Abstract
Gliomas are the most prevalent neurological cancer in the USA and care modalities are not able to effectively combat these aggressive malignancies. Identifying new, more effective treatments require a deep understanding of the complex genetic variations and relevant pathway associations behind these cancers. Drawing connections between gene mutations with a responsive genetic target can help drive therapy selections to enhance patient survival. We have performed extensive molecular profiling of the Capicua gene (CIC), a tumor and transcriptional suppressor gene, and its mutation prevalence in reference to MAPK activation within clinical glioma tissue. CIC mutations occur far more frequently in oligodendroglioma (52.1%) than in low-grade astrocytoma or glioblastoma. CIC-associated mutations were observed across all glioma subtypes, and MAPK-associated mutations were most prevalent in CIC wild-type tissue regardless of the glioma subtype. MAPK activation, however, was enhanced in CIC-mutated oligodendroglioma. The totality of our observations reported supports the use of CIC as a relevant genetic marker for MAPK activation. Identification of CIC mutations, or lack thereof, can assist in selecting, implementing, and developing MEK/MAPK-inhibitory trials to improve patient outcomes potentially.
Similar content being viewed by others
Background
In 2022, neurological cancers were estimated to exceed 25,000 cases and result in over 18,000 deaths in the USA [1]. Around 80% of these deaths were due to malignant gliomas, the most common primary brain cancer in adults [2]. Diffuse adult gliomas are primarily categorized as either astrocytomas or oligodendrogliomas. Lower-grade (WHO 2–3) astrocytomas encompass nearly 10% of gliomas, while Grade 4 astrocytomas, also known as glioblastoma multiforme (GBM), account for 55% of all gliomas. These highly aggressive tumors exhibit one of the lowest survival rates of all cancers, with a 10-year survival of just 2.6% [3, 4]. Five-year survival rates for grades 2 and 3 astrocytomas range between 30 and 50%, respectively [5]. Oligodendrogliomas, defined by the presence of IDH1/2 mutation and co-occurring loss of chromosomes 1p and 19q, make up < 7% of adult diffuse glioma diagnoses. They are relatively slow-growing tumors, with a much better prognosis if discovered at an early age [5,6,7].
The Capicua (CIC) gene is a negative regulator of the mitogen-activated protein kinase (MAPK) signaling pathway [8]. Originally studied in Drosophila, CIC has been recognized as a prospective tumor suppressor gene that mediates cell proliferation and mobility [9]. Located on chromosome 19q, CIC is mutated in nearly 70% of oligodendrogliomas, contributing to poor patient prognosis [10, 11]. CIC knockout, deletion, and mutations have been shown to influence the formation of other cancers, including T-cell lymphoblastic lymphoma, Ewing sarcoma, and metastasis of epidermal growth factor receptor (EGFR) inhibitor-resistant lung adenocarcinoma [8, 12,13,14]. With respect to glioma, studies have shown frequent mutation of CIC in oligodendroglioma but very low mutation frequency in GBM and lower-grade astrocytoma [9]. However, studies performed in Drosophila suggest a relationship between CIC mutations and enhanced MAPK pathway signaling [15]. Nearly 88% of gliomas exhibit MAPK pathway alterations, affecting gene-regulated cell processes, including invasion and proliferation, and playing a role in growth and invasion [16]. Relationships between CIC and its expression levels, MAPK activation, and mutations within both genes can modulate apoptotic activity in malignant cells and enhance survival under hypoxic conditions [17]. Our work seeks to establish a relationship between CIC and MAPK in glioma, as well as generate an understanding of the implications of CIC and MAPK gene expression and mutation levels as they pertain to patient survival and response to current standards of care, possibly introducing CIC as a novel gene target for MAPK-directed therapies.
Methods
Next-generation sequencing (NGS)
NGS was performed on genomic DNA isolated from formalin-fixed paraffin-embedded (FFPE) tumor samples by a commercial CAP/CLIA lab using the NextSeq or NovaSeq 6000 platforms (Illumina, Inc., San Diego, CA). For NextSeq-sequenced tumors, a custom-designed SureSelect XT assay was used to enrich 592 whole-gene targets (Agilent Technologies, Santa Clara, CA). For NovaSeq-sequenced tumors, a panel of more than 700 clinically relevant genes was sequenced at high coverage and high read-depth, along with another panel designed to enrich for additional > 20,000 genes at a lower depth. All variants were detected with > 99% confidence based on allele frequency and amplicon coverage, with an average sequencing depth of coverage of > 500 × and an analytic sensitivity of 5%. Variant testing included single-nucleotide variants (SNV) and insertions and deletions (INDEL) on a panel of 720 genes. Copy number alteration (CNA) analysis was performed on over 400 genes and a 592-gene panel was used for all mutations. Prior to molecular testing, tumor enrichment was achieved by harvesting targeted tissue using manual microdissection techniques. For DNA sequencing, 20% of minimum tumor content was required. Genetic variants identified were interpreted by board-certified molecular geneticists and categorized as ‘pathogenic,’ ‘likely pathogenic,’ ‘variant of unknown significance,’ ‘likely benign,’ or ‘benign,’ according to the American College of Medical Genetics and Genomics (ACMG) standards. When assessing mutation frequencies of individual genes, ‘pathogenic’ and ‘likely pathogenic’ were counted as mutations [18]. The copy number alteration (CNA) of each exon is determined by calculating the average depth of the sample along with the sequencing depth of each exon and comparing this calculated result to a pre-calibrated value.
TMB was measured by counting all non-synonymous missense, nonsense, in-frame insertion/deletion, and frameshift mutations found per tumor that had not been previously described as germline alterations in dbSNP151, Genome Aggregation Database (gnomAD) databases or benign variants identified by Caris geneticists. A cutoff point of ≥ 10 mutations per MB was used based on the KEYNOTE-158 pembrolizumab trial which showed that patients with a TMB of ≥ 10 mt/MB across several tumor types had higher response rates than patients with a TMB of < 10 mt/MB [19].
Whole-transcriptome sequencing
Gene fusion detection was performed on mRNA isolated from a formalin-fixed paraffin-embedded tumor sample using the Illumina NovaSeq platform (Illumina, Inc., San Diego, CA) and Agilent SureSelect Human All Exon V7 bait panel (Agilent Technologies, Santa Clara, CA). FFPE specimens underwent pathology review to diagnose percent tumor content and tumor size; a minimum of 10% of tumor content in the area for microdissection was required to enable enrichment and extraction of tumor-specific RNA. A Qiagen RNA FFPE tissue extraction kit, was used for extraction, and the RNA quality and quantity were determined using the Agilent TapeStation. Biotinylated RNA baits were hybridized to the synthesized and purified cDNA targets and the bait-target complexes were amplified in a post-capture PCR. The resultant libraries were quantified and normalized, and the pooled libraries are denatured, diluted, and sequenced; the reference genome used was GRCh37/hg19 and analytical validation of this test demonstrated ≥ 97% Positive Percent Agreement (PPA), ≥ 99% Negative Percent Agreement (NPA) and ≥ 99% Overall Percent Agreement (OPA) with a validated comparator method. For gene expression, the whole transcriptome from patients was sequenced to an average of 60-M reads. Raw data were demultiplexed by Illumina Dragen BioIT accelerator, trimmed, counted, PCR duplicates removed, and aligned to human reference genome hg19 by STAR aligner. For transcript counting, transcripts per million numbers was generated using the Salmon expression pipeline [20]. Immune cell fraction was calculated by quanTIseq [21].
PyroSeq
MGMT promoter methylation was evaluated by pyrosequencing. DNA extraction from paraffin-embedded tumor samples was performed for subsequent pyrosequencer-based analysis of 5 CpG sites (CpGs 74–78). All DNA samples underwent a bisulfite treatment and were PCR amplified with primers specific for exon 1 of MGMT (GRCh37/hgl9—chr10: 131,265,448- 131,265,560). The methylation status of PCR-amplified products is determined using the PyroMark system (Qiagen, Germantown, MD). Samples with ≥ 7% and < 9% methylation are considered to be equivocal or gray zone results.
Immunohistochemistry
Immunohistochemistry (IHC) of MLH1, M1 antibody; MSH2, G2191129 antibody; MSH6, 44 antibody; and PMS2, EPR3947 antibody were performed on FFPE sections of glass slides. Slides were stained using automated staining techniques, per the manufacturer’s instructions (Ventana Medical Systems, Inc. Tucson, AZ) and were optimized and validated per CLIA/CAP and ISO requirements. Staining was scored for intensity (0 = no staining; 1 + = weak staining; 2 + = moderate staining; 3 + = strong staining) and staining percentage (0–100%). The complete absence of protein expression of any of the 4 proteins tested (0 + in 100% of cells) was considered deficient MMR. A board-certified pathologist evaluated all IHC results independently.
MSI/MMR status
A combination of multiple test platforms was used to determine the MSI or MMR status of the tumors profiled, including fragment analysis (FA, Promega, Madison, WI), IHC (see IHC method), and NGS (7000 target microsatellite loci were examined and compared to the reference genome hg19 from the University of California). The three platforms generated highly concordant results, as previously reported. In the rare cases of discordant results, the MSI or MMR status of the tumor was determined in the order of IHC, FA, and NGS [22].
MPAS
MAPK activation score (MPAS) score was calculated based on the TPM values of RNA expression of 10 genes (SPRY2, SPRY4, ETV4, ETV5, DUSP4, DUSP6, CCND1, PHLDA1, EPHA2, and EPHA4) using a previously reported algorithm as a transcriptomic indicator of MAPK pathway activation [23].
CODEai
Real-world overall survival (rwOS) information was obtained from insurance claims data and calculated from first of treatment time to last of treatment time (TOT). Kaplan–Meier estimates were calculated for molecularly defined patient cohorts. Significance was determined as p values of < 0.05.
Results
CIC demographic and mutation rates in glioma subtypes
A total of 7341 glioma tumor samples were classified based on histology subtypes and characterized for CIC mutation status (Table 1). In total, 296 (4.0%) of gliomas were CIC- mutated, including glioblastoma (0.6%), astrocytoma (1.7%), oligodendroglioma (52.1%), and mixed/unclear typing (10.3%). Of the 19 CIC-mutated astrocytoma samples, 10 were grade 3 and 9 were grade 2. None of the pilocytic/grade 1 astrocytomas were CIC mutated. Of the 202 CIC-mutated oligodendroglioma samples, 93 were grade 3 and 109 were grade 2 (Table 2). In all gliomas analyzed together, CIC mutations were associated with younger age (46 yrs. vs. 58 yrs.) and female gender (50% vs. 41%). These differences were significant, however, only in GBM tumors (median age 49 yrs. vs. 60 yrs., p ≤ 0.00019; female prevalence 58% vs. 40%, p ≤ 0.037; Table 1). Additionally, the association with age was reversed in the oligodendroglioma subset, with CIC-mutated tumors being found in significantly older patients (median age 45.5 yrs. vs. 42 yrs., p ≤ 0.014).
CIC mutations are associated with increased alteration rates of glioma-relevant genes but Not MAPK-associated genes
Whole-Transcriptome Sequencing (WTS), Next-Generation Sequencing (NGS), and immunohistochemistry (IHC) were performed on FFPE tissue samples to identify any molecular alterations associated with CIC mutation status. As shown in Fig. 1A, CIC-mutated tumor samples in all gliomas exhibited significant increases in mutation rates of oncogenic drivers, including FUBP1, NOTCH1, ARID1A, IDH2, MLH1, TET2, KMT2C, and CDKN1B. In addition, increased rates of 1p19q codeletion, TERT promoter mutations, MGMT promoter methylation, and dMMR/MSI were observed in CIC-mutated samples.
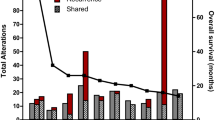
Gene mutation rates are higher in CIC-mutant tissue except for MAPK-related gene in all glioma and all glioma subtypes. A selection of genes and signatures from the array of analysis techniques relevant to tumorigenesis exhibiting mutation relative to CIC mutation or wild-type status (a). Similarly, MAPK-relevant gene mutation status was also characterized (b) and quantified by CIC mutation status; Red = CIC MUT, Blue = CIC WT. MAPK-relevant genes shown via oncoprint by CIC mutation status as CIC mutant (light blue), CIC wild-type (orange), genetic alteration (green), no genetic change (gray), or no data available (white) (c). Mutation rates of MAPK-associated genes in GBM (d), astrocytoma (e), and oligodendroglioma (f) by CIC mutation status; Red = CIC MUT, Blue = CIC WT. *q < 0.05, **q < 0.01, and ***q < 0.001
Conversely, only MAPK pathway-activating alterations were increased in wild-type CIC tumors compared to CIC-mutated tumors. Significant increases of EGFR alterations (including activating mutations, fusions, and the EGFRvIII variant) and NF1 and BRAF mutations were observed in CIC wild-type samples (Fig. 1B). The only significant increase in gene mutation associated with CIC mutation compared to CIC wild-type was MAP2K4 (Fig. 1B). Further genetic alterations associated with CIC mutation status is shown in the OncoPrint in Fig. 1C. Significant genetic alterations, shown in green, were observed in CIC wild-type samples, while few alterations were observed in CIC-mutant samples, confirming the largely mutually exclusive pattern of CIC mutation with other MAPK pathway changes.
Our data across GBM (Fig. 1D), astrocytoma (Fig. 1E), and oligodendroglioma (Fig. 1F) show MAPK-associated gene alterations between CIC-mutated glioma and CIC wild-type tumors. Specifically, CIC wild-type tissue exhibits higher mutation rates of MAPK-associated genes across all glioma subtypes, including more valent EGFR mutation, amplification, EGFRvIII variant, and EGFR fusion. When the relative relationship of MAPK-associated alterations and CIC mutations are examined on OncoPrints (Fig. 2A–C), GBM MAPK-associated gene alterations (Fig. 2A) were shown to be quite prominent in CIC wild-type tumor samples, while CIC-mutated tumors had few alterations in NF1, KRAS, and EGFR. Similarly, astrocytoma (Fig. 2B) and oligodendroglioma (Fig. 2C) exhibited a much higher rate of MAPK-relevant genetic alterations in CIC wild-type tumors where CIC-mutant tumors only displayed few alterations in EGFR, NF1, and KRAS.
MAPK-relevant genetic alterations are more frequently observed in CIC-mutated GBM and astrocytoma with MAPK Activation Score (MPAS) significantly lower for CIC wild-type oligodendroglioma. Oncoplot projections depict MAPK-relevant gene alterations (green), no gene alterations (gray), or no data (white) for GBM (a), astrocytoma (b), and oligodendroglioma (c) by CIC mutation status. Quantification of MAPK activation was calculated via expression profiles of 10 MAPK-associated genes, yielding the MPAS. No significant activation differences were observed between CIC-mutant (red) and CIC wild-type (blue) tissues in all glioma (d), GBM (e), or astrocytoma (f). Oligodendroglioma (g) exhibited lower MPAS in CIC wild-type tissue. ****q < 0.0001
Quantitatively capturing the MAPK pathway association with CIC mutation status via the MAPK Pathway Activity Score (MPAS) scoring method may assist in prognostic evaluations and biomarker associations in various cancer types [23]. Current literature has not yet described MPAS scoring in glioma in association with CIC mutation status. As shown in Fig. 2D–G, significant differences in MAPK activation in CIC-mutant tumors as compared to wild-type only appear in oligodendroglioma, but is not seen in GBM, astrocytoma, or when all three histological subtypes are combined.
GBM, astrocytoma, and oligodendroglioma oncogenic profiles are enhanced in CIC-mutated samples versus CIC wild-type samples
The most prominent glioma subtypes, GBM, astrocytoma, and oligodendroglioma, were individually analyzed to characterize molecular differences between CIC mutants and their CIC wild-type counter parts. As shown in Fig. 3, a majority of oncogenic driver-related genetic alterations were observed in CIC-mutant tumors in GBM (Fig. 3A), astrocytoma (Fig. 3B), and oligodendroglioma (Fig. 3C). Two similarities among the three subtypes were characterized: high prevalence of MGMT promoter methylation, FUBP1 mutation, and IDH1 mutation associated with CIC mutants. Numerous differences, however, were apparent, including increased TMB-high and dMMR/MSI-H prevalence in GBM, and a high rate of TERT promoter mutation and 1p19q codeletion in oligodendroglioma. An increased TP53 mutation rate was observed in CIC wild-type oligodendrogliomas. These results confirm previous reports of significant genetic differences between glioma subtypes and reveal tumor type-specific molecular associations with CIC [24].
Genetic alterations in glioma subtypes are more prevalent in CIC-mutant tissue. Mutation rates of oncologic-related genes and signatures quantified by NGS, Whole-Exome Sequencing (WES) and WTS for GBM (a), astrocytoma (b), and oligodendroglioma (c) by CIC mutation status. *q < 0.05, **q < 0.01, and ***q < 0.001
CIC mutation is positively correlated with patient survival in oligodendroglioma and temozolomide (TMZ)-treated glioma
Patients harboring both CIC mutation and CIC wild-type oligodendroglioma, astrocytoma, and GBM were monitored for over one year following diagnosis to last contact. In oligodendroglioma (Fig. 4A), patients with CIC mutations (90) survived a median 3751 days, while CIC wild-type patients had a median survival of 1911 days. The hazard ratio (HR) between the two groups was 1.758 and a statistically significant difference of median survival of 1840 days yielding p ≤ 0.025. Similarly, as shown in Fig. 4B, patients with either astrocytoma or GBM and CIC wild-type status were grouped into cohort 1 and patients with either astrocytoma or GBM and CIC mutations were grouped into cohort 2. Cohort 1 was followed to a median 536-day survival and cohort 2 did not show a quantifiable end survival date. Because of this, the median difference between the two cohorts was characterized as ‘infinite’ and a p ≤ 0.0001. Additionally, patients who were treated with a TMZ regimen were monitored from first dose of TMZ until last contact. Similar to patients who were not undergoing TMZ treatment, both the oligodendroglioma and combined GBM + astrocytoma cohorts with mutated CIC exhibited longer survival periods (Supp. Figure 1). Specifically, oligodendroglioma patients currently on TMZ therapy with CIC mutation survived a median of 2296 days, while patients with wild-type CIC treated with TMZ survived a median of 907 days (p = 0.002, HR = 2.865) (Supp. Figure 1). In GBM + astrocytoma patients, those with mutated CIC currently on TMZ therapy survived for a median of 1874 days and those patients without CIC mutation survived a median of 602 days (p ≤ 0.001, HR = 2.688) (Supp. Figure 1).
Discussion
Gliomas are difficult to treat and usually result in patient demise within five years of diagnosis [1]. Identification of novel biomarkers to provide clarity on possible patient prognosis and therapeutic response can help create a set of reliable indicators for selecting appropriate therapies [25]. Our study analyzed the prospect of using the CIC gene as an indication of MAPK upregulation within glioma subtypes as well as exploring the underlying genetic landscape that coincides with CIC mutations. This work has shown that the mutation of CIC in glioma was mutually exclusive to MAPK genomic driver alterations, specifically NF1, BRAF, and KRAS. Further, characterization of MAPK activation via MPAS revealed higher activation for mutated CIC in comparison to wild-type CIC. This observation is in line with other studies that discuss the negative correlation between unaltered CIC, MAPK activation, and MAPK driver expression [8, 13, 14, 26].
The current standard of care for all glioma subtypes is tumor resection, if possible [27]. Further decisions on therapeutic modalities are then based on the biomarkers of the tumor and, according to the 5th Edition of the World Health Organization Classification of Tumors of the Central Nervous System (WHO CNS5), particularly the mutational status of isocitrate dehydrogenase (IDH) and the methylation status of methylguanine methyltransferase (MGMT) gene [28]. The National Comprehensive Cancer Network (NCCN) utilizes the status of IDH1 and IDH2, MGMT methylation, codeletion of 1p/19q, and ATRX mutation to drive therapeutic decisions [29]. Low-grade gliomas are commonly treated with radiotherapy and a combination of concurrent or adjuvant TMZ chemotherapy and/or procarbazine and vincristine dependent on the patient-specific molecular markers [28,29,30]. Patients with high-grade glioma, specifically GBM, are usually treated with local radiotherapy and combinatorial TMZ chemotherapy [28, 31]. Unfortunately, most patients receiving these therapies either do not respond or experience recurrence, commonly resulting in death. Numerous clinical trials have been introduced attempting to improve the treatment of glioma, including growth factor receptor inhibition, both EGFR and fibroblast (FGFR); apoptotic pathway regulation; angiogenic targets; and several immunotherapeutic approaches [32,33,34,35,36,37,38,39]. Though some trials have had success in improving overall survival [32,33,34,35, 39], limitations arise in matching targeted therapies to the molecular profile of glioma subtypes.
Here, we describe the prospect of the CIC gene as a target to evaluating tumorigenesis and predicting MAPK-associated therapeutic selections. Previous literature has reported CIC expression and mutation patterns in gliomas with nearly 40% of oligodendroglioma tumors harboring CIC alterations [10, 40]. Further, these alterations in oligodendroglioma along with loss of FUBP1 expression have been shown to be potential markers of rapid recurrence [10]. We have confirmed these observations by showing 50.2% mutation rate in oligodendroglioma, 51.4% mutation rate in anaplastic, high-grade oligodendroglioma, and 49.0% mutation rate in diffuse, low-grade oligodendroglioma. Glioblastoma and astrocytoma both exhibited very low mutation rates at 0.6% and 1.9%, respectively. Though mutation rates vary significantly across histological subtypes, each subtype exhibited fewer MAPK-associated gene mutations in concordance with CIC mutation. Additionally, mutation of CIC resulted in increased alterations of genes and cell signals related to tumorigenesis and MAPK activation. Because of this, mutated CIC can possibly be a predictor of MAPK mutation rate, pathway activation, and heightened tumorigenesis. Characterizing this relationship with MAPK through MPAS, mutant CIC, specifically, drove higher trending MAPK activation scores in GBM and astrocytoma, with significant increases shown in oligodendroglioma. Interestingly, the survival analyses via CODEai algorithm reported enhanced survival in patients with CIC mutations over patients with CIC wild-type. Across oligodendroglioma, astrocytoma, and GBM, patients with identified CIC mutations survived longer, on average, than patients without mutations. This was the case for all CODEai analyses, including those patients treated with TMZ (Supp. Figure 1) and those treated with TMZ harboring IDH mutations and MGMT methylation (Supp. Figure 2).
Utilizing inhibitory agents to block oncogenic molecular cascades from occurring have shown the most promise in glioma therapies. Four MEK/MAPK inhibitors have been approved for use in solid tumors: trametinib, binimetinib, selumetinib, and cobimetinib [41,42,43]. Each have been evaluated in clinical cohorts and have yielded results supporting use in both pediatric and adult populations with MAPK aberrations, adding to the repertoire of available therapies outside of TMZ [43,44,45,46]. These results exemplify the ability of these therapeutics to penetrate the blood brain barrier effectively and should be further studied to evaluate response variation in patients with MAPK-related genetic variation.
Though the findings mentioned do lend insight into the difficulties that are seen with treatment of glioma, it was describing the relationship between CIC and MAPK that elucidate on treatment efficacy and survivability concerns that drive the significance home. While a significant amount of attention is being given toward immunotherapies in many other solid tumors, the ‘cold’ TME of glioma, with no correlative relationship to CIC status (Supp. Figure 1), renders many immunotherapies ineffective. We have shown that mutated CIC, a MAPK-relevant marker, causes an increased rate of oncogenic mutations, possibly driving tumorigenesis. In addition, mutated CIC created increased MAPK activation significantly in oligodendroglioma. Because the largest percentage of glioma subtype CIC mutations are found in oligodendroglioma, this observation may help in selecting MAPK inhibitors as a therapeutic option for these patients in addition to the ability of MAPK inhibitors to cross the blood–brain barrier, overcoming a major challenge that significantly reduces the efficacy of most therapeutics [47]. Even though few significant shifts in the immune landscape were shown with CIC mutations, this work contributes to the understanding of genetic mutations that can harbor significant consequences of tumor progression. Future work on the CIC–MAPK relationship should include in vivo studies to examine the efficacy of MAPK inhibition on glioma tumors harboring CIC mutation, preferably using the four MAPK inhibitors currently approved for clinical use.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request. The deidentified sequencing data are owned by Caris Life Sciences. Qualified researchers can apply for access to these summarized data by contacting Joanne Xiu, PhD and signing a data usage agreement.
References
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7–33.
Ostrom QT, Cioffi G, Waite K, Kruchko C, Barnholtz-Sloan JS. CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2014–2018. Neuro Oncol. 2021;23(12 Suppl 2):iii1–105.
Kim HJ, Park JW, Lee JH. Genetic architectures and cell-of-origin in glioblastoma. Front Oncol. 2020;10:615400.
Tykocki T, Eltayeb M. Ten-year survival in glioblastoma. A systematic review, J Clin Neurosci. 2018;54:7–13.
Goodenberger ML, Jenkins RB. Genetics of adult glioma. Cancer Genet. 2012;205(12):613–21.
van den Bent MJ, Smits M, Kros JM, Chang SM. Diffuse infiltrating oligodendroglioma and astrocytoma. J Clin Oncol. 2017;35(21):2394–401.
Jin K, Zhang SY, Li LW, Zou YF, Wu B, Xia L, Sun CX. Prognosis of oligodendroglioma patients stratified by age: a SEER population-based analysis. Int J Gen Med. 2021;14:9523–36.
Weissmann S, Cloos PA, Sidoli S, Jensen ON, Pollard S, Helin K. The tumor suppressor CIC directly regulates MAPK pathway genes via histone deacetylation. Cancer Res. 2018;78(15):4114–25.
Bunda S, Heir P, Metcalf J, Li ASC, Agnihotri S, Pusch S, Yasin M, Li M, Burrell K, Mansouri S, Singh O, Wilson M, Alamsahebpour A, Nejad R, Choi B, Kim D, von Deimling A, Zadeh G, Aldape K. CIC protein instability contributes to tumorigenesis in glioblastoma. Nat Commun. 2019;10(1):661.
Chan AK, Pang JC, Chung NY, Li KK, Poon WS, Chan DT, Shi Z, Chen L, Zhou L, Ng HK. Loss of CIC and FUBP1 expressions are potential markers of shorter time to recurrence in oligodendroglial tumors. Mod Pathol. 2014;27(3):332–42.
Bettegowda C. Mutations in CIC and FUBP1 contribute to human oligodendroglioma. Science. 2011;333:1453–5.
Kawamura-Saito M, Yamazaki Y, Kaneko K, Kawaguchi N, Kanda H, Mukai H, Gotoh T, Motoi T, Fukayama M, Aburatani H, Takizawa T, Nakamura T. Fusion between CIC and DUX4 up-regulates PEA3 family genes in Ewing-like sarcomas with t(4;19)(q35;q13) translocation. Hum Mol Genet. 2006;15(13):2125–37.
Okimoto RA, Breitenbuecher F, Olivas VR, Wu W, Gini B, Hofree M, Asthana S, Hrustanovic G, Flanagan J, Tulpule A, Blakely CM, Haringsma HJ, Simmons AD, Gowen K, Suh J, Miller VA, Ali S, Schuler M, Bivona TG. Inactivation of Capicua drives cancer metastasis. Nat Genet. 2017;49(1):87–96.
Simon-Carrasco L, Grana O, Salmon M, Jacob HKC, Gutierrez A, Jimenez G, Drosten M, Barbacid M. Inactivation of Capicua in adult mice causes T-cell lymphoblastic lymphoma. Genes Dev. 2017;31(14):1456–68.
Jimenez G, Guichet A, Ephrussi A, Casanova J. Relief of gene repression by Torso RTK signaling - role of capicua in Drosophila terminal and dorsoventral patterning. Genes Dev. 2000;14:224–31.
Pandey V, Bhaskara VK, Babu PP. Implications of mitogen-activated protein kinase signaling in glioma. J Neurosci Res. 2016;94(2):114–27.
Braicu C, Buse M, Busuioc C, Drula R, Gulei D, Raduly L, Rusu A, Irimie A, Atanasov AG, Slaby O, Ionescu C, Berindan-Neagoe I. A comprehensive review on MAPK: a promising therapeutic target in cancer. Cancers (Basel). 2019;11(10):1618.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, Grody WW, Hegde M, Lyon E, Spector E, Voelkerding K, Rehm HL, Committee ALQA. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American college of medical genetics and genomics and the association for molecular pathology. Genet Med. 2015;17(5):405–24.
Marabelle A, Fakih M, Lopez J, Shah M, Shapira-Frommer R, Nakagawa K, Chung HC, Kindler HL, Lopez-Martin JA, Miller WH, Italiano A, Kao S, Piha-Paul SA, Delord J-P, McWilliams RR, Fabrizio DA, Aurora-Garg D, Xu L, Jin F, Norwood K, Bang Y-J. Association of tumour mutational burden with outcomes in patients with advanced solid tumours treated with pembrolizumab: prospective biomarker analysis of the multicohort, open-label, phase 2 KEYNOTE-158 study. Lancet Oncol. 2020;21(10):1353–65.
Patro R, Duggal G, Love MI, Irizarry RA, Kingsford C. Salmon provides fast and bias-aware quantification of transcript expression. Nat Methods. 2017;14(4):417–9.
Finotello F, Mayer C, Plattner C, Laschober G, Rieder D, Hackl H, Krogsdam A, Loncova Z, Posch W, Wilflingseder D, Sopper S, Ijsselsteijn M, Brouwer TP, Johnson D, Xu Y, Wang Y, Sanders ME, Estrada MV, Ericsson-Gonzalez P, Charoentong P, Balko J, de Miranda N, Trajanoski Z. Molecular and pharmacological modulators of the tumor immune contexture revealed by deconvolution of RNA-seq data. Genome Med. 2019;11(1):34.
Vanderwalde A, Spetzler D, Xiao N, Gatalica Z, Marshall J. Microsatellite instability status determined by next-generation sequencing and compared with PD-L1 and tumor mutational burden in 11,348 patients. Cancer Med. 2018;7(3):746–56.
Wagle MC, Kirouac D, Klijn C, Liu B, Mahajan S, Junttila M, Moffat J, Merchant M, Huw L, Wongchenko M, Okrah K, Srinivasan S, Mounir Z, Sumiyoshi T, Haverty PM, Yauch RL, Yan Y, Kabbarah O, Hampton G, Amler L, Ramanujan S, Lackner MR, Huang SA. A transcriptional MAPK Pathway Activity Score (MPAS) is a clinically relevant biomarker in multiple cancer types. NPJ Precis Oncol. 2018;2(1):7.
Ohgaki H, Kleihues P. Genetic profile of astrocytic and oligodendroglial gliomas. Brain Tumor Pathol. 2011;28(3):177–83.
Chen TY, Liu Y, Chen L, Luo J, Zhang C, Shen XF. Identification of the potential biomarkers in patients with glioma: a weighted gene co-expression network analysis. Carcinogenesis. 2020;41(6):743–50.
Simon-Carrasco L, Jimenez G, Barbacid M, Drosten M. The Capicua tumor suppressor: a gatekeeper of Ras signaling in development and cancer. Cell Cycle. 2018;17(6):702–11.
Jakola AS, Skjulsvik AJ, Myrmel KS, Sjavik K, Unsgard G, Torp SH, Aaberg K, Berg T, Dai HY, Johnsen K, Kloster R, Solheim O. Surgical resection versus watchful waiting in low-grade gliomas. Ann Oncol. 2017;28(8):1942–8.
Yang K, Wu Z, Zhang H, Zhang N, Wu W, Wang Z, Dai Z, Zhang X, Zhang L, Peng Y, Ye W, Zeng W, Liu Z, Cheng Q. Glioma targeted therapy: insight into future of molecular approaches. Mol Cancer. 2022;21(1):39.
Kim YZ, Kim CY, Lim DH. The overview of practical guidelines for gliomas by KSNO, NCCN, and EANO. Brain Tumor Res Treat. 2022;10(2):83–93.
Behin A, Hoang-Xuan K, Carpentier AF, Delattre J-Y. Primary brain tumours in adults. The Lancet. 2003;361(9354):323–31.
Weller M, van den Bent M, Tonn JC, Stupp R, Preusser M, Cohen-Jonathan-Moyal E, Henriksson R, Rhun EL, Balana C, Chinot O, Bendszus M, Reijneveld JC, Dhermain F, French P, Marosi C, Watts C, Oberg I, Pilkington G, Baumert BG, Taphoorn MJB, Hegi M, Westphal M, Reifenberger G, Soffietti R, Wick W. European association for neuro-oncology (EANO) guideline on the diagnosis and treatment of adult astrocytic and oligodendroglial gliomas. Lancet Oncol. 2017;18(6):e315–29.
Friedman HS, Prados MD, Wen PY, Mikkelsen T, Schiff D, Abrey LE, Yung WK, Paleologos N, Nicholas MK, Jensen R, Vredenburgh J, Huang J, Zheng M, Cloughesy T. Bevacizumab alone and in combination with irinotecan in recurrent glioblastoma. J Clin Oncol. 2009;27(28):4733–40.
Bouffet E, Larouche V, Campbell BB, Merico D, de Borja R, Aronson M, Durno C, Krueger J, Cabric V, Ramaswamy V, Zhukova N, Mason G, Farah R, Afzal S, Yalon M, Rechavi G, Magimairajan V, Walsh MF, Constantini S, Dvir R, Elhasid R, Reddy A, Osborn M, Sullivan M, Hansford J, Dodgshun A, Klauber-Demore N, Peterson L, Patel S, Lindhorst S, Atkinson J, Cohen Z, Laframboise R, Dirks P, Taylor M, Malkin D, Albrecht S, Dudley RW, Jabado N, Hawkins CE, Shlien A, Tabori U. Immune checkpoint inhibition for hypermutant glioblastoma multiforme resulting from germline biallelic mismatch repair deficiency. J Clin Oncol. 2016;34(19):2206–11.
Bahleda R, Italiano A, Hierro C, Mita A, Cervantes A, Chan N, Awad M, Calvo E, Moreno V, Govindan R, Spira A, Gonzalez M, Zhong B, Santiago-Walker A, Poggesi I, Parekh T, Xie H, Infante J, Tabernero J. Multicenter Phase I Study of Erdafitinib (JNJ-42756493), oral pan-fibroblast growth factor receptor inhibitor, in patients with advanced or refractory solid tumors. Clin Cancer Res. 2019;25(16):4888–97.
Schalper KA, Rodriguez-Ruiz ME, Diez-Valle R, Lopez-Janeiro A, Porciuncula A, Idoate MA, Inoges S, de Andrea C, Lopez-Diaz de Cerio A, Tejada S, Berraondo P, Villarroel-Espindola F, Choi J, Gurpide A, Giraldez M, Goicoechea I, Gallego Perez-Larraya J, Sanmamed MF, Perez-Gracia JL, Melero I. Neoadjuvant nivolumab modifies the tumor immune microenvironment in resectable glioblastoma. Nat Med. 2019;25(3):470–6.
Lee EQ, Zhang P, Wen PY, Gerstner ER, Reardon DA, Aldape KD, deGroot JF, Pan E, Raizer JJ, Kim LJ, Chmura SJ, Robins HI, Connelly JM, Battiste JD, Villano JL, Wagle N, Merrell RT, Wendland MM, Mehta MP. NRG/RTOG 1122: a phase 2, double-blinded, placebo-controlled study of bevacizumab with and without trebananib in patients with recurrent glioblastoma or gliosarcoma. Cancer. 2020;126(12):2821–8.
Gluck WL, Gounder MM, Frank R, Eskens F, Blay JY, Cassier PA, Soria JC, Chawla S, de Weger V, Wagner AJ, Siegel D, De Vos F, Rasmussen E, Henary HA. Phase 1 study of the MDM2 inhibitor AMG 232 in patients with advanced P53 wild-type solid tumors or multiple myeloma. Invest New Drugs. 2020;38(3):831–43.
Sepulveda-Sanchez JM, Vaz MA, Balana C, Gil-Gil M, Reynes G, Gallego O, Martinez-Garcia M, Vicente E, Quindos M, Luque R, Ramos A, Ruano Y, Perez-Segura P, Benavides M, Sanchez-Gomez P, Hernandez-Lain A. Phase II trial of dacomitinib, a pan-human EGFR tyrosine kinase inhibitor, in recurrent glioblastoma patients with EGFR amplification. Neuro Oncol. 2017;19(11):1522–31.
Chen C, Cheng CD, Wu H, Wang ZW, Wang L, Jiang ZR, Wang AL, Hu C, Dong YF, Niu WX, Qi S, Qi ZP, Liu J, Wang WC, Niu CS, Liu QS. Osimertinib successfully combats EGFR-negative glioblastoma cells by inhibiting the MAPK pathway. Acta Pharmacol Sin. 2021;42(1):108–14.
Yip S, Butterfield YS, Morozova O, Chittaranjan S, Blough MD, An J, Birol I, Chesnelong C, Chiu R, Chuah E, Corbett R, Docking R, Firme M, Hirst M, Jackman S, Karsan A, Li H, Louis DN, Maslova A, Moore R, Moradian A, Mungall KL, Perizzolo M, Qian J, Roldan G, Smith EE, Tamura-Wells J, Thiessen N, Varhol R, Weiss S, Wu W, Young S, Zhao Y, Mungall AJ, Jones SJ, Morin GB, Chan JA, Cairncross JG, Marra MA. Concurrent CIC mutations, IDH mutations, and 1p/19q loss distinguish oligodendrogliomas from other cancers. J Pathol. 2012;226(1):7–16.
Selvasaravanan KD, Wiederspohn N, Hadzalic A, Strobel H, Payer C, Schuster A, Karpel-Massler G, Siegelin MD, Halatsch ME, Debatin KM, Westhoff MA. The limitations of targeting MEK signalling in glioblastoma therapy. Sci Rep. 2020;10(1):7401.
Han J, Liu Y, Yang S, Wu X, Li H, Wang Q. MEK inhibitors for the treatment of non-small cell lung cancer. J Hematol Oncol. 2021;14(1):1.
Fangusaro J, Onar-Thomas A, Young Poussaint T, Wu S, Ligon AH, Lindeman N, Banerjee A, Packer RJ, Kilburn LB, Goldman S, Pollack IF, Qaddoumi I, Jakacki RI, Fisher PG, Dhall G, Baxter P, Kreissman SG, Stewart CF, Jones DTW, Pfister SM, Vezina G, Stern JS, Panigrahy A, Patay Z, Tamrazi B, Jones JY, Haque SS, Enterline DS, Cha S, Fisher MJ, Doyle LA, Smith M, Dunkel IJ, Fouladi M. Selumetinib in paediatric patients with BRAF-aberrant or neurofibromatosis type 1-associated recurrent, refractory, or progressive low-grade glioma: a multicentre, phase 2 trial. Lancet Oncol. 2019;20(7):1011–22.
Trippett T, Toledano H, Campbell Hewson Q, Verschuur A, Langevin AM, Aerts I, Howell L, Gallego S, Rossig C, Smith A, Patel D, Pereira LR, Cheeti S, Musib L, Hutchinson KE, Devlin C, Bernardi R, Geoerger B. Cobimetinib in pediatric and young adult patients with relapsed or refractory solid tumors (iMATRIX-cobi): a multicenter. Phase I/II Study, Target Oncol. 2022;17(3):283–93.
Bikhezar F, de Kruijff RM, van der Meer A, Torrelo Villa G, van der Pol SMA, Becerril Aragon G, Gasol Garcia A, Narayan RS, de Vries HE, Slotman BJ, Denkova AG, Sminia P. Preclinical evaluation of binimetinib (MEK162) delivered via polymeric nanocarriers in combination with radiation and temozolomide in glioma. J Neurooncol. 2020;146(2):239–46.
Selt F, van Tilburg CM, Bison B, Sievers P, Harting I, Ecker J, Pajtler KW, Sahm F, Bahr A, Simon M, Jones DTW, Well L, Mautner VF, Capper D, Hernaiz Driever P, Gnekow A, Pfister SM, Witt O, Milde T. Response to trametinib treatment in progressive pediatric low-grade glioma patients. J Neurooncol. 2020;149(3):499–510.
Tan Q, Zhao S, Xu T, Wang Q, Lan M, Yan L, Chen X. Getting drugs to the brain: advances and prospects of organic nanoparticle delivery systems for assisting drugs to cross the blood-brain barrier. J Mater Chem B. 2022;10(45):9314–33.
Acknowledgements
The authors would like to thank and recognize the contributions and statistical support provided by Dr. Dan Magee, PhD, Caris Life Sciences.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
Conceptualization and Study Design: SD, JX, and MJD; Case Contribution: SD, SK, SA, KMW, SS, AS, and MJD; Writing and Original Draft Preparation: TS; Writing, reviewing, and editing of the manuscript: TS, SD, JX, SK, SA, KMW, SS, AS, JC, DS, MG, and MJD; Data Analysis: JX; Data Review and Discussion: JC, DS, and MG.
Corresponding author
Ethics declarations
Competing interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethical approval
This study was conducted in accordance with the guidelines of the Declaration of Helsinki, Belmont report, and U.S. Common rule. In keeping with 45 CFR 46.101(b)(4), this study was performed utilizing retrospective, deidentified clinical data. Therefore, this study is considered IRB-exempt, and no patient consent was necessary from the subject.
Consent to participate
This study was conducted in accordance with the guidelines of the Declaration of Helsinki, Belmont report, and U.S. Common rule. In keeping with 45 CFR 46.101(b)(4), this study was performed utilizing retrospective, deidentified clinical data. Therefore, this study is considered IRB-exempt, and no patient consent was necessary from the subject.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Darabi, S., Xiu, J., Samec, T. et al. Capicua (CIC) mutations in gliomas in association with MAPK activation for exposing a potential therapeutic target. Med Oncol 40, 197 (2023). https://doi.org/10.1007/s12032-023-02071-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-023-02071-0