Abstract
Background
Progressive hemorrhagic injury (PHI) is common in patients with severe traumatic brain injury (TBI) and is associated with poor outcomes. TBI-associated coagulopathy is frequent and has been described as risk factor for PHI. This coagulopathy is a dynamic process involving hypercoagulable and hypocoagulable states either one after the other either concomitant. Fibrin monomers (FMs) are a direct marker of thrombin action and thus reflect coagulation activation. This study sought to determine the ability of FM to predict PHI after severe TBI.
Methods
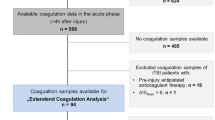
We conducted a prospective, observational study including all severe TBI patients admitted in the trauma center. Between September 2011 and September 2016, we enrolled patients with severe TBI into the derivation cohort. Between October 2016 and December 2018, we recruited the validation cohort on the same basis. Study protocol included FM measurements and standard coagulation test at admission and two computed tomography (CT) scans (upon arrival and at least 6 h thereafter). A PHI was defined by an increment in size of initial lesion (25% or more) or the development of a new hemorrhage in the follow-up CT scan. Multivariate logistic regression analysis was applied to identify predictors of PHI.
Results
Overall, 106 patients were included in the derivation cohort. Fifty-four (50.9%) experienced PHI. FM values were higher in these patients (151 [136.8–151] vs. 120.5 [53.3–151], p < 0.0001). The ROC curve demonstrated that FM had a fair accuracy to predict the occurrence of PHI with an area under curve of 0.7 (95% CI [0.6–0.79]). The best threshold was determined at 131.7 μg/ml. In the validation cohort of 54 patients, this threshold had a negative predictive value of 94% (95% CI [71–100]) and a positive predictive value of 49% (95% CI [32–66]). The multivariate logistic regression analysis identified 2 parameters associated with PHI: FM ≥ 131.7 (OR 6.8; 95% CI [2.8–18.1]) and Marshall category (OR 1.7; 95% CI [1.3–2.2]). Coagulopathy was not associated with PHI (OR 1.3; 95% CI [0.5–3.0]). The proportion of patients with an unfavorable functional neurologic outcome at 6-months follow-up was higher in patients with positive FM: 59 (62.1%) versus 16 (29.1%), p < 0.0001.
Conclusions
FM levels at admission had a fair accuracy to predict PHI in patients with severe TBI. FM values ≥ 131.7 μg/ml are independently associated with the occurrence of PHI.







Similar content being viewed by others
Abbreviations
- TBI:
-
Traumatic brain injury
- GCS:
-
Glasgow Coma Scale
- ICU:
-
Intensive care unit
- ICP:
-
Intracranial pressure
- GOS:
-
Glasgow Outcome Scale
- AUC:
-
Area under curve
- ROC:
-
Receiver operating characteristic
- 95% CI:
-
95% confidence intervals
- PHI:
-
Progressive hemorrhagic injury
- INR:
-
Internationalized normalized ratio
- FM:
-
Fibrin monomer
- FDP:
-
Fibrin/fibrinogen-degradation products
- TIC:
-
Trauma-induced coagulopathy
- PT:
-
Prothrombin time
- aPTT:
-
Activated partial thromboplastin time
- Se:
-
Sensitivity
- Spe:
-
Specificity
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
- LR+:
-
Positive likelihood ratio
- ISS:
-
Injury Severity Score
- ADP:
-
Agonists adenosine diphosphate
- AA:
-
Arachidonic acid
- TF:
-
Tissue factor
- MVs:
-
Microvesicles
References
Maas AIR, Stocchetti N, Bullock R. Moderate and severe traumatic brain injury in adults. Lancet Neurol. 2008;7(8):728–41.
Alali AS, Burton K, Fowler RA, Naimark DMJ, Scales DC, Mainprize TG, et al. Economic evaluations in the diagnosis and management of traumatic brain injury: a systematic review and analysis of quality. Value Health. 2015;18(5):721–34.
Emami P, Czorlich P, Fritzsche FS, Westphal M, Rueger JM, Lefering R, et al. Impact of Glasgow Coma Scale score and pupil parameters on mortality rate and outcome in pediatric and adult severe traumatic brain injury: a retrospective, multicenter cohort study. J Neurosurg. 2017;126(3):760–7.
Esnault P, Nguyen C, Bordes J, D’Aranda E, Montcriol A, Contargyris C, et al. Early-onset ventilator-associated pneumonia in patients with severe traumatic brain injury: incidence, risk factors, and consequences in cerebral oxygenation and outcome. Neurocrit Care. 2017;27(2):187–98.
Cepeda S, Gómez PA, Castaño-Leon AM, Martínez-Pérez R, Munarriz PM, Lagares A. Traumatic intracerebral hemorrhage: risk factors associated with progression. J Neurotrauma. 2015;32(16):1246–53.
Juratli TA, Zang B, Litz RJ, Sitoci K-H, Aschenbrenner U, Gottschlich B, et al. Early hemorrhagic progression of traumatic brain contusions: frequency, correlation with coagulation disorders, and patient outcome: a prospective study. J Neurotrauma. 2014;31(17):1521–7.
Tian H-L, Chen H, Wu B-S, Cao H-L, Xu T, Hu J, et al. D-dimer as a predictor of progressive hemorrhagic injury in patients with traumatic brain injury: analysis of 194 cases. Neurosurg Rev. 2010;33(3):359–65 (discussion 365–6).
Oertel M, Kelly DF, McArthur D, Boscardin WJ, Glenn TC, Lee JH, et al. Progressive hemorrhage after head trauma: predictors and consequences of the evolving injury. J Neurosurg. 2002;96(1):109–16.
Yuan Q, Sun Y-R, Wu X, Yu J, Li Z-Q, Du Z-Y, et al. Coagulopathy in traumatic brain injury and its correlation with progressive hemorrhagic injury: a systematic review and meta-analysis. J Neurotrauma. 2016;33(14):1279–91.
Stolla M, Zhang F, Meyer MR, Zhang J, Dong J-F. Current state of transfusion in traumatic brain injury and associated coagulopathy. Transfusion. 2019;59(S2):1522–8.
Wada H, Sakuragawa N. Are fibrin-related markers useful for the diagnosis of thrombosis? Semin Thromb Hemost. 2008;34(1):33–8.
Hasegawa M, Wada H, Miyazaki S, Yamaguchi T, Wakabayashi H, Fujimoto N, et al. The evaluation of fibrin-related markers for diagnosing or predicting acute or subclinical venous thromboembolism in patients undergoing major orthopedic surgery. Clin Appl Thromb Hemost. 2018;24(1):107–14.
Singh N, Pati HP, Tyagi S, Upadhyay AD, Saxena R. Evaluation of the diagnostic performance of fibrin monomer in comparison to D-dimer in patients with overt and nonovert disseminated intravascular coagulation. Clin Appl Thromb Hemost. 2017;23(5):460–5.
Hatada T, Wada H, Kawasugi K, Okamoto K, Uchiyama T, Kushimoto S, et al. Analysis of the cutoff values in fibrin-related markers for the diagnosis of overt DIC. Clin Appl Thromb Hemost. 2012;18(5):495–500.
Gris J-C, Cochery-Nouvellon E, Bouvier S, Jaber S, Albanese J, Constantin J-M, et al. Clinical value of automated fibrin generation markers in patients with septic shock: a SepsiCoag ancillary study. Br J Haematol. 2018;11(101):1644.
Sørensen JV, Jensen HP, Rahr HB, Borris LC, Lassen MR, Fedders O, et al. Fibrinogen and fibrin derivatives in traumatized patients: relation to injury severity and posttraumatic pulmonary dysfunction. Haemostasis. 1993;23(2):91–7.
Folkerson LE, Sloan D, Cotton BA, Holcomb JB, Tomasek JS, Wade CE. Predicting progressive hemorrhagic injury from isolated traumatic brain injury and coagulation. Surgery. 2015;158(3):655–61.
Yuan F, Ding J, Chen H, Guo Y, Wang G, Gao W-W, et al. Predicting progressive hemorrhagic injury after traumatic brain injury: derivation and validation of a risk score based on admission characteristics. J Neurotrauma. 2012;29(12):2137–42.
Brain Trauma Foundation, American Association of Neurological Surgeons, Congress of Neurological Surgeons. Guidelines for the management of severe traumatic brain injury. J Neurotrauma. 2007;24(Suppl 1):S1–106.
Wafaisade A, Lefering R, Tjardes T, Wutzler S, Simanski C, Paffrath T, et al. Acute coagulopathy in isolated blunt traumatic brain injury. Neurocrit Care. 2010;12(2):211–9.
Zehtabchi S, Soghoian S, Liu Y, Carmody K, Shah L, Whittaker B, et al. The association of coagulopathy and traumatic brain injury in patients with isolated head injury. Resuscitation. 2008;76(1):52–6.
Hamano A, Tanaka S, Takeda Y, Umeda M, Sakata Y. A novel monoclonal antibody to fibrin monomer and soluble fibrin for the detection of soluble fibrin in plasma. Clin Chim Acta. 2002;318(1–2):25–32.
Maegele M, Schöchl H, Menovsky T, Maréchal H, Marklund N, Buki A, et al. Coagulopathy and haemorrhagic progression in traumatic brain injury: advances in mechanisms, diagnosis, and management. Lancet Neurol. 2017;16(8):630–47.
de Oliveira Manoel AL, Neto AC, Veigas PV, Rizoli S. Traumatic brain injury associated coagulopathy. Neurocrit Care. 2015;22(1):34–44.
Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1(7905):480–4.
Wan X, Fan T, Wang S, Zhang S, Liu S, Yang H, et al. Progressive hemorrhagic injury in patients with traumatic intracerebral hemorrhage: characteristics, risk factors and impact on management. Acta Neurochir (Wien). 2017;159(2):227–35.
Palazón-Bru A, Folgado-de la Rosa DM, Cortés-Castell E, López-Cascales MT, Gil-Guillén VF. Sample size calculation to externally validate scoring systems based on logistic regression models. PLoS ONE. 2017;12(5):e0176726.
Zhang J, He M, Song Y, Xu J. Prognostic role of D-dimer level upon admission in patients with traumatic brain injury. Medicine (Baltimore). 2018;97(31):e11774.
Gando S, Hayakawa M. Pathophysiology of trauma-induced coagulopathy and management of critical bleeding requiring massive transfusion. Semin Thromb Hemost. 2016;42(2):155–65.
Zhang J, Jiang R, Liu L, Watkins T, Zhang F, Dong J-F. Traumatic brain injury-associated coagulopathy. J Neurotrauma. 2012;29(17):2597–605.
Harhangi BS, Kompanje EJO, Leebeek FWG, Maas AIR. Coagulation disorders after traumatic brain injury. Acta Neurochir (Wien). 2008;150(2):165–75.
Engström M, Romner B, Schalén W, Reinstrup P. Thrombocytopenia predicts progressive hemorrhage after head trauma. J Neurotrauma. 2005;22(2):291–6.
Allard CB, Scarpelini S, Rhind SG, Baker AJ, Shek PN, Tien H, et al. Abnormal coagulation tests are associated with progression of traumatic intracranial hemorrhage. J Trauma. 2009;67(5):959–67.
Hulka F, Mullins RJ, Frank EH. Blunt brain injury activates the coagulation process. Arch Surg. 1996;131(9):923–7 (discussion 927–8).
Kearney TJ, Bentt L, Grode M, Lee S, Hiatt JR, Shabot MM. Coagulopathy and catecholamines in severe head injury. J Trauma. 1992;32(5):608–11 (discussion 611–2).
Piek J, Chesnut RM, Marshall LF, van Berkum-Clark M, Klauber MR, Blunt BA, et al. Extracranial complications of severe head injury. J Neurosurg. 1992;77(6):901–7.
Laroche M, Kutcher ME, Huang MC, Cohen MJ, Manley GT. Coagulopathy after traumatic brain injury. Neurosurgery. 2012;70(6):1334–45.
Nakae R, Takayama Y, Kuwamoto K, Naoe Y, Sato H, Yokota H. Time course of coagulation and fibrinolytic parameters in patients with traumatic brain injury. J Neurotrauma. 2016;33(7):688–95.
McCully SP, Schreiber MA. Traumatic brain injury and its effect on coagulopathy. Semin Thromb Hemost. 2013;39(8):896–901.
Davis PK, Musunuru H, Walsh M, Cassady R, Yount R, Losiniecki A, et al. Platelet dysfunction is an early marker for traumatic brain injury-induced coagulopathy. Neurocrit Care. 2013;18(2):201–8.
Castellino FJ, Chapman MP, Donahue DL, Thomas S, Moore EE, Wohlauer MV, et al. Traumatic brain injury causes platelet adenosine diphosphate and arachidonic acid receptor inhibition independent of hemorrhagic shock in humans and rats. J Trauma Acute Care Surg. 2014;76(5):1169–76.
Foley JH, Conway EM. Cross talk pathways between coagulation and inflammation. Circ Res. 2016;118(9):1392–408.
Atefi G, Aisiku O, Shapiro N, Hauser C, Dalle Lucca J, Flaumenhaft R, et al. Complement activation in trauma patients alters platelet function. Shock. 2016;46(3 Suppl 1):83–8.
Cohen MJ, Brohi K, Ganter MT, Manley GT, Mackersie RC, Pittet J-F. Early coagulopathy after traumatic brain injury: the role of hypoperfusion and the protein C pathway. J Trauma. 2007;63(6):1254–61 (discussion 1261–2).
Hijazi N, Abu Fanne R, Abramovitch R, Yarovoi S, Higazi M, Abdeen S, et al. Endogenous plasminogen activators mediate progressive intracerebral hemorrhage after traumatic brain injury in mice. Blood. 2015;125(16):2558–67.
Eddleston M, la Torre de JC, Oldstone MB, Loskutoff DJ, Edgington TS, Mackman N. Astrocytes are the primary source of tissue factor in the murine central nervous system. A role for astrocytes in cerebral hemostasis. J Clin Invest. 1993;92(1):349–58.
Nekludov M, Mobarrez F, Gryth D, Bellander B-M, Wallen H. Formation of microparticles in the injured brain of patients with severe isolated traumatic brain injury. J Neurotrauma. 2014;31(23):1927–33.
Tian Y, Salsbery B, Wang M, Yuan H, Yang J, Zhao Z, et al. Brain-derived microparticles induce systemic coagulation in a murine model of traumatic brain injury. Blood. 2015;125(13):2151–9.
Mause SF, Weber C. Microparticles: protagonists of a novel communication network for intercellular information exchange. Circ Res. 2010;107(9):1047–57.
Morel O, Morel N, Jesel L, Freyssinet J-M, Toti F. Microparticles: a critical component in the nexus between inflammation, immunity, and thrombosis. Semin Immunopathol. 2011;33(5):469–86.
Mooberry MJ, Key NS. Microparticle analysis in disorders of hemostasis and thrombosis. Cytometry A. 2016;89(2):111–22.
Zhang D, Gong S, Jin H, Wang J, Sheng P, Zou W, et al. Coagulation parameters and risk of progressive hemorrhagic injury after traumatic brain injury: a systematic review and meta-analysis. Biomed Res Int. 2015;2015(6):261825-10.
Goodnight SH, Kenoyer G, Rapaport SI, Patch MJ, Lee JA, Kurze T. Defibrination after brain-tissue destruction: a serious complication of head injury. N Engl J Med. 1974;290(19):1043–7.
Mann KG, Butenas S, Brummel K. The dynamics of thrombin formation. Arterioscler Thromb Vasc Biol. 2003;23(1):17–25.
Refaai MA, Riley P, Mardovina T, Bell PD. The Clinical Significance of Fibrin Monomers. Thromb Haemost. 2018;118(11):1856–66.
Rao A, Lin A, Hilliard C, Fu R, Lennox T, Barbosa R, et al. The utility of thromboelastography for predicting the risk of progression of intracranial hemorrhage in traumatic brain injury patients. Neurosurgery. 2017;64(CN_suppl_1):182–7.
Author information
Authors and Affiliations
Contributions
PE, QM, and EM contributed to the study concept and design. PE, QM, ED, AM, PJC, and MC contributed to the acquisition of data. PE, CD, AD, and PG contributed to the analysis and interpretation of data. PE, PG, and EM contributed to drafting the manuscript and critically revising the manuscript for important intellectual content. All authors read and approved the final manuscript.
Source of Support
None.
Conflicts of Interest
The authors have no conflicts of interest related to this study.
Ethical Approval/Informed Consent
This study was approved by the Institutional Review Board of the Sainte Anne Military Hospital, Toulon (France). The institutional review board waived the requirement for informed consent from patients or their kin, given the observational nature of the study.
Availability of Supporting Data
Not applicable.
Consent for Publication
Not applicable.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Esnault, P., Mathais, Q., D’Aranda, E. et al. Ability of Fibrin Monomers to Predict Progressive Hemorrhagic Injury in Patients with Severe Traumatic Brain Injury. Neurocrit Care 33, 182–195 (2020). https://doi.org/10.1007/s12028-019-00882-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-019-00882-6