Abstract
Purpose
The impact of body mass index (BMI) on outcomes after open or laparoscopic surgery for rectal cancer remains unclear. The objective of this retrospective cohort study was to examine the interaction of body mass index and surgical modality (i.e., laparoscopy versus open) with respect to short-term clinical outcomes in patients with rectal cancer.
Methods
The ACS-NSQIP database (2012–2016) was reviewed for patients undergoing open or laparoscopic surgery for rectal cancer. The primary outcome was 30-day all-cause morbidity. Logistic regression and Cox proportional hazard models were used for analysis.
Results
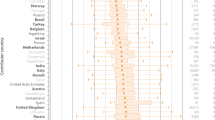
A total of 16,145 patients were grouped into open (N = 6759, 42%) and laparoscopic (N = 9386, 58%) cohorts. Patients with higher BMI (p < 0.001) and those undergoing open surgery (p < 0.001) were at increased risk of all-cause morbidity. There was no significant change in the odds ratio of experiencing all-cause morbidity between open and laparoscopic surgery with increasing BMI (p = 0.572). Median length of stay was significantly shorter in the laparoscopy group (4 days vs. 6 days; p < 0.001), at the cost of increased operative time (239 min vs. 210 min, p < 0.001). The difference in operative time between laparoscopy and open surgery did not increase with rising BMI (i.e., ∆37 min vs. ∆39 min at BMI 25 kg/m2 vs 50 kg/m2, respectively, p = 0.491).
Conclusion
BMI may not be a strong modifier for surgical approach with respect to short-term clinical outcomes in patients with obesity and rectal cancer. Laparoscopic surgery was associated with improved short-term clinical outcomes, without much change in the absolute difference in operative time compared with open surgery, even at higher BMIs.




Similar content being viewed by others
Availability of Data and Material
All raw data is available in the form of participant use files from the ACS-NSQIP website (https://www.facs.org/quality-programs/acs-nsqip/participant-use).
References
Haggar FA, Boushey RP. Colorectal cancer epidemiology: incidence, mortality, survival, and risk factors. Clin Colon Rectal Surg. 2009;22(4):191–7.
Fleshman JW, Smallwood N. Current concepts in rectal cancer. Clin Colon Rectal Surg. 2015;28(1):5–11.
González-Muniesa P, Mártinez-González MA, Hu FB, et al. Obesity Nat Rev Dis Primers. 2017;3:17034.
Qiu Y, Liu Q, Chen G, et al. Outcome of rectal cancer surgery in obese and nonobese patients: a meta-analysis. World J Surg Oncol. 2016;14(1):23.
Kang SB, Park JW, Jeong SY, et al. Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol. 2010;11(7):637–45.
Jeong SY, Park JW, Nam BH, et al. Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol. 2014;15(7):767–74.
Bonjer HJ, Deijen CL, Haglind E, et al. A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med. 2015;373(2):194.
Chen K, Cao G, Chen B, et al. Laparoscopic versus open surgery for rectal cancer: A meta-analysis of classic randomized controlled trials and high-quality Nonrandomized Studies in the last 5 years. Int J Surg. 2017;39:1–10.
Huang Y, Lee Y, Huang Y, et al. Comparison of clinical outcomes between laparoscopic and open surgery for left-sided colon cancer: a nationwide population-based study. Scientific Reports. 2020;10(75):1–7.
Conticchio M, Papagni V, Notarnicola M, et al. Laparoscopic vs. open mesorectal excision for rectal cancer: Are these approaches still comparable? A systematic review and meta-analysis. PLoS One. 2020;15(7): e0235887.
von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4(10):e296.
Schwenk W, Haase O, Neudecker J, et al. Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev. 2005(3):CD003145.
Hida K, Okamura R, Sakai Y, et al. Open versus laparoscopic surgery for advanced low rectal cancer: a large, multicenter, propensity score matched cohort study in Japan. Ann Surg. 2018;268(2):318–24.
Veldkamp R, Kuhry E, Hop WC, et al. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005;6:477–84.
Hussan H, Gray DM, Hinton A, et al. Morbid obesity is associated with increased mortality, surgical complications, and incremental health care utilization in the peri-operative period of colorectal cancer surgery. World J Surg. 2016;40(4):987–94.
Bell S, Kong JC, Wale R, et al. The effect of increasing body mass index on laparoscopic surgery for colon and rectal cancer. Colorectal Dis. 2018;20(9):778–88.
Stevenson AR, Solomon MJ, Lumley JW, et al. Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA. 2015;314(13):1356–63.
Ishikawa K, Kusumi T, Hosokawa M, et al. Incisional surgical site infection after elective open surgery for colorectal cancer. Int J Surg Oncol. 2014;2014:419712.
Lee L, Wong-Chong N, Kelly JJ, et al. Minimally invasive surgery for stage III colon adenocarcinoma is associated with less delay to initiation of adjuvant systemic therapy and improved survival. Surg Endosc. 2018.
Manchon-Walsh P, Aliste L, Biondo S, et al. A propensity-score-matched analysis of laparoscopic vs open surgery for rectal cancer in a population-based study. Colorectal Dis. 2018.
Sood SK, Kang P, Ihedioha U, et al. Response to Bell et al., The effect of increasing body mass index on laparoscopic surgery for colon and rectal cancer. Colorectal Dis. 2018.
Davis CH, Gaglani T, Moore LW, et al. Trends and outcomes in laparoscopic versus open surgery for rectal cancer from 2005 to 2016 using the ACS-NSQIP database, a retrospective cohort study. Int J Surg. 2019;63:71–6.
Sheils CR, Dahlke AR, Kreutzer L, et al. Evaluation of hospitals participating in the American College of Surgeons National Surgical Quality Improvement Program. Surgery. 2016;160(5):1182–8.
Goulart A, Malheiro N, Rios H, et al. Influence of visceral fat in the outcomes of colorectal cancer. Dig Surg. 2018.
Scott SI, Farid S, Mann C, et al. Abdominal fat ratio—a novel parameter for predicting conversion in laparoscopic colorectal surgery. Ann R Coll Surg Engl. 2017;99(1):46–50.
Author information
Authors and Affiliations
Contributions
Conceptualization: all authors. Methodology: Dhruvin Hirpara, Colin O’Rourke, and Sami Chadi. Formal analysis and investigation: Dhruvin Hirpara and Colin O’Rourke. Writing—original draft preparation: Dhruvin Hirpara, Colin O’Rourke, and Arash Azin. Writing—review and editing: all authors. Funding acquisition: not applicable. Resources: Sami Chadi. Supervision: Steven Wexner and Sami Chadi.
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Wexner—consulting: Intuitive Surgical, Karl Storz, Stryker, Medtronic, Takeda, Regentys, and OstomyCure; stock options: Regentys, LifeBond, Pragma, and Renew Medical; royalties: Medtronic, Intuitive Surgical, Karl Storz, and Unique Surgical Innovations.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hirpara, D.H., O’Rourke, C., Azin, A. et al. Impact of BMI on Adverse Events After Laparoscopic and Open Surgery for Rectal Cancer. J Gastrointest Canc 53, 370–379 (2022). https://doi.org/10.1007/s12029-021-00612-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-021-00612-2