Abstract
Background
Refractory intracranial hypertension (RICH) is associated with high mortality in severe traumatic brain injury (sTBI). Indomethacin (INDO) can decrease intracranial cerebral pressure (ICP) improving cerebral pressure perfusion (CPP). Our aim was to determine modifications in ICP and CPP following INDO in RICH secondary to sTBI.
Methods
INDO was administered in a loading dose (0.8 mg/kg/15 min), followed by continuous 2-h infusion period (0.5 mg/kg/h). Clinical outcome was assessed at 30 days according to Glasgow Outcome Scale (GOS). Differences in ICP and CPP values were assessed using repeated-measures ANOVA. Receiver operating characteristic curve (AUC) was used for discrimination in predicting 30-day survival and good functional outcome (GOS 4 or 5). Analysis of INDO safety profile was also conducted.
Results
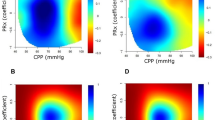
Thirty-two patients were included. Median GCS score was 6 (interquartile range: 4–7). The most frequent CT finding was the evacuated mass lesion (EML) according to Marshall classification (28.1 %). Mortality rate was 34.4 %. Within 15 min of INDO infusion, ICP decreased (Δ%: −54.6 %; P < 0.0001), CPP increased (Δ%: +44.0 %; P < 0.0001), and the remaining was stable during the entire infusion period. Patients with good outcome (n = 12) showed a greater increase of CPP during INDO test (P = 0.028). CPP response to INDO test discriminated moderately well surviving patients (AUC = 0.751; P = 0.0098) and those with good functional recovery (AUC = 0.763; P = 0.0035) from those who died and from those with worse functional outcome, respectively. No adverse events were observed.
Conclusions
INDO appears effective in reducing ICP and improving CPP in RICH. INDO test could be a useful tool in identifying RICH patients with favorable outcome. Future studies are needed.




Similar content being viewed by others
References
Zammit C, Knight WA. Severe traumatic brain injury in adults. Emerg Med Pract. 2013;15:1–28.
Mauritz W, Wilbacher I, Majdan M, et al. Epidemiology, treatment and outcome of patients after severe traumatic brain injury in European regions with different economic status. Eur J Public Health. 2008;18:575–80.
Maas AI, Stocchetti N, Bullock R. Moderate and severe traumatic brain injury in adults. Lancet Neurol. 2008;7:728–41.
Rutland-Brown W, Langlois JA, Thomas KE, Xi YL. Incidence of traumatic brain injury in the United States, 2003. J Head Trauma Rehabil. 2006;21:544–8.
Miller JD, Becker DP, Ward JD, Sullivan HG, Adams WE, Rosner MJ. Significance of intracranial hypertension in severe head injury. J Neurosurg. 1977;47:503–16.
Rangel-Castilla L, Gopinath S, Robertson CS. Management of intracranial hypertension. Neurol Clin. 2008;26:521–41.
Meyer MJ, Megyesi J, Meythaler J, et al. Acute management of acquired brain injury part I: an evidence-based review of non-pharmacological interventions. Brain Inj. 2010;24:694–705.
Meyer MJ, Megyesi J, Meythaler J, et al. Acute management of acquired brain injury part II: an evidence-based review of pharmacological interventions. Brain Inj. 2010;24:706–21.
Biestro AA, Alberti RA, Soca AE, Cancela M, Puppo CB, Borovich B. Use of indomethacin in brain-injured patients with cerebral perfusion pressure impairment: preliminary report. J Neurosurg. 1995;83:627–30.
Clemmesen JO, Hansen BA, Larsen FS. Indomethacin normalizes intracranial pressure in acute liver failure: a twenty-three-year-old woman treated with indomethacin. Hepatology. 1997;26:1423–5.
Imberti R, Fuardo M, Bellinzona G, Pagani M, Langer M. The use of indomethacin in the treatment of plateau waves: effects on cerebral perfusion and oxygenation. J Neurosurg. 2005;102:455–9.
Jensen K, Ohrstrom J, Cold GE, Astrup J. The effects of indomethacin on intracranial pressure, cerebral blood flow and cerebral metabolism in patients with severe head injury and intracranial hypertension. Acta Neurochir (Wien). 1991;108:116–21.
Godoy DA, Rabinstein AA, Biestro A, Ainslie PN, Di Napoli M. Effects of indomethacin test on intracranial pressure and cerebral hemodynamics in patients with refractory intracranial hypertension: a feasibility study. Neurosurgery. 2012;71:245–57 discussion 57-8.
Rasmussen M. Treatment of elevated intracranial pressure with indomethacin: friend or foe? Acta Anaesthesiol Scand. 2005;49:341–50.
Roberts RG, Redman JW. Indomethacin: a review of its role in the management of traumatic brain injury. Crit Care Resusc. 2002;4:271–80.
Slavik RS, Rhoney DH. Indomethacin: a review of its cerebral blood flow effects and potential use for controlling intracranial pressure in traumatic brain injury patients. Neurol Res. 1999;21:491–9.
Dahl B, Bergholt B, Cold GE, et al. CO(2) and indomethacin vasoreactivity in patients with head injury. Acta Neurochir (Wien). 1996;138:265–73.
Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81–4.
Marshall LF, Marshall SB, Klauber MR, et al. A new classification of head injury based on computerized tomography. Special Supplements. 1991;75:S14–20.
Foundation BT. Guidelines for the management of severe traumatic brain injury. J Neurotrauma. 2007;24:S1–106.
TBT Foundation. The American Association of Neurological Surgeons. The Joint Section on Neurotrauma and Critical Care. Guidelines for cerebral perfusion pressure. J Neurotrauma. 2000;17:507–11.
Puppo C, Lopez L, Farina G, et al. Indomethacin and cerebral autoregulation in severe head injured patients: a transcranial Doppler study. Acta Neurochir (Wien). 2007;149:139–49 discussion 49.
Wilson JT, Pettigrew LE, Teasdale GM. Structured interviews for the Glasgow Outcome Scale and the extended Glasgow Outcome Scale: guidelines for their use. J Neurotrauma. 1998;15:573–85.
Jensen K, Kjaergaard S, Malte E, Bunemann L, Therkelsen K, Knudsen F. Effect of graduated intravenous and standard rectal doses of indomethacin on cerebral blood flow in healthy volunteers. J Neurosurg Anesthesiol. 1996;8:111–6.
Rasmussen M, Tankisi A, Cold GE. The effects of indomethacin on intracranial pressure and cerebral haemodynamics in patients undergoing craniotomy: a randomised prospective study. Anaesthesia. 2004;59:229–36.
Harrigan MR, Tuteja S, Neudeck BL. Indomethacin in the management of elevated intracranial pressure: a review. J Neurotrauma. 1997;14:637–50.
Upton RN, Rasmussen M, Grant C, Martinez AM, Cold GE, Ludbrook GL. Pharmacokinetics and pharmacodynamics of indomethacin: effects on cerebral blood flow in anaesthetized sheep. Clin Exp Pharmacol Physiol. 2008;35:317–23.
Eriksson S, Hagenfeldt L, Law D, Patrono C, Pinca E, Wennmalm A. Effect of prostaglandin synthesis inhibitors on basal and carbon dioxide stimulated cerebral blood flow in man. Acta Physiol Scand. 1983;117:203–11.
Pickard J, Tamura A, Stewart M, McGeorge A, Fitch W. Prostacyclin, indomethacin and the cerebral circulation. Brain Res. 1980;197:425–31.
Pickard JD, MacDonell LA, Mackenzie ET, Harper AM. Prostaglandin-induced effects in the primate cerebral circulation. Eur J Pharmacol. 1977;43:343–51.
Quintana A, Raczka E, Quintana MA. Effects of indomethacin and diclofenac on cerebral blood flow in hypercapnic conscious rats. Eur J Pharmacol. 1988;149:385–8.
Markus HS, Vallance P, Brown MM. Differential effect of three cyclooxygenase inhibitors on human cerebral blood flow velocity and carbon dioxide reactivity. Stroke. 1994;25:1760–4.
Weigert G, Berisha F, Resch H, Karl K, Schmetterer L, Garhofer G. Effect of unspecific inhibition of cyclooxygenase by indomethacin on retinal and choroidal blood flow. Invest Ophthalmol Vis Sci. 2008;49:1065–70.
Jensen K, Freundlich M, Bunemann L, Therkelsen K, Hansen H, Cold GE. The effect of indomethacin upon cerebral blood flow in healthy volunteers. The influence of moderate hypoxia and hypercapnia. Acta Neurochir (Wien). 1993;124:114–9.
Bruhn H, Fransson P, Frahm J. Modulation of cerebral blood oxygenation by indomethacin: MRI at rest and functional brain activation. J Magn Reson Imaging. 2001;13:325–34.
Gjedde A, Johannsen P, Cold GE, Ostergaard L. Cerebral metabolic response to low blood flow: possible role of cytochrome oxidase inhibition. J Cereb Blood Flow Metab. 2005;25:1183–96.
Godoy DA, Biestro A, Puppo C. Does indomethacin cause cerebral ischemia? Acta Anaesthesiol Scand. 2005;49:1577–8.
Schumann P, Touzani O, Young AR, Verard L, Morello R, MacKenzie ET. Effects of indomethacin on cerebral blood flow and oxygen metabolism: a positron emission tomographic investigation in the anaesthetized baboon. Neurosci Lett. 1996;220:137–41.
St Lawrence KS, Ye FQ, Lewis BK, Frank JA, McLaughlin AC. Measuring the effects of indomethacin on changes in cerebral oxidative metabolism and cerebral blood flow during sensorimotor activation. Magn Reson Med. 2003;50:99–106.
Ling GS, Neal CJ. Maintaining cerebral perfusion pressure is a worthy clinical goal. Neurocrit Care. 2005;2:75–81.
Stocchetti N, Chieregato A, De Marchi M, Croci M, Benti R, Grimoldi N. High cerebral perfusion pressure improves low values of local brain tissue O2 tension (PtiO2) in focal lesions. Acta Neurochirurgica Supplement. 1998;71:162–5.
Marin-Caballos AJ, Murillo-Cabezas F, Cayuela-Dominguez A, et al. Cerebral perfusion pressure and risk of brain hypoxia in severe head injury: a prospective observational study. Crit Care. 2005;9:R670–6.
Johnston AJ, Steiner LA, Coles JP, et al. Effect of cerebral perfusion pressure augmentation on regional oxygenation and metabolism after head injury. Crit Care Med. 2005;33:189–95 discussion 255-7.
Rosner MJ, Rosner SD, Johnson AH. Cerebral perfusion pressure: management protocol and clinical results. J Neurosurg. 1995;83:949–62.
Nelson DW, Thornquist B, MacCallum RM, et al. Analyses of cerebral microdialysis in patients with traumatic brain injury: relations to intracranial pressure, cerebral perfusion pressure and catheter placement. BMC Med. 2011;9:21.
Tofteng F, Larsen FS. The effect of indomethacin on intracranial pressure, cerebral perfusion and extracellular lactate and glutamate concentrations in patients with fulminant hepatic failure. J Cereb Blood Flow Metab. 2004;24:798–804.
Cooper DJ, Rosenfeld JV, Murray L, et al. Decompressive craniectomy in diffuse traumatic brain injury. N Engl J Med. 2011;364:1493–502.
Kamel H, Navi BB, Nakagawa K, Hemphill JC 3rd, Ko NU. Hypertonic saline versus mannitol for the treatment of elevated intracranial pressure: a meta-analysis of randomized clinical trials. Crit Care Med. 2011;39:554–9.
Conflict of interest
None for all authors
Author information
Authors and Affiliations
Corresponding authors
Additional information
This paper was present in part (poster format) and was distinguished in the 10th Annual Meeting of Neurocritical Care Society, Denver, Colorado, USA. October 4–7, 2012. Neurocrit Care 2012; 17: S32.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Godoy, D.A., Alvarez, E., Manzi, R. et al. The Physiologic Effects of Indomethacin Test on CPP and ICP in Severe Traumatic Brain Injury (sTBI). Neurocrit Care 20, 230–239 (2014). https://doi.org/10.1007/s12028-013-9924-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-013-9924-0