Abstract
Dysregulation of the kynurenine pathway (KP) is believed to play a significant role in neurodegenerative and cognitive disorders. While some evidence links the KP to myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), further studies are needed to clarify the overall picture of how inflammation-driven KP disturbances may contribute to symptomology in ME/CFS. Here, we report that plasma levels of most bioactive KP metabolites differed significantly between ME/CFS patients and healthy controls in a manner consistent with their known contribution to symptomology in other neurological disorders. Importantly, we found that enhanced production of the first KP metabolite, kynurenine (KYN), correlated with symptom severity, highlighting the relationship between inflammation, KP dysregulation, and ME/CFS symptomology. Other significant changes in the KP included lower levels of the downstream KP metabolites 3-HK, 3-HAA, QUIN, and PIC that could negatively impact cellular energetics. We also rationalized KP dysregulation to changes in the expression of inflammatory cytokines and, for the first time, assessed levels of the iron (Fe)-regulating hormone hepcidin that is also inflammation-responsive. Levels of hepcidin in ME/CFS decreased nearly by half, which might reflect systemic low Fe levels or possibly ongoing hypoxia. We next performed a proteomics screen to survey for other significant differences in protein expression in ME/CFS. Interestingly, out of the seven most significantly modulated proteins in ME/CFS patient plasma, 5 proteins have roles in maintaining gut health, which considering the new appreciation of how gut microbiome and health modulates systemic KP could highlight a new explanation of symptomology in ME/CFS patients and potential new prognostic biomarker/s and/or treatment avenues.







Similar content being viewed by others
Data Availability
Data that supports the findings of this study are available from the corresponding authors upon request.
References
Carruthers BM et al (2003) Myalgic encephalomyelitis/chronic fatigue syndrome: clinical working case definition, diagnostic and treatment protocols. J Chronic Fatigue Syndr 11(1):7–115
Close S et al (2020) The economic impacts of myalgic encephalomyelitis/chronic fatigue syndrome in an Australian cohort. Front Public Health 8:420
Kavyani B et al (2022) Could the kynurenine pathway be the key missing piece of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) complex puzzle? Cell Mol Life Sci 79(8):1–19
Lim CK et al (2017) Kynurenine pathway metabolomics predicts and provides mechanistic insight into multiple sclerosis progression. Sci Rep 7(1):1–9
Natelson BH, Haghighi MH, Ponzio NM (2002) Evidence for the presence of immune dysfunction in chronic fatigue syndrome. Clin Vaccine Immunol 9(4):747–752
Heng B et al (2015) Understanding the role of the kynurenine pathway in human breast cancer immunobiology. Oncotarget 7(6):6506–6520
Forsyth LM et al (1999) Therapeutic effects of oral NADH on the symptoms of patients with chronic fatigue syndrome. Ann Allergy Asthma Immunol 82(2):185–191
Guillemin GJ (2012) Quinolinic acid, the inescapable neurotoxin. FEBS J 279(8):1356–1365
Wirthgen E et al (2018) Kynurenic acid: the Janus-faced role of an immunomodulatory tryptophan metabolite and its link to pathological conditions. Front Immunol 8:1957
Wang J et al (2006) Kynurenic acid as a ligand for orphan G protein-coupled receptor GPR35. J Biol Chem 281(31):22021–22028
Grant R, Coggan S, Smythe GA (2009) The physiological action of picolinic acid in the human brain. Int J Tryptophan Res 2:IJTR. S2469
Ying W (2008) NAD+/NADH and NADP+/NADPH in cellular functions and cell death: regulation and biological consequences. Antioxid Redox Signal 10(2):179–206
Badawy AA (2017) Kynurenine pathway of tryptophan metabolism: regulatory and functional aspects. Int J Tryptophan Res 10:1178646917691938
Anderson G, Maes M, Berk M (2012) Biological underpinnings of the commonalities in depression, somatization, and chronic fatigue syndrome. Med Hypotheses 78(6):752–756
Blankfield A (2013) Article Commentary: Kynurenine pathway pathologies: do nicotinamide and other pathway co-factors have a therapeutic role in reduction of symptom severity, including chronic fatigue syndrome (CFS) and fibromyalgia (FM). Int J Tryptophan Res 6:IJTR. S11193
Dehhaghi M et al (2022) The role of kynurenine pathway and NAD+ metabolism in myalgic encephalomyelitis/chronic fatigue syndrome. Aging Dis 13(3):698–711
Fallarino F et al (2006) Tryptophan catabolism generates autoimmune-preventive regulatory T cells. Transpl Immunol 17(1):58–60
DiNatale BC et al (2010) Kynurenic acid is a potent endogenous aryl hydrocarbon receptor ligand that synergistically induces interleukin-6 in the presence of inflammatory signaling. Toxicol Sci 115(1):89–97
Hayashi T et al (2007) 3-Hydroxyanthranilic acid inhibits PDK1 activation and suppresses experimental asthma by inducing T cell apoptosis. Proc Natl Acad Sci 104(47):18619–18624
Lee W-S et al (2013) The tryptophan metabolite 3-hydroxyanthranilic acid suppresses T cell responses by inhibiting dendritic cell activation. Int Immunopharmacol 17(3):721–726
Linderholm KR et al (2012) Increased levels of kynurenine and kynurenic acid in the CSF of patients with schizophrenia. Schizophr Bull 38(3):426–432
Sellgren CM et al (2019) Peripheral and central levels of kynurenic acid in bipolar disorder subjects and healthy controls. Transl Psychiatry 9(1):37
van den Ameele S et al (2020) A mood state-specific interaction between kynurenine metabolism and inflammation is present in bipolar disorder. Bipolar Disord 22(1):59–69
Messaoud A et al (2018) Reduced peripheral availability of tryptophan and increased activation of the kynurenine pathway and cortisol correlate with major depression and suicide. World J Biol Psychiatr
Cysique LA et al (2023) The kynurenine pathway relates to post-acute COVID-19 objective cognitive impairment and PASC. Ann Clin Transl Neurol 10(8):1338–1352
Kashi AA, Davis RW, Phair RD (2019) The IDO metabolic trap hypothesis for the etiology of ME/CFS. Diagnostics 9(3):82
Groven N et al (2021) Kynurenine metabolites and ratios differ between chronic fatigue syndrome, fibromyalgia, and healthy controls. Psychoneuroendocrinology 105287
Simonato M et al (2021) Tryptophan metabolites, cytokines, and fatty acid binding protein 2 in myalgic encephalomyelitis/chronic fatigue syndrome. Biomedicines 9(11):1724
Qian ZM, Ke Y (2020) Hepcidin and its therapeutic potential in neurodegenerative disorders. Med Res Rev 40(2):633–653
Armitage AE et al (2011) Hepcidin regulation by innate immune and infectious stimuli. Blood, J Am Soc Hematol 118(15):4129–4139
Świątczak M et al (2022) Chronic fatigue syndrome in patients with deteriorated iron metabolism. Diagnostics 12(9):2057
Van Rensburg S et al (2001) Serum concentrations of some metals and steroids in patients with chronic fatigue syndrome with reference to neurological and cognitive abnormalities. Brain Res Bull 55(2):319–325
Bjørklund G et al (2023) Perspectives on iron deficiency as a cause of human disease in global public health. Curr Med Chem. https://doi.org/10.2174/0929867330666230324154606
Nelp MT et al (2018) Immune-modulating enzyme indoleamine 2, 3-dioxygenase is effectively inhibited by targeting its apo-form. Proc Natl Acad Sci 115(13):3249–3254
Wenninger J et al (2019) Associations between tryptophan and iron metabolism observed in individuals with and without iron deficiency. Sci Rep 9(1):1–9
Kubicova L, Chobot V (2021) Potential of kynurenine metabolites in drug development against neurodegenerative diseases. Neural Regen Res 16(2):308
Lidbury BA et al (2017) Activin B is a novel biomarker for chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME) diagnosis: a cross sectional study. J Transl Med 15(1):1–10
Besson-Fournier C et al (2012) Induction of activin B by inflammatory stimuli up-regulates expression of the iron-regulatory peptide hepcidin through Smad1/5/8 signaling. Blood, J Am Soc Hematol 120(2):431–439
Thomas N et al (2022) The underlying sex differences in neuroendocrine adaptations relevant to myalgic encephalomyelitis chronic fatigue syndrome. Front Neuroendocrinol 66:100995
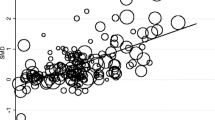
Richardson AM et al (2018) Weighting of orthostatic intolerance time measurements with standing difficulty score stratifies ME/CFS symptom severity and analyte detection. J Transl Med 16(1):1–11
Richardson AM et al (2018) Weighting of orthostatic intolerance time measurements with standing difficulty score stratifies ME/CFS symptom severity and analyte detection. J Transl Med 16:1–11
Lidbury BA et al (2019) Rethinking ME/CFS diagnostic reference intervals via machine learning, and the utility of activin B for defining symptom severity. Diagnostics 9(3):79
Guillemin GJ et al (2007) Characterization of the kynurenine pathway in human neurons. J Neurosci 27(47):12884–12892
Rappsilber J, Mann M, Ishihama Y (2007) Protocol for micro-purification, enrichment, pre-fractionation and storage of peptides for proteomics using StageTips. Nat Protoc 2(8):1896–1906
Ahn SB et al (2019) Potential early clinical stage colorectal cancer diagnosis using a proteomics blood test panel. Clin Proteomics 16:1–20
Ahn SB et al (2021) Use of a recombinant biomarker protein DDA library increases DIA coverage of low abundance plasma proteins. J Proteome Res 20(5):2374–2389
Wu JX et al (2016) SWATH mass spectrometry performance using extended peptide MS/MS assay libraries. Mol Cell Proteomics 15(7):2501–2514
Pascovici D et al (2016) Multiple testing corrections in quantitative proteomics: a useful but blunt tool. Proteomics 16(18):2448–2453
De Bie J et al (2016) Central kynurenine pathway shift with age in women. J Neurochem 136(5):995–1003
Moroni F et al (1984) The excitotoxin quinolinic acid is present in the brain of several mammals and its cortical content increases during the aging process. Neurosci Lett 47(1):51–55
Darlington LG et al (2010) On the biological importance of the 3-hydroxyanthranilic acid: anthranilic acid ratio. Int J Tryptophan Res 3:82
Russell-Jones G (2022) Functional vitamin B12 deficiency in chronic fatigue syndrome. Int J Psychiatry 7(3):153–158
Naviaux RK et al (2016) Metabolic features of chronic fatigue syndrome. Proc Natl Acad Sci 113(37):E5472–E5480
Castro-Marrero J et al (2021) Effect of dietary coenzyme Q10 plus NADH supplementation on fatigue perception and health-related quality of life in individuals with myalgic encephalomyelitis/chronic fatigue syndrome: a prospective, randomized, double-blind, placebo-controlled trial. Nutrients 13(8):2658
Paul ER et al (2022) Peripheral and central kynurenine pathway abnormalities in major depression. Brain Behav Immun 101:136–145
Groven N et al (2021) Kynurenine metabolites and ratios differ between chronic fatigue syndrome, fibromyalgia, and healthy controls. Psychoneuroendocrinology 131:105287
Russell A et al (2019) Persistent fatigue induced by interferon-alpha: a novel, inflammation-based, proxy model of chronic fatigue syndrome. Psychoneuroendocrinology 100:276–285
Montoya JG et al (2017) Cytokine signature associated with disease severity in chronic fatigue syndrome patients. Proc Natl Acad Sci 114(34):E7150–E7158
Tate W et al (2022) Molecular mechanisms of neuroinflammation in ME/CFS and long COVID to sustain disease and promote relapses. Front Neurol 13:936
Cocks BG et al (1993) IL-13 induces proliferation and differentiation of human B cells activated by the CD40 ligand. Int Immunol 5(6):657–663
Fluge Ø et al (2011) Benefit from B-lymphocyte depletion using the anti-CD20 antibody rituximab in chronic fatigue syndrome. A double-blind and placebo-controlled study. PloS one 6(10):e26358
Fluge Ø et al (2019) B-lymphocyte depletion in patients with myalgic encephalomyelitis/chronic fatigue syndrome: a randomized, double-blind, placebo-controlled trial. Ann Intern Med 170(9):585–593
Kell DB, Pretorius E (2022) The potential role of ischaemia–reperfusion injury in chronic, relapsing diseases such as rheumatoid arthritis, Long COVID, and ME/CFS: evidence, mechanisms, and therapeutic implications. Biochem J 479(16):1653–1708
Hoel F et al (2021) A map of metabolic phenotypes in patients with myalgic encephalomyelitis/chronic fatigue syndrome. JCI Insight 6(16):e149217
Sandvik MK et al (2023) Endothelial dysfunction in ME/CFS patients. PLoS ONE 18(2):e0280942
van Campen CM, Rowe PC, Visser FC (2020) Cerebral blood flow is reduced in severe myalgic encephalomyelitis/chronic fatigue syndrome patients during mild orthostatic stress testing: an exploratory study at 20 degrees of head-up tilt testing. in Healthcare. MDPI
Fernández-Ayala DJM, Navas P, López-Lluch G (2020) Age-related mitochondrial dysfunction as a key factor in COVID-19 disease. Exp Gerontol 142:111147
Kobayashi K et al (2001) Detection of Fcγ binding protein antigen in human sera and its relation with autoimmune diseases. Immunol Lett 79(3):229–235
Guan Y et al (2021) Overexpression of PLXDC2 in stromal cell-associated M2 macrophages is related to EMT and the progression of gastric cancer. Front Cell Dev Biol 9:673295
Lovisa S, Genovese G, Danese S (2019) Role of epithelial-to-mesenchymal transition in inflammatory bowel disease. J Crohns Colitis 13(5):659–668
Jones S et al (1995) Adhesion molecules in inflammatory bowel disease. Gut 36(5):724–730
Vainer B (2010) Intercellular adhesion molecule-1 (ICAM-1) in ulcerative colitis: presence, visualization, and significance. APMIS 118:1–46
Bui TM, Wiesolek HL, Sumagin R (2020) ICAM-1: a master regulator of cellular responses in inflammation, injury resolution, and tumorigenesis. J Leucocyte Biol 108(3):787–799
Kim H, Kataru RP, Koh GY (2014) Inflammation-associated lymphangiogenesis: a double-edged sword? J Clin Investig 124(3):936–942
Lee AS et al (2018) COMP-angiopoietin-1 ameliorates inflammation-induced lymphangiogenesis in dextran sulfate sodium (DSS)-induced colitis model. J Mol Med 96:459–467
Zheng J et al (2018) HSPC 159 promotes proliferation and metastasis by inducing epithelial-mesenchymal transition and activating the PI 3K/Akt pathway in breast cancer. Cancer Sci 109(7):2153–2163
Zhao LQ, Thiennu HV (2006) Identification of genes regulating alveolar morphogenesis by supression subtractive hybridization. Fen zi xi bao Sheng wu xue bao = J Mol Cell Biol 39(6):553–562
Rossmann C et al (2014) Expression of serum amyloid A4 in human trophoblast-like choriocarcinoma cell lines and human first trimester/term trophoblast cells. Placenta 35(8):661–664
Seok A et al (2017) Identification and validation of SAA4 as a rheumatoid arthritis prescreening marker by liquid chromatography tandem-mass spectrometry. Molecules 22(5):805
Yamada T et al (2001) Further characterization of serum amyloid A4 as a minor acute phase reactant and a possible nutritional marker. Clin Chem Lab Med 39(1):7–10
Baraniuk JN et al (2005) A chronic fatigue syndrome–related proteome in human cerebrospinal fluid. BMC Neurol 5(1):1–19
Sweetman E et al (2020) A SWATH-MS analysis of myalgic encephalomyelitis/chronic fatigue syndrome peripheral blood mononuclear cell proteomes reveals mitochondrial dysfunction. J Transl Med 18(1):1–18
Milivojevic M et al (2020) Plasma proteomic profiling suggests an association between antigen driven clonal B cell expansion and ME/CFS. PLoS ONE 15(7):e0236148
Giloteaux L et al (2023) Proteomics and cytokine analyses distinguish myalgic encephalomyelitis/chronic fatigue syndrome cases from controls. J Transl Med 21(1):1–22
Chandramouli K, Qian P-Y (2009) Proteomics: challenges, techniques and possibilities to overcome biological sample complexity. Human Genom Proteomics 2009:239204
Guo C et al (2023) Deficient butyrate-producing capacity in the gut microbiome is associated with bacterial network disturbances and fatigue symptoms in ME/CFS. Cell Host Microbe 31(2):288-304.e8
Sheedy JR et al (2009) Increased d-lactic acid intestinal bacteria in patients with chronic fatigue syndrome. In vivo 23(4):621–628
König RS et al (2022) The gut microbiome in myalgic encephalomyelitis (ME)/chronic fatigue syndrome (CFS). Front Immunol 12:628741
Lukić I et al (2019) Role of tryptophan in microbiota-induced depressive-like behavior: evidence from tryptophan depletion study. Front Behav Neurosci 13:123
Williams BB et al (2014) Discovery and characterization of gut microbiota decarboxylases that can produce the neurotransmitter tryptamine. Cell Host Microbe 16(4):495–503
Bhattarai Y et al (2018) Gut microbiota-produced tryptamine activates an epithelial G-protein-coupled receptor to increase colonic secretion. Cell Host Microbe 23(6):775-785.e5
Smith EA, Macfarlane GT (1996) Enumeration of human colonic bacteria producing phenolic and indolic compounds: effects of pH, carbohydrate availability and retention time on dissimilatory aromatic amino acid metabolism. J Appl Bacteriol 81(3):288–302
Roager HM, Licht TR (2018) Microbial tryptophan catabolites in health and disease. Nat Commun 9(1):3294
Gutiérrez-Vázquez C, Quintana FJ (2018) Regulation of the immune response by the aryl hydrocarbon receptor. Immunity 48(1):19–33
Metidji A et al (2018) The environmental sensor AHR protects from inflammatory damage by maintaining intestinal stem cell homeostasis and barrier integrity. Immunity 49(2):353-362.e5
Acknowledgements
Bahar Kavyani is supported by an International PhD scholarship from Macquarie University. Gilles J. Guillemin is supported by the National Health and Medical Research Council (NHMRC; APP1176660) and Macquarie University. Paul R. Fisher and Sarah J. Annesley are supported by the Mason Foundation (MAS2018F00026 and MASONMECFS051). The authors thank Dr Peter Petocz, School of Statistics, Macquarie University for his assistance with statistical analysis.
Funding
This study is supported by the National Health and Medical Research Council (NHMRC, APP1176660), Macquarie University, and the Mason Foundation (MAS2018F00026 and MASONMECFS051).
Author information
Authors and Affiliations
Contributions
Bahar Kavyani, Benjamin Heng, Richard Schloeffel, Gilles J. Guillemin, and Seong Beom Ahn contributed to conception and design of the study. Experiments and data collection were performed by Bahar Kavyani. David B. Lovejoy, Benjamin Heng, Bahar Kavyani, and Seong Beom Ahn contributed to data analysis. Manuscript preparation and editing were performed by Bahar Kavyani, David B. Lovejoy, Benjamin Heng, Paul R. Fisher, Sarah J. Annesley, and Daniel Missailidis. Samples were collected by Paul R. Fisher, Sarah J. Annesley, and Daniel Missailidis. All authors read and approved the manuscript.
Corresponding authors
Ethics declarations
Ethics Approval
Patient recruitment and sample collection were approved by the Australian National University Human Research Ethics Committee (Reference 2015/193 and the La Trobe University Human Ethics Committee (Reference HEC19316).
Consent to Participate
Informed consent was obtained from all participants included in this study.
Consent for Publication
The authors affirm that human research participants provided informed consent for publication of data in Figs. 2, 3, 4, 5, 6 and 7 and Tables 1, 2 and 3.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Gilles J. Guillemin contributed as senior author.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kavyani, B., Ahn, S.B., Missailidis, D. et al. Dysregulation of the Kynurenine Pathway, Cytokine Expression Pattern, and Proteomics Profile Link to Symptomology in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). Mol Neurobiol (2023). https://doi.org/10.1007/s12035-023-03784-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12035-023-03784-z