorme C, Desestret V, Gorza L, Hautecloque-Raysz G et al (2021) Neurologic manifestations associated with COVID-19: a multicentre registry. Clin Microbiol Infect 27(3):458–466
Li Z, Lin D, Xu X, Liu X, Zhang J, Huang K, Wang F, Liu J et al (2023) Central nervous system complications in SARS-CoV-2-infected patients. J Neurol 270(10):4617–4631
Aubart M, Roux CJ, Durrleman C, Gins C, Hully M, Kossorotoff M, Gitiaux C, Levy R et al (2022) Neuroinflammatory disease following severe acute respiratory syndrome coronavirus 2 infection in children. J Pediatr 247:22–28.e22
Garg RK, Paliwal VK, Gupta A (2021) Encephalopathy in patients with COVID-19: A review. J Med Virol 93(1):206–222
Venkatesan A, Tunkel AR, Bloch KC, Lauring AS, Sejvar J, Bitnun A, Stahl JP, Mailles A et al (2013) Case definitions, diagnostic algorithms, and priorities in encephalitis: consensus statement of the international encephalitis consortium. Clin Infect Dis 57(8):1114–1128
Sa MJ (2009) Acute transverse myelitis: a practical reappraisal. Autoimmun Rev 9(2):128–131
Pohl D, Alper G, Van Haren K, Kornberg AJ, Lucchinetti CF, Tenembaum S, Belman AL (2016) Acute disseminated encephalomyelitis: Updates on an inflammatory CNS syndrome. Neurology 87(9 Suppl 2):S38–S45
Carbo EC, Blankenspoor I, Goeman JJ, Kroes ACM, Claas ECJ, De Vries JJC (2021) Viral metagenomic sequencing in the diagnosis of meningoencephalitis: a review of technical advances and diagnostic yield. Expert Rev Mol Diagn 21(11):1139–1146
Lim JA, Lee ST, Moon J, Jun JS, Kim TJ, Shin YW, Abdullah S, Byun JI et al (2019) Development of the clinical assessment scale in autoimmune encephalitis. Ann Neurol 85(3):352–358
Graus F, Titulaer MJ, Balu R, Benseler S, Bien CG, Cellucci T, Cortese I, Dale RC et al (2016) A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol 15(4):391–404
Huang L, Yao Q, Gu X, Wang Q, Ren L, Wang Y, Hu P, Guo L et al (2021) 1-year outcomes in hospital survivors with COVID-19: a longitudinal cohort study. Lancet 398(10302):747–758
Hensley MK, Markantone D, Prescott HC (2022) Neurologic manifestations and complications of COVID-19. Annu Rev Med 73:113–127
Rogers JP, Watson CJ, Badenoch J, Cross B, Butler M, Song J, Hafeez D, Morrin H et al (2021) Neurology and neuropsychiatry of COVID-19: a systematic review and meta-analysis of the early literature reveals frequent CNS manifestations and key emerging narratives. J Neurol Neurosurg Psychiatry 92(9):932–941
Kubota T, Kuroda N (2021) Exacerbation of neurological symptoms and COVID-19 severity in patients with preexisting neurological disorders and COVID-19: A systematic review. Clin Neurol Neurosurg 200:106349
Di Nicola M, Pepe M, De Mori L, Ferrara OM, Panaccione I, Sani G (2023) Physical and cognitive correlates, inflammatory levels, and treatment response in post-COVID-19 first-onset vs. recurrent depressive episodes. Eur Arch Psychiatry Clin Neurosci 5(8):1–11
Putri C, Hariyanto TI, Hananto JE, Christian K, Situmeang RFV, Kurniawan A (2021) Parkinson's disease may worsen outcomes from coronavirus disease 2019 (COVID-19) pneumonia in hospitalized patients: A systematic review, meta-analysis, and meta-regression. Parkinsonism Relat Disord 87:155–161
Sakibuzzaman M, Hassan A, Hayee S, Haque FA, Bushra SS, Maliha M, Tania MK, Sadat A et al (2022) Exacerbation of pre-existing neurological symptoms with COVID-19 in patients with chronic neurological diseases: an updated systematic review. Cureus 14(9):e29297
Kantonen J, Mahzabin S, Mayranpaa MI, Tynninen O, Paetau A, Andersson N, Sajantila A, Vapalahti O et al (2020) Neuropathologic features of four autopsied COVID-19 patients. Brain Pathol 30(6):1012–1016
Solomon IH, Normandin E, Bhattacharyya S, Mukerji SS, Keller K, Ali AS, Adams G, Hornick JL (2020) Neuropathological Features of Covid-19. N Engl J Med 383(10):989–992
Franke C, Ferse C, Kreye J, Reincke SM, Sanchez-Sendin E, Rocco A, Steinbrenner M, Angermair S et al (2021) High frequency of cerebrospinal fluid autoantibodies in COVID-19 patients with neurological symptoms. Brain Behav Immun 93:415–419
Moonis G, Filippi CG, Kirsch CFE, Mohan S, Stein EG, Hirsch JA, Mahajan A (2021) The spectrum of neuroimaging findings on CT and MRI in adults With COVID-19. AJR Am J Roentgenol 217(4):959–974
Jeppesen R, Nilsson AC, Sorensen NV, Orlovska-Waast S, Christensen RHB, Benros ME (2023) Antineuronal antibodies in cerebrospinal fluid and serum of 104 patients with psychotic disorders compared to 104 individually matched healthy controls. Schizophr Res 252:39–45
Takekoshi A, Kimura A, Yoshikura N, Yamakawa I, Urushitani M, Nakamura K, Yoshida K, Shimohata T (2023) Clinical features and neuroimaging findings of neuropil antibody-positive idiopathic sporadic ataxia of unknown etiology. Cerebellum 22(5):915–924
Rizk JG, Kalantar-Zadeh K, Mehra MR, Lavie CJ, Rizk Y, Forthal DN (2020) Pharmaco-Immunomodulatory Therapy in COVID-19. Drugs 80(13):1267–1292
Acknowledgements
The authors thank all participants for their participation in our study.
Funding
Supported by the National Natural Science Foundation of China (grants 82371364).
Author information
Authors and Affiliations
Contributions
Jingfang Lin accessed and verified the underlying data reported in the manuscript, literature search, data interpretation and writing; Dong Zheng, Decai Tian, Pei Zheng, Hongya Zhang, Chuo Li and Chunliang Lei carried out the figures, data collection and data analysis; Fudong Shi and Honghao Wang conceptualized and designed the study and revised the manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
The study was approved by the Ethics Committee of Eight people's Hospital of Guangzhou (202115202), Guangzhou. A written informed consent of each participant was obtained from their caregivers at admission prior to enrolment in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary file 1
(DOCX 206 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lin, J., Zheng, D., Tian, D. et al. High Frequency of Autoantibodies in COVID-19 Patients with Central Nervous System Complications: a Multicenter Observational Study. Mol Neurobiol (2024). https://doi.org/10.1007/s12035-024-04109-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12035-024-04109-4