Abstract
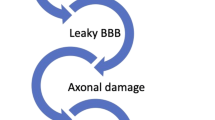
This study aimed to investigate how gut microbiota dysbiosis impacts the repair of the blood-brain barrier and neurological deficits following traumatic brain injury (TBI). Through 16S rRNA sequencing analysis, we compared the gut microbiota of TBI rats and normal controls, discovering significant differences in abundance, species composition, and ecological function, potentially linked to Ghrelin-mediated brain-gut axis functionality. Further, in vivo experiments showed that fecal microbiota transplantation or Ghrelin injection could block the intracerebral TNF signaling pathway, enhance GLP-1 expression, significantly reduce brain edema post-TBI, promote the repair of the blood-brain barrier, and improve neurological deficits. However, the TNF signaling pathway activation could reverse these beneficial effects. In summary, our research suggests that by restoring the balance of gut microbiota, the levels of Ghrelin can be elevated, leading to the blockade of intracerebral TNF signaling pathway and enhanced GLP-1 expression, thereby mitigating post-TBI blood-brain barrier disruption and neurological injuries.










Similar content being viewed by others
Data Availability
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
References
Roozenbeek B, Maas AI, Menon DK (2013) Changing patterns in the epidemiology of traumatic brain injury. Nat Rev Neurol 9(4):231–236. https://doi.org/10.1038/nrneurol.2013.22
Jiang JY, Gao GY, Feng JF et al (2019) Traumatic brain injury in China. Lancet Neurol 18(3):286–295. https://doi.org/10.1016/S1474-4422(18)30469-1
Kowalski RG, Hammond FM, Weintraub AH et al (2021) Recovery of consciousness and functional outcome in moderate and severe traumatic brain injury. JAMA Neurol 78(5):548–557. https://doi.org/10.1001/jamaneurol.2021.0084
Kaur P, Sharma S (2018) Recent advances in pathophysiology of traumatic brain injury. Curr Neuropharmacol 16(8):1224–1238. https://doi.org/10.2174/1570159X15666170613083606
van Vliet EA, Ndode-Ekane XE, Lehto LJ et al (2020) Long-lasting blood-brain barrier dysfunction and neuroinflammation after traumatic brain injury. Neurobiol Dis 145:105080. https://doi.org/10.1016/j.nbd.2020.105080
Kalra S, Malik R, Singh G et al (2022) Pathogenesis and management of traumatic brain injury (TBI): role of neuroinflammation and anti-inflammatory drugs. Inflammopharmacology 30(4):1153–1166. https://doi.org/10.1007/s10787-022-01017-8
Das M, Tang X, Mohapatra SS, Mohapatra S (2019) Vision impairment after traumatic brain injury: present knowledge and future directions. Rev Neurosci 30(3):305–315. https://doi.org/10.1515/revneuro-2018-0015
Uteshev VV, Tenovuo O, Gaidhani N (2016) The cholinergic potential, the vagus nerve and challenges in treatment of traumatic brain injury. Curr Pharm Des 22(14):2083–2092. https://doi.org/10.2174/1381612822666160127111630
Matenchuk BA, Mandhane PJ, Kozyrskyj AL (2020) Sleep, circadian rhythm, and gut microbiota. Sleep Med Rev 53:101340. https://doi.org/10.1016/j.smrv.2020.101340
Hirt N, Body-Malapel M (2020) Immunotoxicity and intestinal effects of nano- and microplastics: a review of the literature. Part Fibre Toxicol 17(1):57. https://doi.org/10.1186/s12989-020-00387-7
Patterson E, Ryan PM, Cryan JF et al (2016) Gut microbiota, obesity and diabetes. Postgrad Med J 92(1087):286–300. https://doi.org/10.1136/postgradmedj-2015-133285
West DB, Diaz J, Roddy S, Woods SC (1987) Long-term effects on adiposity after preweaning nutritional manipulations in the gastrostomy-reared rat. J Nutr 117(7):1259–1264. https://doi.org/10.1093/jn/117.7.1259
Gao K, Mu CL, Farzi A, Zhu WY (2020) Tryptophan metabolism: a link between the gut microbiota and brain. Adv Nutr 11(3):709–723. https://doi.org/10.1093/advances/nmz127
Quigley EMM (2017) Microbiota-brain-gut axis and neurodegenerative diseases. Curr Neurol Neurosci Rep 17(12):94. https://doi.org/10.1007/s11910-017-0802-6
Hu X, Wang T, Jin F (2016) Alzheimer’s disease and gut microbiota. Sci China Life Sci 59(10):1006–1023. https://doi.org/10.1007/s11427-016-5083-9
Megur A, Baltriukiene D, Bukelskiene V, Burokas A (2020) The microbiota-gut-brain axis and Alzheimer’s disease: neuroinflammation is to blame? Nutrients 13(1). https://doi.org/10.3390/nu13010037
Qi L, Cui X, Dong W et al (2014) Ghrelin protects rats against traumatic brain injury and hemorrhagic shock through upregulation of UCP2. Ann Surg 260(1):169–178. https://doi.org/10.1097/SLA.0000000000000328
Qi L, Cui X, Dong W et al (2012) Ghrelin attenuates brain injury after traumatic brain injury and uncontrolled hemorrhagic shock in rats. Mol Med 18(1):186–193. https://doi.org/10.2119/molmed.2011.00390
Shao XF, Li B, Shen J et al (2020) Ghrelin alleviates traumatic brain injury-induced acute lung injury through pyroptosis/NF-kappaB pathway. Int Immunopharmacol 79:106175. https://doi.org/10.1016/j.intimp.2019.106175
Shao X, Hu Q, Chen S, Wang Q, Xu P, Jiang X (2018) Ghrelin ameliorates traumatic brain injury by down-regulating bFGF and FGF-BP. Front Neurosci 12:445. https://doi.org/10.3389/fnins.2018.00445
Bansal V, Ryu SY, Blow C et al (2010) The hormone ghrelin prevents traumatic brain injury induced intestinal dysfunction. J Neurotrauma 27(12):2255–2260. https://doi.org/10.1089/neu.2010.1372
Tian D, Shi W, Yu Y et al (2023) Enrofloxacin exposure induces anxiety-like behavioral responses in zebrafish by affecting the microbiota-gut-brain axis. Sci Total Environ 858(Pt 3):160094. https://doi.org/10.1016/j.scitotenv.2022.160094
Kanehisa M, Sato Y, Kawashima M, Furumichi M, Tanabe M (2016) KEGG as a reference resource for gene and protein annotation. Nucleic Acids Res 44(D1):D457–D462. https://doi.org/10.1093/nar/gkv1070
Douglas GM, Maffei VJ, Zaneveld JR et al (2020) PICRUSt2 for prediction of metagenome functions. Nat Biotechnol 38(6):685–688. https://doi.org/10.1038/s41587-020-0548-6
Yuan F, Xu ZM, Lu LY et al (2016) SIRT2 inhibition exacerbates neuroinflammation and blood-brain barrier disruption in experimental traumatic brain injury by enhancing NF-kappaB p65 acetylation and activation. J Neurochem 136(3):581–593. https://doi.org/10.1111/jnc.13423
You W, Zhu Y, Wei A et al (2022) Traumatic brain injury induces gastrointestinal dysfunction and dysbiosis of gut microbiota accompanied by alterations of bile acid profile. J Neurotrauma 39(1-2):227–237. https://doi.org/10.1089/neu.2020.7526
Mahajan C, Khurana S, Kapoor I et al (2023) Characteristics of gut microbiome after traumatic brain injury. J Neurosurg Anesthesiol 35(1):86–90. https://doi.org/10.1097/ANA.0000000000000789
Du D, Tang W, Zhou C et al (2021) Fecal microbiota transplantation is a promising method to restore gut microbiota dysbiosis and relieve neurological deficits after traumatic brain injury. Oxidative Med Cell Longev 2021:5816837. https://doi.org/10.1155/2021/5816837
Yang DX, Jing Y, Liu YL et al (2019) Inhibition of transient receptor potential vanilloid 1 attenuates blood-brain barrier disruption after traumatic brain injury in mice. J Neurotrauma 36(8):1279–1290. https://doi.org/10.1089/neu.2018.5942
Hashimoto Y, Campbell M (2020) Tight junction modulation at the blood-brain barrier: current and future perspectives. Biochim Biophys Acta Biomembr 1862(9):183298. https://doi.org/10.1016/j.bbamem.2020.183298
Gagnon J, Baggio LL, Drucker DJ, Brubaker PL (2015) Ghrelin is a novel regulator of GLP-1 secretion. Diabetes 64(5):1513–1521. https://doi.org/10.2337/db14-1176
Li W, Zeng Y, Zhao J, Zhu CJ, Hou WG, Zhang S (2014) Upregulation and nuclear translocation of testicular ghrelin protects differentiating spermatogonia from ionizing radiation injury. Cell Death Dis 5(5):e1248. https://doi.org/10.1038/cddis.2014.223
Kowalski K, Mulak A (2019) Brain-gut-microbiota axis in Alzheimer’s disease. J Neurogastroenterol Motil 25(1):48–60. https://doi.org/10.5056/jnm18087
Kesika P, Suganthy N, Sivamaruthi BS, Chaiyasut C (2021) Role of gut-brain axis, gut microbial composition, and probiotic intervention in Alzheimer’s disease. Life Sci 264:118627. https://doi.org/10.1016/j.lfs.2020.118627
Sulhan S, Lyon KA, Shapiro LA, Huang JH (2020) Neuroinflammation and blood-brain barrier disruption following traumatic brain injury: pathophysiology and potential therapeutic targets. J Neurosci Res 98(1):19–28. https://doi.org/10.1002/jnr.24331
Kim KA, Kim D, Kim JH et al (2020) Autophagy-mediated occludin degradation contributes to blood-brain barrier disruption during ischemia in bEnd.3 brain endothelial cells and rat ischemic stroke models. Fluids Barriers CNS 17(1):21. https://doi.org/10.1186/s12987-020-00182-8
Celorrio M, Abellanas MA, Rhodes J et al (2021) Gut microbial dysbiosis after traumatic brain injury modulates the immune response and impairs neurogenesis. Acta Neuropathol Commun 9(1):40. https://doi.org/10.1186/s40478-021-01137-2
Jing Y, Bai F, Wang L et al (2022) Fecal microbiota transplantation exerts neuroprotective effects in a mouse spinal cord injury model by modulating the microenvironment at the lesion site. Microbiol Spectr 10(3):e0017722. https://doi.org/10.1128/spectrum.00177-22
Soriano S, Curry K, Wang Q, Chow E, Treangen TJ, Villapol S (2022) Fecal microbiota transplantation derived from Alzheimer’s disease mice worsens brain trauma outcomes in wild-type controls. Int J Mol Sci 23(9). https://doi.org/10.3390/ijms23094476
Davis BT, Chen Z, Islam M, Timken ME, Procissi D, Schwulst SJ (2022) Fecal microbiota transfer attenuates gut dysbiosis and functional deficits after traumatic brain injury. Shock 57(6):251–259. https://doi.org/10.1097/SHK.0000000000001934
Poher AL, Tschop MH, Muller TD (2018) Ghrelin regulation of glucose metabolism. Peptides 100:236–242. https://doi.org/10.1016/j.peptides.2017.12.015
Lopez NE, Krzyzaniak MJ, Blow C et al (2012) Ghrelin prevents disruption of the blood-brain barrier after traumatic brain injury. J Neurotrauma 29(2):385–393. https://doi.org/10.1089/neu.2011.2053
Leeuwendaal NK, Cryan JF, Schellekens H (2021) Gut peptides and the microbiome: focus on ghrelin. Curr Opin Endocrinol Diabetes Obes 28(2):243–252. https://doi.org/10.1097/MED.0000000000000616
Page LC, Gastaldelli A, Gray SM, D’Alessio DA, Tong J (2018) Interaction of GLP-1 and ghrelin on glucose tolerance in healthy humans. Diabetes 67(10):1976–1985. https://doi.org/10.2337/db18-0451
Glotfelty EJ, Delgado T, Tovar YRLB et al (2019) Incretin mimetics as rational candidates for the treatment of traumatic brain injury. ACS Pharmacol Transl Sci 2(2):66–91. https://doi.org/10.1021/acsptsci.9b00003
Li Y, Glotfelty EJ, Namdar I et al (2020) Neurotrophic and neuroprotective effects of a monomeric GLP-1/GIP/Gcg receptor triagonist in cellular and rodent models of mild traumatic brain injury. Exp Neurol 324:113113. https://doi.org/10.1016/j.expneurol.2019.113113
Casault C, Al Sultan AS, Banoei M, Couillard P, Kramer A, Winston BW (2019) Cytokine responses in severe traumatic brain injury: where there is smoke, is there fire? Neurocrit Care 30(1):22–32. https://doi.org/10.1007/s12028-018-0522-z
Huang Y, Long X, Tang J et al (2020) The attenuation of traumatic brain injury via inhibition of oxidative stress and apoptosis by tanshinone IIA. Oxidative Med Cell Longev 2020:4170156. https://doi.org/10.1155/2020/4170156
Weaver JL (2021) The brain-gut axis: A prime therapeutic target in traumatic brain injury. Brain Res 1753:147225. https://doi.org/10.1016/j.brainres.2020.147225
Hanscom M, Loane DJ, Shea-Donohue T (2021) Brain-gut axis dysfunction in the pathogenesis of traumatic brain injury. J Clin Invest 131(12). https://doi.org/10.1172/JCI143777
Margolis KG, Cryan JF, Mayer EA (2021) The microbiota-gut-brain axis: from motility to mood. Gastroenterol 160(5):1486–1501. https://doi.org/10.1053/j.gastro.2020.10.066
Funding
This study was funded by the Innovation Foundation of The Affiliated Hospital of Chengdu University (No. CDFYCX202209) and the Research Project of Sichuan Medical Association (No. S21055).
Author information
Authors and Affiliations
Contributions
YMZ and JYL planned the experiments; XYL and YZ performed the experiments, prepared the figures, and analyzed the data; YMZ and JYL performed some of the experiments; JG was responsible for the collection of the samples; ZS and LM contributed to drafting the manuscript All authors have read and approved the final submitted manuscript.
Corresponding authors
Ethics declarations
Ethics Approval
The experimental program and animal use protocol has been approved by the Institutional Animal Care and Use Committee (IACUC) of Chengdu University affiliated Hospital (No. PJ2022-126-01).
Consent to Participate
Not applicable
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
Supplemental Fig. 1 The detailed procedures of the in vivo animal experiment. (EPS 2807 kb)
ESM 2
Supplemental Fig. 2 Ecological function prediction of intestinal flora in TBI rats (n = 10) and sham-operated rats (n = 10). A, Functional enrichment of aerobic_chemoheterotrophy in the TBI rats and sham-operated rats. B, Functional enrichment of cellulolysis in the TBI rats and sham-operated rats. C, Functional enrichment of human_pathogens_all in the TBI rats and sham-operated rats. D, Functional enrichment of nitrate-reduction in the TBI rats and sham-operated rats. E, Functional enrichment of xylanolysis in the TBI rats and sham-operated rats. (EPS 1729 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, Y., Liu, J., Liu, X. et al. Fecal Microbiota Transplantation-Mediated Ghrelin Restoration Improves Neurological Functions After Traumatic Brain Injury: Evidence from 16S rRNA Sequencing and In Vivo Studies. Mol Neurobiol 61, 919–934 (2024). https://doi.org/10.1007/s12035-023-03595-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-023-03595-2