Abstract
Background
Children supported with extracorporeal membrane oxygenation (ECMO) have been shown to be at risk for developing seizures. However, previous studies have consisted of heterogeneous patient populations. We aimed to describe the rate of seizures in pediatric patients receiving ECMO for cardiac indications and to identify risk factors for the occurrence of this complication.
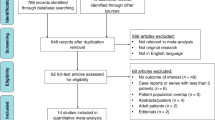
Methods
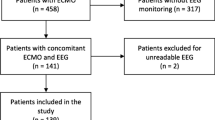
This is a retrospective cohort study of consecutive pediatric patients on ECMO for congenital or acquired cardiac disease between 2014 and 2018 at a tertiary care pediatric hospital.
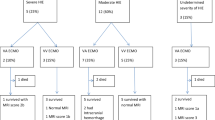
Results
We reviewed 110 children, of whom 104 (95%) received continuous electroencephalogram for at least 48 h after ECMO initiation. Seizures were observed in 20 (18%) children. Seizures were subclinical only in 13 (65%) patients, and 8 (40%) developed status epilepticus. The median time from ECMO initiation to first seizure was 34 h (25%, 75%: 19, 44). Children with seizures were more likely to have suffered pre-ECMO cardiac arrest (odds ratio 5.7, 95% confidence interval 2.0–16.1, p < 0.001), require extracorporeal cardiopulmonary resuscitation (odds ratio 5.2, 95% confidence interval 1.9–14.7, p < 0.001), and have been cannulated via the cervical vessels (p = 0.029). Children with seizures also had lower pH nadir prior to ECMO (p = 0.015) and had higher peak lactate prior to ECMO (p = 0.002). Patients with seizures had significantly a longer median intensive care unit length of stay, (43 versus 32 days, p = 0.02), had a significantly worse pediatric cerebral performance score (2 versus 1, p = 0.03), and tended to have worse survival to hospital discharge (50% versus 71%, p = 0.069).
Conclusions
Seizures in pediatric patients on ECMO for cardiac indications are common, occurring in nearly one in five patients. Seizures are frequently subclinical only and often progress to status epilepticus. Continuous electroencephalogram is therefore warranted for this patient population, especially in the setting of cardiac arrest, extracorporeal cardiopulmonary resuscitation, or severe metabolic acidosis.

Similar content being viewed by others
References
Thiagarajan RR, Barbaro RP, Rycus PT, et al. Extracorporeal life support organization registry international report 2016. ASAIO J. 2017;63:60–7.
Thiagarajan RR, Laussen PC, Rycus PT, Bartlett RH, Bratton SL. Extracorporeal membrane oxygenation to aid cardiopulmonary resuscitation in infants and children. Circulation. 2007;116:1693–700.
Walters HL 3rd, Hakimi M, Rice MD, Lyons JM, Whittlesey GC, Klein MD. Pediatric cardiac surgical ECMO: multivariate analysis of risk factors for hospital death. Ann Thorac Surg. 1995;60:329–36; discussion 36–7.
Raithel SC, Pennington DG, Boegner E, Fiore A, Weber TR. Extracorporeal membrane oxygenation in children after cardiac surgery. Circulation. 1992;86:II305–10.
Ghez O, Feier H, Ughetto F, Fraisse A, Kreitmann B, Metras D. Postoperative extracorporeal life support in pediatric cardiac surgery: recent results. ASAIO J. 2005;51:513–6.
Barrett CS, Bratton SL, Salvin JW, Laussen PC, Rycus PT, Thiagarajan RR. Neurological injury after extracorporeal membrane oxygenation use to aid pediatric cardiopulmonary resuscitation. Pediatr Crit Care Med. 2009;10:445–51.
Mehta A, Ibsen LM. Neurologic complications and neurodevelopmental outcome with extracorporeal life support. World J Crit Care Med. 2013;2:40–7.
Hervey-Jumper SL, Annich GM, Yancon AR, Garton HJ, Muraszko KM, Maher CO. Neurological complications of extracorporeal membrane oxygenation in children. J Neurosurg Pediatr. 2011;7:338–44.
Polito A, Barrett CS, Wypij D, et al. Neurologic complications in neonates supported with extracorporeal membrane oxygenation. An analysis of ELSO registry data. Intensive Care Med. 2013;39:1594–601.
Booth KL, Roth SJ, Thiagarajan RR, Almodovar MC, del Nido PJ, Laussen PC. Extracorporeal membrane oxygenation support of the Fontan and bidirectional Glenn circulations. Ann Thorac Surg. 2004;77:1341–8.
Yuliati A, Federman M, Rao LM, Chen L, Sim MS, Matsumoto JH. Prevalence of seizures and risk factors for mortality in a continuous cohort of pediatric extracorporeal membrane oxygenation patients. Pediatr Crit Care Med. 2020;21:949–58.
Okochi S, Shakoor A, Barton S, et al. Prevalence of seizures in pediatric extracorporeal membrane oxygenation patients as measured by continuous electroencephalography. Pediatr Crit Care Med. 2018;19:1162–7.
Lin JJ, Banwell BL, Berg RA, et al. Electrographic seizures in children and neonates undergoing extracorporeal membrane oxygenation. Pediatr Crit Care Med. 2017;18:249–57.
Barbaro RP, Paden ML, Guner YS, et al. Pediatric extracorporeal life support organization registry international report 2016. ASAIO J. 2017;63:456–63.
Piantino JA, Wainwright MS, Grimason M, et al. Nonconvulsive seizures are common in children treated with extracorporeal cardiac life support. Pediatr Crit Care Med. 2013;14:601–9.
Cook RJ, Rau SM, Lester-Pelham SG, et al. Electrographic seizures and brain injury in children requiring extracorporeal membrane oxygenation. Pediatr Neurol. 2020;108:77–85.
Sansevere AJ, DiBacco ML, Akhondi-Asl A, et al. EEG features of brain injury during extracorporeal membrane oxygenation in children. Neurology. 2020;95:e1372–80.
Pollack MM, Holubkov R, Glass P, et al. Functional Status Scale: new pediatric outcome measure. Pediatrics. 2009;124:e18-28.
Fiser DH. Assessing the outcome of pediatric intensive care. J Pediatr. 1992;121:68–74.
Tsuchida TN, Wusthoff CJ, Shellhaas RA, et al. American clinical neurophysiology society standardized EEG terminology and categorization for the description of continuous EEG monitoring in neonates: report of the American Clinical Neurophysiology Society critical care monitoring committee. J Clin Neurophysiol. 2013;30:161–73.
Hirsch LJ, LaRoche SM, Gaspard N, et al. American clinical neurophysiology society’s standardized critical care EEG terminology: 2012 version. J Clin Neurophysiol. 2013;30:1–27.
Abend NS, Arndt DH, Carpenter JL, et al. Electrographic seizures in pediatric ICU patients: cohort study of risk factors and mortality. Neurology. 2013;81:383–91.
Topjian AA, Gutierrez-Colina AM, Sanchez SM, et al. Electrographic status epilepticus is associated with mortality and worse short-term outcome in critically ill children. Crit Care Med. 2013;41:215–23.
Wagenman KL, Blake TP, Sanchez SM, et al. Electrographic status epilepticus and long-term outcome in critically ill children. Neurology. 2014;82:396–404.
Legriel S, Hilly-Ginoux J, Resche-Rigon M, et al. Prognostic value of electrographic postanoxic status epilepticus in comatose cardiac-arrest survivors in the therapeutic hypothermia era. Resuscitatio. 2013;84:343–50.
Naim MY, Gaynor JW, Chen J, et al. Subclinical seizures identified by postoperative electroencephalographic monitoring are common after neonatal cardiac surgery. J Thorac Cardiovasc Surg. 2015;150:169–78; discussion 78–80.
Funding
This study received no funding.
Author information
Authors and Affiliations
Contributions
DH and MF were involved in the study design and conception, data collection, data analysis, data interpretation, and drafting of the manuscript. SW and CM were involved in study design and conception, data interpretation, and revising of the manuscript. MS was involved in study design and conception, data analysis, and revising of the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval/informed consent
This retrospective study was approved by the institutional review board at Indiana University, and the need for informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hassumani, D.O., Shan, M., Mastropietro, C.W. et al. Seizures in Children with Cardiac Disease on Extracorporeal Membrane Oxygenation. Neurocrit Care 36, 157–163 (2022). https://doi.org/10.1007/s12028-021-01276-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-021-01276-3