Abstract
Background
Subarachnoid hemorrhage (SAH) has been associated with pronounced acute sympathetic activation. The purpose of this investigation is to identify demographic, clinical, radiological, and anatomical features of SAH that relate to sympathetic activation.
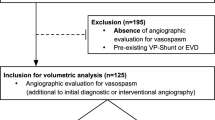
Methods
Observational study of consecutive Grades 3–5 SAH patients requiring ventriculostomy and undergoing endovascular aneurysmal obliteration. All patients underwent cerebrospinal fluid (CSF) sampling within 48 h of SAH onset, and samples were assayed for various catecholamine compounds and metabolites. Univariate analyses were performed to identify variables associated with catecholamine levels, and to correlate linearity among catecholamine compounds and metabolites. Variables demonstrating a possible association and variables of interest were entered into linear regression models to determine predictors of catecholamine elevations.
Results
Of the 102 patients, mean age was 58 years and 74% were female; 42% were Hunt–Hess (H/H) grade 4/5, 61% had a computed tomography (CT) score of 3/4, 57% had anterior cerebral or communicating artery (ACA/ACom) aneursysms, and 23% had aneurysms in the posterior circulation. In the univariate analysis, age, gender, H/H grade, CT score, and aneurysm location demonstrated various associations with catecholamine levels, and substantial positive correlations existed between the various catecholamine compounds and metabolites. Linear regression analyses revealed H/H grade to be an independent predictor of elevated CSF epinephrine (EPI), 3,4-dihydroxyphenylalanine (DOPA) and 3,4-dihydroxyphenyl acetic acid (DOPAC) levels, and of the norepinephrine/3,4-dihydroxyphenylglycol (NE/DHPG) ratio (p < 0.05 for all analyses). Female gender independently predicted increased dopamine (DA) and DOPAC levels (p < 0.05 for two analyses), as well as possibly DOPA levels (p < 0.1). Age, CT score and aneurysm location demonstrated only inconsistent associations and trends.
Conclusions
Central sympathetic activation relates to clinical severity and female gender. No definitive associations were found for age, hemorrhage amount, or aneurysm location.

Similar content being viewed by others
References
Naredi S, Lambert G, Eden E, Zall S, Runnerstam M, Rydenhag B, Friberg P. Increased sympathetic nervous activity in patients with nontraumatic subarachnoid hemorrhage. Stroke. 2000;31:901–6.
Lee V, Oh J, Mulvagh S, Wijdicks E. Mechanisms in neurogenic stress cardiomyopathy after aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2006;5:243–9.
Bruder N, Rabinstein A. Cardiovascular and pulmonary complications of aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2011;15:257–69.
Khush K, Kopelnik A, Tung P, et al. Age and aneurysm position predict patterns of left ventricular dysfunction after subarachnoid hemorrhage. J Am Soc Echo. 2005;18:168–74.
Tung P, Kopelnik A, Banki N, et al. Predictors of neurocardiogenic injury after subarachnoid hemorrhage. Stroke. 2004;35:548–53.
Eisenhofer G, Goldstein D, Stull R, Keiser H, Sunderland T, Murphy D, Kopin I. Simultaneous liquid chromatographic determination of 3,4-dihydroxyphenylglycol, catecholamines, and 3,4-dihydroxyphenylalanine in plasma, and their responses to inhibition of monoamine oxidase. Clin Chem. 1986;32:2030–3.
Kramer A, Hehir M, Nathan B, Gress D, Dumont A, Kassell N, Bleck T. A comparison of 3 radiographic scales for the prediction of delayed ischemia and prognosis following subarachnoid hemorrhage. J Neurosurg. 2008;109:199–207.
Vinken P, Bruyn G, editors. The autonomic nervous system. Amsterdam: Elsevier; 1999.
Feenstra M. Dopamine and noradrenaline release in the prefrontal cortex in relation to unconditioned and conditioned stress and reward. Prog Brain Res. 2000;126:133–63.
Raskind M, Peskind E, Holmes C, Goldstein D. Patterns of cerebrospinal fluid catechols support increased central noradrenergic responsiveness in aging and alzheimer’s disease. Biol Psychiatry. 1999;46:756–65.
Ebinger G. The significance of homovanillic acid and 3,4-dihydroxyphenylacetic acid concentrations in human lumbar cerebrospinal fluid. J Neurochem. 1987;48:1725–9.
Lenders J, Willemsen J, Beissel T, Kloppenborg P, Thien T, Benraad T. Value of the plasma norepinephrine/3,4-dihydroxyphenylglycol ratio for the diagnosis of pheochromocytoma. Am J Med. 1992;92:147–52.
Mayer S, Lin J, Homma S, et al. Myocardial injury and left ventricular performance after subarachnoid hemorrhage. Stroke. 1999;30:780–6.
Kothavale A, Banki N, Kopelnik A, et al. Predictors of left ventricular regional wall motion abnormalities after subarachnoid hemorrhage. Neurocrit Care. 2006;4:199–205.
Wittstein I, Thiemann D, Lima J, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. 2005;352:539–48.
Kopelnik A, Fisher L, Miss J, et al. Prevalence and implications of diastolic dysfunction after subarachnoid hemorrhage. Neurocrit Care. 2005;3:132–8.
Zaroff J, Pawlikowska L, Miss J, et al. Adrenoceptor polymorphisms and the risk of cardiac injury and dysfunction after subarachnoid hemorrhage. Stroke. 2006;37:1680–5.
Lambert G, Naredi S, Eden E, Rydenhag B, Friberg P. Monoamine metabolism and sympathetic nervous system activation following subarachnoid hemorrhage—influence of gender and hydrocephalus. Brain Res Bull. 2002;58:77–82.
Shivalkar B, Van Loon J, Wieland W, Tjandra-Maga T, Borgers M, Plets C, Flameng W. Variable effects of explosive or gradual increase of intracranial pressure on myocardial structure and function. Circulation. 1993;87:230–9.
Marion D, Segal R, Thompson M. Subarachnoid hemorrhage and the heart. Neurosurgery. 1986;18:101–6.
Stoddard-Apter S, Siegel A, Levin B. Plasma catecholamine and cardiovascular responses following hypothalamic stimulation in the awake cat. J Auton Nerv Syst. 1983;8:343–60.
Saito M, Moinokoshi Y, Shimazu T. Accelerated norephinephrine turnover in peripheral tissues after ventromedial hypothalamic stimulation in rats. Brain Res. 1989;481:298–303.
Melville K, Blum B, Shister H, Silver M. Cardiac ischemic changes and arrhythmias induced by hypothalamic stimulation. Am J Cardiol. 1963;12:781–91.
Neil-Dwyer G, Walter P, Cruickshank J, Doshi R, O’Gorman P. Effect of propranolol and phentolamine on myocardial necrosis after subarachnoid hemorrhage. BMJ. 1978;2:990–2.
Masuda T, Sato K, Yamamoto S, et al. Sympathetic nervous activity and myocardial damage immediately after subarachnoid hemorrhage in a unique animal model. Stroke. 2002;33:1671–6.
Doshi R, Neil-Dwyer G. Hypothalamic and myocardial lesions after subarachnoid hemorrhage. J Neurol Neurosurg Psychiatry. 1977;40:821–6.
Meyer S, Strittmatter M, Fischer C, Georg T, Schmitz B. Lateralization in autonomic dysfunction in ischemic stroke involving the insular cortex. Neuroreport. 2004;15:357–61.
Sykora M, Diedler J, Rupp A, Turcani P, Steiner T. Impaired baroreceptor reflex sensitivity in acute stroke is associated with insular involvement but not with carotid atherosclerosis. Stroke. 2009;40:737–42.
Butcher K, Cechetto D. Insular lesion invokes autonomic effects of stroke in normotensive and hypertensive rats. Stroke. 1995;26:459–65.
Fiorella D, Albuquerque F, Han P, McDougall C. Preliminary experience using the neuroform stent for the treatment of cerebral aneurysms. Neurosurgery. 2004;54:6–16.
Jayaraman M, Huy M, Versnick E, Seteinberg G, Marks M. Morphologic assessment of middle cerebral artery aneurysms for endovascular treatment. J Stroke Cerebrovasc Dis. 2007;16:52–6.
Fink J, Selim M, Kumar S, Voetsch B, Fong W, Caplan L. Insular cortex infarction in acute middle cerebral artery stroke—predictor of stroke severity and vascular lesion. Arch Neurol. 2005;62:1081–5.
Moussouttas M, Lai E, Dombrowski K, Huynh T, Khoury J, Carmona G, DeCaro M, Pacak K. CSF catecholamine profile in subarachnoid hemorrhage patients with neurogenic cardiomyopathy. Neurocrit Care. 2011;14:401–6.
Acknowledgments
The authors express gratitude to the nurses of the neurological intensive care unit from the Jefferson Hospital of Neurosciences at Thomas Jefferson University Medical Center for their assistance in this project. This project represents a collaboration between the Neurocritical Care Division in the Department of Neurology at Thomas Jefferson Medical Center, and the Section on Neuroendocrinology of the Reproductive and Adult Endocrinology Program at the National Institutes of Health. This research study was supported in part by the Intramural Research Program of the NIH/NICHD.
Conflict of interest
The authors have no financial disclosures or conflicts of interest to announce.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moussouttas, M., Lai, E.W., Khoury, J. et al. Determinants of Central Sympathetic Activation in Spontaneous Primary Subarachnoid Hemorrhage. Neurocrit Care 16, 381–388 (2012). https://doi.org/10.1007/s12028-012-9673-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-012-9673-5