Abstract
Goals
To determine the attitudes and practices of gastroenterologists regarding the delivery of cancer diagnoses.
Background
Gastroenterologists frequently diagnose colorectal cancer. Receiving the news of a cancer diagnosis is difficult, and the delivery of the diagnosis can influence a patient’s understanding of their disease. No study to date has reported how gastroenterologists deliver cancer diagnoses to their patients.
Study
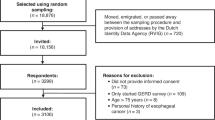
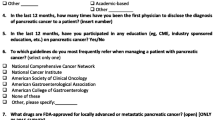
An anonymous questionnaire was sent online to gastroenterologists of the American College of Gastroenterology to assess views regarding the delivery of cancer diagnoses.
Results
Of the 280 complete responses (response rate = 1.64%), most respondents were male (n = 205, 73.21%), in practice between 0 and 9 years (n = 133, 47.50%), and at the attending/faculty level (n = 69.53%, 194). Most responded that they would disclose a cancer diagnosis to the patient themselves if they had made the discovery on endoscopy/colonoscopy (n = 255, 94.80%), with the preferred methods being an in person discussion (n = 187, 71.65%). Most respondents were not familiar with any guidelines for delivering cancer diagnoses (n = 202, 75.94%) and would be open to receiving training on cancer diagnosis delivery (n = 207, 78.11%).
Conclusions
Most gastroenterologists take personal responsibility in the delivery of cancer diagnoses. Many gastroenterologists receive no specific training on how to deliver this news and are unaware of any guidelines to follow that may be helpful in their practice. However, most displayed a willingness to learn these guidelines through some form of formal education. Future directions should consider the incorporation of education in cancer diagnosis delivery for gastroenterologists and gastroenterology fellows.

Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author upon request.
References
Arnold M, Abnet CC, Neale RE, et al. Global burden of 5 major types of gastrointestinal cancer. Gastroenterology. 2020;159(1):335–349 e15. https://doi.org/10.1053/j.gastro.2020.02.068.
Key Statistics for Colorectal Cancer. Accessed 30 Oct 2021. https://www.cancer.org/cancer/colon-rectal-cancer/about/key-statistics.html.
von Blanckenburg P, Hofmann M, Rief W, Seifart U, Seifart C. Assessing patients preferences for breaking bad news according to the SPIKES-Protocol: the MABBAN scale. Patient Educ Couns. 2020;103(8):1623–9. https://doi.org/10.1016/j.pec.2020.02.036.
Oken D. What to tell cancer patients. A study of medical attitudes JAMA. 1961;175:1120–8. https://doi.org/10.1001/jama.1961.03040130004002.
Friedman HJ. Physician management of dying patients: an exploration. Psychiatry Med. 1970;1(4):295–305. https://doi.org/10.2190/qhye-h6gw-ym2j-tpc6.
Adler DD, Riba MB, Eggly S. Breaking bad news in the breast imaging setting. Acad Radiol. 2009;16(2):130–5. https://doi.org/10.1016/j.acra.2008.08.006.
Baile WF, Lenzi R, Parker PA, Buckman R, Cohen L. Oncologists’ attitudes toward and practices in giving bad news: an exploratory study. J Clin Oncol. 2002;20(8):2189–96. https://doi.org/10.1200/JCO.2002.08.004.
Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP. SPIKES-A six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5(4):302–11. https://doi.org/10.1634/theoncologist.5-4-302.
Keum N, Giovannucci E. Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nat Rev Gastroenterol Hepatol. 2019;16(12):713–32. https://doi.org/10.1038/s41575-019-0189-8.
Gebhardt C, Gorba C, Oechsle K, Vehling S, Koch U, Mehnert A. [Breaking bad news to cancer patients: content, communication preferences and psychological distress]. Psychother Psychosom Med Psychol. 2017;67(7):312–321. Die Kommunikation schlechter Nachrichten bei Krebspatienten: Inhalte, Kommunikationspraferenzen und psychische Belastungen. https://doi.org/10.1055/s-0043-113628.
Alves CGB, Treister NS, Ribeiro ACP, et al. Strategies for communicating oral and oropharyngeal cancer diagnosis: why talk about it? Oral Surg Oral Med Oral Pathol Oral Radiol. 2020;129(4):347–56. https://doi.org/10.1016/j.oooo.2019.11.014.
Porensky EK, Carpenter BD. Breaking bad news: effects of forecasting diagnosis and framing prognosis. Patient Educ Couns. 2016;99(1):68–76. https://doi.org/10.1016/j.pec.2015.07.022.
Street RL Jr, Makoul G, Arora NK, Epstein RM. How does communication heal? Pathways linking clinician-patient communication to health outcomes. Patient Educ Couns. 2009;74(3):295–301. https://doi.org/10.1016/j.pec.2008.11.015.
Langbecker D, Caffery LJ, Gillespie N, Smith AC. Using survey methods in telehealth research: a practical guide. J Telemed Telecare. 2017;23(9):770–9. https://doi.org/10.1177/1357633X17721814.
Kelley K, Clark B, Brown V, Sitzia J. Good practice in the conduct and reporting of survey research. Int J Qual Health Care. 2003;15(3):261–6. https://doi.org/10.1093/intqhc/mzg031.
Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of Internet e-surveys (CHERRIES). J Med Internet Res. 2004;6(3):e34. https://doi.org/10.2196/jmir.6.3.e34.
Al-Mohaimeed AA, Sharaf FK. Breaking bad news issues: a survey among physicians. Oman Med J. 2013;28(1):20–5. https://doi.org/10.5001/omj.2013.05.
Fulmer T, Escobedo M, Berman A, Koren MJ, Hernandez S, Hult A. Physicians’ views on advance care planning and end-of-life care conversations. J Am Geriatr Soc. 2018;66(6):1201–5. https://doi.org/10.1111/jgs.15374.
Kumar M, Goyal S, Singh K, et al. Breaking bad news issues: a survey among radiation oncologists. Indian J Palliat Care. 2009;15(1):61–6. https://doi.org/10.4103/0973-1075.53533.
Eid A, Petty M, Hutchins L, Thompson R. “Breaking bad news”: standardized patient intervention improves communication skills for hematology-oncology fellows and advanced practice nurses. J Cancer Educ. 2009;24(2):154–9. https://doi.org/10.1080/08858190902854848.
Musa A, Baron DA, Anavim A, et al. Notions of Preprocedural Patient Anxiety in the Realm of IR. J Vasc Interv Radiol. 2020;31(2):336–340 e1. https://doi.org/10.1016/j.jvir.2019.04.007.
Funding
Guarantor: Dr. Tobias Zuchelli.
Author information
Authors and Affiliations
Contributions
Abdelwahab Ahmed: this author served as corresponding author, completed data analysis, and contributed to the creation of the manuscript. Arif Musa: this author performed data analysis and contributed to the creation of the final manuscript. Shannon Lohman: this author contributed to the creation of the final manuscript. Ji-Cheng Hsieh: this author contributed to the creation of the final manuscript. Keving Harris: this author contributed to the creation of the final manuscript. Salman Faisal: this author contributed to the creation of the final manuscript. Mouhanna Ghanimeh: this author contributed to the creation of the final manuscript. Eva Alsheik: this author contributed to the creation of the final manuscript. Tobias Zuchelli: this author contributed to the creation of the final manuscript and serves as the principal investigator.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ahmed, A., Musa, A., Lohman, S. et al. Attitudes of Gastroenterologists Regarding Delivery of Cancer Diagnoses: a Cross-Sectional Study. J Gastrointest Canc 54, 1286–1291 (2023). https://doi.org/10.1007/s12029-023-00921-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-023-00921-8