Abstract
During the last decades, gestational diabetes mellitus (GDM) prevalence has been on the rise. While insulin remains the gold standard treatment for GDM, metformin use during pregnancy is controversial. This review aimed to comprehensively assess the available data on the efficacy and safety of metformin during pregnancy, both for the mother and the offspring. Metformin has been validated for maternal efficacy and safety, achieving comparable glycemic control with insulin. Additionally, it reduces maternal weight gain and possibly the occurrence of hypertensive disorders. During the early neonatal period, metformin administration does not increase the risk of congenital anomalies or other major adverse effects, including lower APGAR score at 5 min, neonatal intensive care unit admissions, and respiratory distress syndrome. Several studies have demonstrated a reduction in neonatal hypoglycemia. Metformin has been associated with an increase in preterm births and lower birth weight, although this effect is controversial and depends on the indication for which it was administered. Evidence indicates possible altered fetal programming and predisposition to childhood obesity and metabolic syndrome during adulthood after use of metformin in pregnancy. With critical questions still requiring a final verdict, ongoing research on the field must be conducted.
Similar content being viewed by others
Introduction
Gestational hyperglycemia cases are exhibiting a staggering surge in recent years and health care providers have to confront and manage the associated health consequences. The adverse outcomes include spontaneous abortion, pre-eclampsia, fetal anomalies, fetal demise, macrosomia, cesarean section, neonatal hypoglycemia, and neonatal respiratory distress syndrome [1]. The 10th edition of the International Diabetes Atlas states that hyperglycemia during pregnancy affects 16.7% of pregnancies worldwide, accounting for 21.1 million affected live births [2]. According to the International Diabetes Federation (IDF), hyperglycemia in pregnancy can be classified as gestational diabetes mellitus (GDM) (80.3%), pre-gestational diabetes (10.6%), and diabetes diagnosed during pregnancy (overt diabetes) (9.1%) [2].
Universal screening for GDM at 24–28 gestational weeks has been established and is performed with a one- or a two-step approach according to various diagnostic criteria, without universal consensus [1, 3,4,5]. According to the American Diabetes Association (ADA) guidelines, GDM diagnosis can be accomplished either with the one-step 75-g oral glucose tolerance test (OGTT) (IADPSG criteria) or with the two-step approach that consists of a 50 g screening test followed by a 3-hour 100-g OGTT for positive subjects (Carpenter-Coustan criteria) [6, 7].
Invariably, management involves lifestyle modifications, including nutritional intervention, physical exercise, and weight loss, if indicated [6]. If lifestyle changes are insufficient for adequate glycemic control, pharmaceutical intervention follows [1, 3, 6]. Although insulin is the gold standard treatment during pregnancy, the risk of hypoglycemia and weight gain, as well as the financial burden, maintenance requirements and patient education time, hinder patient compliance and impede treatment acceptance [1]. Currently, only the oral agents metformin and glyburide are acceptable alternatives, as the other hypoglycemic options lack long-term safety data [1]. The available data indicate patients’ preference for the oral administration route of metformin rather than insulin’s subcutaneous injection, which has resulted in enhanced compliance and satisfaction [8,9,10]. However, caution should be taken as both agents cross the placenta, unlike insulin [11].
Guidelines for the pharmaceutical management of hyperglycemia during pregnancy vary. ADA recommends insulin as the first-line agent and suggests metformin as a secondary option, if necessary [1]. In the guidelines of the Canadian Diabetes Association, insulin remains the gold standard, while metformin is considered as an alternative approach only in patients with GDM [4]. Comparably, a board of Italian scientific societies reported that metformin could be used for diabetes in pregnancy as a second-line treatment or in addition to insulin, to reduce its dose, especially in obese women [12]. According to two expert Greek teams, which were commissioned to construct the national guidelines, no antidiabetic drug, except insulin, should be recommended during pregnancy [13,14,15]. In contrast, the UK’s NICE guidelines recommend metformin as first-line treatment and insulin only under special conditions [3]. Notably, the Italian guidelines introduce metformin considerations for pregnant women with a body mass index (BMI) over 35 kg/m2 or women with polycystic ovary syndrome (PCOS), especially when BMI is over 30 kg/m2 [12]. However, ADA recommends that metformin should be discontinued by the end of the first trimester, when prescribed pre-pregnancy in women with PCOS to assist with conception [1]. Further indications, other than obesity or PCOS, are being investigated with limited evidence [16,17,18]. Potential factors contributing to these divergences in various national guidelines include different priorities, such as economical or medico-legal considerations.
Metformin is widely prescribed to pregnant women, but its safety has yet to be established. Although initial studies of metformin during the antenatal and immediate postnatal period found no negative effect [19,20,21], recent research has suggested potential effects on fetal metabolic programming and long-term consequences [22, 23].
This review aims to comprehensively assess the available data on the efficacy and safety of metformin during pregnancy for both mother and offspring. Table 1 provides a concice summary of key attributes pertaining to the randomised controlled trials (RCTs), that will be utilised during the review.
Maternal outcomes: metformin for gestational and type 2 diabetes
Maternal weight gain
The available data consistently indicate reduced weight gain with metformin use during pregnancy compared to controls. This effect is observed regardless of treatment indication [type 2 diabetes mellitus (T2DM), GDM, PCOS] [8, 9, 20, 24,25,26,27,28,29,30,31]. The difference in weight gain ranges from 0.47 kg to 1.8 kg. Obesity significantly increases the risk of pregnancy complications related to metabolic diseases (Tables 1–3). Therefore, such complications can be reduced by minimal weight gain during pregnancy [29]. Notably, studies on the effect of metformin postpartum weight change are still inconclusive [32,33,34].
Glycemic control
Numerous studies report that metformin is equivalent or even superior to insulin in glycemic control during pregnancy [8, 20, 25, 28, 29, 31]. Glycemic control can be assessed by various modalities, such as glycated hemoglobin (HbA1c), and fasting, postprandial, and random blood glucose. Notably, the threshold for target glucose concentrations is inconsistent between study protocols. Specifically, the maximum fasting glucose concentrations range from 5.5 to 6.1 mmol/L (100 to 110 mg/dL), and postprandial concentrations were measured at 1, 1.5 or 2 h with differing limits [8, 9, 26]. Clinical trials on the topic continue to arise. EMERGE trial is an ongoing phase III placebo-controlled clinical trial studying metformin’s early initiation effectiveness and safety on GDM [35]. Another ongoing initiative is the MATCh-GDM trial, which evaluates GDM pathogenetic mechanisms, to establish a more individualized treatment approach [36].
Need for additional insulin
Insulin is added when glycemic targets are not reached during treatment with metformin. Depending on the study protocol, women in need of supplementary insulin were excluded from the analysis [27], continued in the metformin group [22], or examined as an additional group [9, 10]. In the Mig trials, 46.3% of women in the metformin group were administered add-on insulin. These patients had higher BMI and elevated glycemic concentrations at randomization compared to women who achieved their treatment goals with metformin alone [8]. Another RCT reported that the women receiving metformin and required additional insulin (20.9%) were older, had an earlier screening, and had higher fructosamine and HbA1c concentrations at baseline. Further analysis demonstrated that fructosamine at baseline could predict the need for additional insulin [relative risk (RR) 4.6, 95% CI 1.6 to 13.6; p = 0.006] [26]. In a case-control study comparing metformin with metformin plus insulin in GDM patients, 22.94% of the cohort required supplementary insulin. Fasting glucose concentrations below 90 mg/dL at screening and primiparity were associated with reduced odds of requiring combination treatment [odds ratio (OR) 0.438, 95% confidence interval (CI) 0.235 to 0.815; p = 0.009 and OR 0.28, 95% CI 0.111 to 0.704; p = 0.007, respectively]. In contrast, obesity was correlated with an increased risk for metformin failure (OR 2.072, 95% CI 1.063 to 4.039; p = 0.032) [37]. Lastly, in an RCT of T2DM, 84.9% of women in the metformin group required additional insulin [9]. A possible explanation of disparities can be variations in genetic and phenotypic characteristics of studied populations [9]. Notably, in addition to inconsistencies in group formation, the dosing, titration, and initiation of treatment vary between studies. Thus, the establishment of universal therapeutic guidelines is necessary [8, 10, 26, 27].
Pregnancy-related hypertensive disorders
Several studies support a trend for reduced risk of gestational hypertensive disorders with metformin use [9, 25, 28,29,30]. However, the evidence is inconsistent, and a definitive conclusion has yet to be reached. To our knowledge, no study reports an association of hypertensive disorders during pregnancy with metformin administration. However, the meta-analyses’ results on the topic vary. Wang et al. (2021) conclude that metformin significantly reduced the risk of pregnancy-induced hypertension (RR 0.47, 95% CI 0.27 to 0.83; p = 0.01, n = 822) and had no effect on pre-eclampsia incidence [38]. Feng et al. (2017) demonstrated lower rates of gestational hypertension and pre-eclampsia (RR 0.07, 95% CI 0.49 to 0.99; p = 0.04, n = 1660) [28]. Guo et al. (2019) suggested that pregnancy-induced hypertension risk was similar (RR 0.56, 95% CI 0.30 to 1.06; p = 0.08, n = 606) and pre-eclampsia risk was lower under metformin treatment (RR 0.57, 95% CI 0.56 to 1.74; p < 0.001, n = 3402) [20].
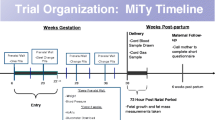
The MiTy trial compared the addition of either metformin or placebo to insulin treatment in women with T2DM. No difference was observed in the collective incidence of gestational hypertension, worsening hypertension, and pre-eclampsia between the compared groups [31]. On the contrary, Ainuddin et al. (2015) compared metformin alone (n = 16), metformin plus insulin (n = 90), and insulin alone (n = 100). Gestational hypertension was significantly less frequent in the metformin-alone group and the metformin plus insulin group compared with insulin alone (6.2%, 23.3% and 36%, respectively). Pre-eclampsia incidence was comparable across all groups [9].
Cesarean delivery
Hyperglycemia during pregnancy is a well-known risk factor for cesarean delivery [39,40,41]. Three meta-analyses, including GDM patients (n = 706, n = 1270, and n = 2611), concluded that the risk for cesarean delivery was comparable regardless of treatment modality [20, 28, 29]. However, in a recent meta-analysis, metformin administration was associated with fewer cesarean deliveries (RR 0.86, 95% CI 0.78 to 0.95; p < 0.001, n = 1693) [38].
According to the MiTy trial, cesarean section was less likely in pregnant women with T2DM who received metformin plus insulin treatment compared with placebo plus insulin (RR 0.85, 95% CI 0.73 to 0.99; p = 0.031) [31]. Another study including women with pre-gestational diabetes reported that treatment with metformin plus insulin resulted in fewer cesarean deliveries compared to metformin alone or insulin alone (52.2%, 81.2%, and 82%, respectively, p < 0.01) [9]. Table 2 summarizes the maternal outcomes of metformin use during pregnancy.
Maternal outcomes: metformin for other indications
Metformin use in pregnant women with polycystic ovary syndrome (PCOS) and obesity is a flourishing research field. Both populations are at increased risk of GDM and other pregnancy-related complications, partially attributed to the hyperglycemia and insulin resistance that characterize these conditions [42]. As an insulin-sensitizing agent, metformin reverses insulin resistance and minimizes the risk of complications. In pre-gestational diabetes, the treatment protocol starts during the first trimester [9, 17, 24]. Conversely, in GDM, treatment typically begins after 24–28 gestational weeks, when universal screening is conducted. The variation in treatment initiation affects the duration of metformin exposure and could result in differences in observed outcomes, and efficacy fluctuations, with the need for additional insulin ranging from 20.9% to 84.9%, as mentioned previously [9, 26].
The PregMet2 study included 478 pregnant women previously diagnosed with PCOS; 244 were randomized to metformin and 243 to a placebo group. Treatment was initiated during the first trimester of pregnancy. Metformin did not have any protective effect over developing GDM or hypertensive disorders during pregnancy [24]. Another RCT has also demonstrated this lack of association [43]. Neither study reported any substantial adverse effect on the mother or the offspring.
The available literature has been methodically evaluated by several meta-analyses. Zeng et al. merged the findings from 13 studies and concluded that preterm birth was negatively associated with the use of metformin during pregnancy, as well as pregnancy-induced hypertension (OR 0.22, 95% CI 0.13 to 0.38; p < 0.001) and early pregnancy loss (OR 0.19, 95% CI 0.12 to 0.28; p < 0.001) [44]. Lastly, GDM risk was statistically lower in the metformin group compared to placebo (OR 0.35, 95% CI 0.14 to 0.87; p = 0.02, n = 1080). However, the subgroup analysis exclusively in the RCTs did not confirm the association (OR 1.23, 95% CI 0.71 to 2.12; p = 0.46, n = 348) [44].
As mentioned above, metformin use in pregnancy aims to prevent the development of GDM in high-risk populations. Despite studies supporting metformin’s protective effect, most fail to establish this association [16,17,18, 24, 43,44,45,46,47,48]. The incidence of GDM was similar between metformin and control groups. Two meta-analyses evaluated the incidence of GDM in obese and overweight populations. Metformin did not reduce the risk of GDM in the pooled analysis [49, 50]. Despite its insulin-sensitizing abilities, metformin failed to prove efficient in preventing GDM development.
The exploration of metformin’s use in overweight and obese women during pregnancy is not limited to GDM prevention. Above-normal BMI measurements are associated with a wide range of maternal and neonatal complications, such as GDM, gestational hypertension, pre-eclampsia, cesarean section, as well as increased neonatal birth weight and large-for-gestational age (LGA) infants [51].
The GRoW study included overweight women (BMI 25–30 kg/m2), the EMPOWaR included obese women (BMI ≥ 30 kg/m2), and the study of Syngelaki et al. included women with BMI > 35 kg/m2 [17, 18, 47]. GDM, gestational hypertension, and birth weight were comparable across all studies in metformin and placebo groups. Pre-eclampsia rate did not differ between the metformin and placebo groups in the GRoW and EMPOWaR studies, but Syngelaki et al. reported a statistically significant reduction in frequency (OR 0.24, 95% CI 0.10 to 0.61; p = 0.001). LGA rate was similar in the GRoW trial and Syngelaki et al., while the EMPOWaR trial did not evaluate this outcome [17, 18, 47]. Notably, in a stratified analysis of the GRoW trial according to maternal BMI, the results indicated metformin’s protective effect on macrosomia (birth weight over 4000 g) in the overweight group compared with the obese [47]. The GRoW and EMPOWaR studies found no difference in overall gestational weight gain, while Syngelaki et al. reported reduced weight gain in the metformin group. A subsequent meta-analysis of the three RCTs supported that there is insufficient evidence to establish metformin’s use during pregnancy [16]. The EudraCT trial is currently ongoing and aims to evaluate metformin administration during pregnancy in obese patients after risk stratification and detection of high-risk individuals [52].
Neonatal outcomes
Gestational age/preterm birth
Numerous studies support that metformin administration in GDM treatment results in earlier gestational age compared with the control group [8, 20, 29, 30]. In the MiG trials, although the results were statistically significant (38.3 ± 1.4 vs 38.5 ± 1.3, p = 0.02), they were not clinically significant [8]. Similarly, three meta-analyses showed a mean difference (MD) of −0.14, 0.16 and 0.23 weeks [20, 29, 30]. Balsells et al. commented that although the net effect of metformin on gestational age was small (−0.16 weeks), it coincided with a 50% elevation of preterm birth rate (RR 1.50, 95% CI 1.04 to 2.16; p = 0.03, n = 1299) [30]. Guo et al. found no significant difference in the incidence of preterm birth; however, heterogeneity between studies was significant (RR 0.90, 95% CI 0.51 to 1.58; p = 0,71, I2 = 71%, n = 2943) [20]. On the contrary, metformin was not correlated with gestational age or prematurity in T2DM patients [9, 31], although no meta-analyses are available for this population.
Additionally, prematurity was examined in women with PCOS, comparing metformin to placebo. PregMet and PregMet2 found similar rates of preterm births, trending towards a protective effect of metformin [24, 43]. Moreover, a meta-analysis of this population described a significantly lower prevalence of preterm births in the metformin group (OR 0.37, 95% CI 0.20 to 0.68; p = 0.002, n = 1606). The authors also reported that metformin promoted term gestation (OR 5.23, p < 0.001) [44].
Finally, a register-based cohort study examined the effects of metformin administration on GDM, T2DM, and PCOS. Infants of mothers who received combination treatment with metformin and insulin were more likely to be preterm compared to infants exposed exclusively to insulin (OR 1.46, 95% CI 1.10 to 1.95). Notably, the rate of preterm deliveries was similar between metformin-alone and insulin-alone groups [19].
Congenital anomalies
The transplacental passage of metformin raises concerns about its effects on fetal growth, especially when taken during fetal organogenesis (4th to 12th gestational week) [53]. The current literature on the use of metformin during the first trimester is limited but reassuring regarding the risk of major congenital malformations (MCM). Studies consistently show that metformin does not increase the overall incidence of MCM compared to insulin [19,20,21, 53, 54].
In their cohort study, Lin et al. pointed out a lower risk of congenital malformations in women with pre-existing T2DM treated with metformin compared with those treated with insulin (OR 0.51, 95% CI 0.27 to 0.94; p = 0.032). The reasons are unclear, but it is tempting to speculate that women treated with metformin may have milder diabetes than those on insulin therapy [55]. A case-control study involving 50,167 babies found a higher risk of pulmonary valve atresia after metformin exposure, compared to controls, after adjustment for diabetes and other confounders. The authors recommended further surveillance to increase the sample size and follow up on the cardiac signal, as they suspect this finding to be coincidental [56].
Birth weight/SGA/LGA/macrosomia
Neonates with a birth weight below the 10th percentile are considered small-for-gestational-age (SGA), while those above the 90th percentile are considered large-for-gestational-age (LGA). Macrosomic neonates exceed 4000 g at birth. In the meta-analyses of Guo et al. and Tarry-Adkins et al., metformin-exposed neonates weighed less, with a mean difference of 114.48 (95% CI 37.32 to 191.64; p < 0.01) and 107.69 (95% CI 182.70 to 32.68; p = 0.005), respectively. Additionally, macrosomia incidence was significantly lower, but no difference was observed in SGA and LGA infant rates [20, 57].
Regarding pre-gestational diabetes, Ainuddin et al. estimated comparable birth weight across all groups – metformin alone, insulin alone and combination treatment [9]. The MiTy study reported a statistically significant reduction in birth weight, elevation in the rate of SGA and reduction in the rate of macrosomia in offspring exposed to insulin and metformin combined, compared to insulin with placebo (p = 0.0016, p = 0.026, p = 0.046 respectively). The incidence of LGA was similar in both groups [31]. Birth weight was not affected by metformin treatment in the offspring of women with PCOS [24, 43]. Another cohort study reported that metformin-exposed neonates were more likely to be SGA (OR 1.65, 95% CI 1.16 to 2.34), while the combination therapy group presented an increased risk for LGA [19].
Neonatal hypoglycemia
Various studies support that metformin for the treatment of GDM reduces the risk of neonatal hypoglycemia in the offspring [8, 10, 20, 28, 38]. The threshold point of hypoglycemia was not consistent throughout studies, ranging from glucose concentrations <1.4 to <2.6 mmol/L [8, 9]. Ainuddin et al. did not confirm metformin’s protective effect in women with T2DM. However, the combination of metformin with insulin resulted in a significant decrease in neonatal hypoglycemia (metformin plus insulin: 7.8%, insulin alone: 30%, p < 0.01) [9]. The MiTy trial reported a comparable incidence of neonatal hypoglycemia between insulin plus metformin versus insulin plus placebo in patients with T2DM (RR 0.82, 95% CI 0.52 to 1.30) [31]. In a retrospective cohort study, metformin was associated with a reduced risk for neonatal hypoglycemia, regardless of treatment indication. Surprisingly, the combination of metformin with insulin was associated with an increased risk for hypoglycemia in neonates [19].
Other neonatal complications
The collective verdict from multiple RCTs and meta-analyses is that metformin administration during pregnancy is not associated with NICU admissions, respiratory distress syndrome, or reduced APGAR score at 5 min [9, 10, 17, 20, 22, 26, 29, 31, 38, 43, 47]. Table 3 summarizes the neonatal outcomes of metformin use during pregnancy.
Childhood outcomes
Offspring of mothers with GDM from the MiG trial were divided into medical centers in Adelaide and Auckland to examine the long-term effects of intrauterine exposure to metformin. In Adelaide (metformin: n = 58, insulin: n = 51), no difference was detected in anthropometric measures at the 2- and 7-year checkpoint. Conversely, in Auckland (metformin: n = 45, insulin: n = 54), the 2-year-old metformin-exposed offspring had significantly higher measurements in BMI, chest, mid-arm, waist and hip circumference, waist-to-hip ratio, subscapular and bicep folds. At the age of 9 years, they continued to have higher weight, mid-arm and waist circumference, waist-to-height ratio, and upper arm fat mass. Additionally, metformin and insulin groups had comparable body fat mass and subcutaneous, visceral, and total abdominal mass percentages. Mothers in the metformin group had higher BMI and the associations remained after adjustment for maternal BMI and weight [22]. A follow-up study of the MiG offspring reported no neurodevelopmental effect at the age of 2 years [58]. Another meta-analysis indicated that metformin exposure resulted in heavier offspring with similar height between 18 months and 2 years old; however, the results were inconsistent at 5-9 years old. BMI was significantly higher in the metformin-exposed group of the same age (MD 0.78, 95% CI 0.23 to 1.33; p = 0.005) [57].
Corresponding studies were conducted on the offspring of women with PCOS, comparing metformin to placebo. Offspring exposed to placebo demonstrated higher weight, BMI, and overweight/obesity ratio at 4 years of age, with no difference in height. This relation was apparent from 6 months of age. Adjustment for pre-pregnancy maternal BMI did not alter the results [59]. Offspring from the PregMet trial were examined in the PedMet study at 5–10 years old. Data showed a link between metformin exposure and increased BMI, obesity, waist circumference, and waist-to-height ratio, with no difference in height alone. Maternal pre-pregnancy BMI > 30 kg/m2 was correlated with higher adiposity in the metformin group [23]. Lastly, a register-based cohort compared the long-term effects of metformin-alone, metformin plus insulin, and insulin-alone intrauterine exposure. No difference was reported in obesity and motor-social developmental outcomes [19].
Although there is limited available data, intrauterine exposure to metformin has been accused of impairing the reproductive health of the offspring. Animal studies have shown that metformin exposure in utero is associated with reduced testicular size and growth, as well as with reduced testosterone production [60, 61]. However, no difference was noted in the testicular size of boys aged 33 to 85 months born by mothers with GDM randomized to metformin or insulin [62].
Pharmacokinetics
Metformin’s transplacental transmission is one major concern that impedes its official authorization in pregnancy. The concentrations in the umbilical cord blood range from 50-100% of the maternal [63]. Metformin is a substrate of many cellular transportation systems, including organic cation transporter proteins (OCT3), expressed in the placental tissue and are the main effectors in transplacental passage. OCT3 expression is low during the first trimester and increases progressively with gestational age [64]. In parallel, the mitochondria, which are metformin’s main site of action, are few and immature at the early stages of gestation and develop gradually with fetal growth [65]. Consequently, the above mechanism supports metformin’s safety in early gestation and the absence of risk for congenital anomalies, as demonstrated in clinical studies [20, 21, 54].
However, the overall effect of metformin administration in pregnancy has yet to be determined. It has been suggested that metformin can affect fetal growth, nutrient bioavailability, and epigenetic programming [64, 65]. Metformin shifts the cellular metabolism from anabolic to a catabolic state, and suppresses growth and the transplacental transmission of nutrients (amino acids, glucose) – despite the nutrient-rich environment [65]. The resulting calorie depletion could explain the observed trend for reduced neonatal birth weight and SGA incidence following metformin use in pregnancy [64]. The catabolic state and nutrient restriction sustain a developmental environment that predisposes to cardiometabolic disease in adulthood (“thrifty hypothesis”) [66].
Prenatal metformin exposure leads to significant changes in the hepatic gene expression profile. The insulin-induced gene-1 (Insig-1) is involved in lipogenesis and adipogenesis, and its expression is upregulated in adipose tissue in response to a high-fat diet. In response to prenatal metformin exposure, Insig-1 mRNA expression was upregulated approximately threefold in male mice offspring, and a similar trend was observed in females without statistical significance [67]. H19 gene expression is also upregulated. Normally, its expression is negligible in adult liver, but it increases in individuals with T2DM. H19 overexpression reduces methylation and upregulates hepatocyte nuclear factor 4α (Hnf4α) expression, activating of the gluconeogenic program, resulting in altered hepatic differentiation and premature gluconeogenesis gene expression [68]. Additionally, data suggest an implication of metformin in the bioavailability of methyl donors, such as folic acid and vitamin B12, as well as a direct effect on one-carbon metabolism. These changes result in DNA hypomethylation and differential epigenetic signaling. Thus, metformin activity during fetal growth can permanently alter the metabolic programming of the body [64].
Metformin’s effect along with the diet followed during pregnancy was examined. Specifically, metformin administration to mothers who followed a regular diet during pregnancy predisposed to offspring obesity and male-specific glucose intolerance during adulthood in response to a high-fat diet [69]. Conversely, metformin administration to mothers who followed a high-fat diet during pregnancy had a protective effect on metabolic programming, resulting in reduced weight, adipose tissue gain, and glucose intolerance in both sexes when exposed to a high-fat diet during adulthood [67]. To correctly appreciate the results of in vivo experiments on rodents, it is critical to acknowledge the differences in fetal development between mice and humans. Mice are born immediately after organogenesis and organ maturation occurs during the neonatal period. On the contrary, most organ development in humans is achieved in utero [70].
Another researched field is the mechanism of metformin’s protective effect over gestational hypertensive disorders, which has been demonstrated in multiple studies [9, 25, 28, 30]. The most prominent hypothesis attributes metformin’s protective qualities to a pro-angiogenic effect. Elevation of pro-angiogenic factors like vascular endothelial growth factor (VEGF) and matrix metalloproteionase-2 (MMP-2) and inhibition of anti-angiogenic modulators like sFlt-1 and sEng, facilitate adequate trophoblast invasion and fetoplacental circulation, thus reducing hypertensive disorders [71, 72]. A different approach focuses on a potential anti-inflammatory action, thereby reducing endothelial dysfunction. Specifically, metformin’s use resulted in a reversal of lipopolysaccharide (LPS)-induced pre-eclampsia in mice, with concomitant suppression of the nFkB pathway and inflammatory modulators. Interestingly, a reduction of CRP concentrations was noted in pregnant women taking metformin compared with placebo. However, no difference was observed when compared with insulin. The authors concluded that the anti-inflammatory effect might be attributed to a general hypoglycemic effect and not to a discrete property of metformin itself [71, 73]. Based on metformin’s speculated protective endothelial effect, its utility in preterm pre-eclampsia for prolonging gestation is being examined, without evidence yet [74].
Conclusions
In conclusion, metformin has the potential to constitute an alternative to insulin treatment during pregnancy, as it has equally effective results on glycemic control at a significantly lower cost. Also, the oral administration route is an inherent advantage, which enhances compliance and favors metformin in patients’ preferences. Nevertheless, its use during pregnancy remains controversial. The available data support that metformin is not associated with congenital defects. Moreover, metformin administration was associated with reduced maternal weight gain, incidence of hypertensive disorders, and neonatal hypoglycemia. However, evidence indicating altered fetal programming and predisposition to childhood obesity and metabolic syndrome during adulthood impede metformin’s universal use during pregnancy. As critical questions still require a final verdict, ongoing research on the field must be conducted.
References
American Diabetes Association Professional Practice Committee: 15, Management of diabetes in pregnancy: standards of medical care in diabetes-2022. Diabetes Care 45, 232–43 (2022). https://doi.org/10.2337/dc22-S015
IDF Diabetes Atlas. Int. Diabetes Fed. (2021). https://doi.org/10.1016/j.diabres.2013.10.013
National Institute for Health and Care Excellence (NICE). Diabetes in Pregnancy: Management of Diabetes and its Complications from Pre-conception to the Postnatal Period (NG3), NG3 edn. (National Institute for Health and Care Excellence, 2015) https://www.nice.org.uk/guidance/ng3
Diabetes Canada Clinical Practice Guidelines Expert Committee, D.S. Feig, H. Berger, L. Donovan, A. Godbout, T. Kader, E. Keely et al. Diabetes and pregnancy. Can. J. Diabetes 42, 255–82 (2018). https://doi.org/10.1016/j.jcjd.2017.10.038
M. Hod, A. Kapur, D.A. Sacks, E. Hadar, M. Agarwal, G.C. Di Renzo et al. The International Federation of Gynecology and Obstetrics (FIGO) Initiative on Gestational Diabetes Mellitus: a pragmatic guide for diagnosis, management, and care. Int. J. Gynecol. Obstet. 131, S173–211 (2015)
S.A. Paschou, E. Bletsa, M. Papazisi, N. Mili, F. Kanouta, G.N. Kassi et al. Screening and management of major endocrinopathies during pregnancy: an update. Endocrine 1–10 (2022). https://doi.org/10.1007/S12020-022-03237-Y/TABLES/2
K.W. Davidson, M.J. Barry, C.M. Mangione, M. Cabana, A.B. Caughey, E.M. Davis et al. Screening for gestational diabetes: US Preventive Services Task Force recommendation statement. JAMA 326, 531–538 (2021). https://doi.org/10.1001/JAMA.2021.11922
J.A. Rowan, W.M. Hague, W. Gao, M.R. Battin, M. Peter Moore, Metformin versus insulin for the treatment of gestational diabetes. N. Engl. J. Med. 358, 2003–18 (2008)
J.A. Ainuddin, N. Karim, S. Zaheer, S. Sanwer Ali, A. Ara Hasan, Metformin treatment in type 2 diabetes in pregnancy: an active controlled, parallel-group, randomized, open label study in patients with type 2 diabetes in pregnancy. (2015). https://doi.org/10.1155/2015/325851
J.A. Ainuddin, N. Karim, A.A. Hasan, S.A. Naqvi, Metformin versus insulin treatment in gestational diabetes in pregnancy in a developing country: a randomized control trial. Diabetes Res. Clin. Pract. 107, 290–9 (2015). https://doi.org/10.1016/J.DIABRES.2014.10.001
F. Garcia-Bournissen, D.S. Feig, G. Koren, Maternal-fetal transport of hypoglycaemic drugs. Clin. Pharmacokinet. 42, 303–13 (2003). https://doi.org/10.2165/00003088-200342040-00001
L. Sciacca, C. Bianchi, S. Burlina, G. Formoso, E. Manicardi, M.A. Sculli et al. Position paper of the Italian Association of Medical Diabetologists (AMD), Italian Society of Diabetology (SID), and the Italian Study Group of Diabetes in pregnancy: metformin use in pregnancy. Acta Diabetol. 60, 1421–37 (2023). https://doi.org/10.1007/S00592-023-02137-5/TABLES/15
E. Anastasiou, G. Farmakidis, A. Gerede, D.G. Goulis, E. Koukkou, A. Kourtis et al. Clinical practice guidelines on diabetes mellitus and pregnancy: Ι. Pre-existing type 1 and type 2 diabetes mellitus. Hormones 19, 593–600 (2020). https://doi.org/10.1007/S42000-020-00192-Z
E. Anastasiou, G. Farmakidis, A. Gerede, D.G. Goulis, E. Koukkou, A. Kourtis et al. Clinical practice guidelines on diabetes mellitus and pregnancy: ΙI. Gestational diabetes mellitus. Hormones 19, 601–7 (2020). https://doi.org/10.1007/S42000-020-00193-Y
Hellenic Diabetes Association, G. Dimitriadis, I. Ioannidis, K. Makrilakis, A. Mavrogiannaki, A. Melidonis, I. Migdalis et al. Guidelines for Diabetes Mellitus. 5 (2023). https://www.ede.gr
J.M. Dodd, R.M. Grivell, A.R. Deussen, W.M., Hague, Metformin for women who are overweight or obese during pregnancy for improving maternal and infant outcomes. Cochrane Database Syst. Rev. (2018). https://doi.org/10.1002/14651858.CD010564.pub2
A. Syngelaki, K.H. Nicolaides, J. Balani, S. Hyer, R. Akolekar, R. Kotecha et al. Metformin versus placebo in obese pregnant women without diabetes mellitus. N. Engl. J. Med. 374, 434–43 (2016). https://doi.org/10.1056/NEJMOA1509819/SUPPL_FILE/NEJMOA1509819_DISCLOSURES.PDF
C. Chiswick, R.M. Reynolds, F. Denison, A.J. Drake, S. Forbes, D.E. Newby et al. Effect of metformin on maternal and fetal outcomes in obese pregnant women (EMPOWaR): a randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol. 3, 778–86 (2015). https://doi.org/10.1016/S2213-8587(15)00219-3
K.M.G. Brand, L. Saarelainen, J. Sonajalg, E. Boutmy, C. Foch, M. Vääräsmäki et al. Metformin in pregnancy and risk of adverse long-term outcomes: a register-based cohort study. BMJ Open Diabetes Res. Care. 10, 2363 (2022). https://doi.org/10.1136/BMJDRC-2021-002363
L. Guo, J. Ma, J. Tang, D. Hu, W. Zhang, X. Zhao Comparative efficacy and safety of metformin, glyburide, and insulin in treating gestational diabetes mellitus: a meta-analysis. J. Diabetes Res. 2019, 9084708 (2019). https://doi.org/10.1155/2019/9804708
C. Gilbert, M. Valois, G. Koren, Pregnancy outcome after first-trimester exposure to metformin: a meta-analysis. Fertil. Steril. 86, 658–63 (2006). https://doi.org/10.1016/J.FERTNSTERT.2006.02.098
J.A. Rowan, E.C. Rush, L.D. Plank, J. Lu, V. Obolonkin, S. Coat et al. Metformin in gestational diabetes: the offspring follow-up (MiG TOFU): body composition and metabolic outcomes at 7–9 years of age. BMJ Open Diabetes Res. Care. 6, 456 (2018). https://doi.org/10.1136/BMJDRC-2017-000456
L.G.E. Hanem, Ø. Salvesen, P.B. Juliusson, S.M. Carlsen, M.C.F. Nossum, M.Ø. Vaage et al. Intrauterine metformin exposure and offspring cardiometabolic risk factors (PedMet study): a 5–10 year follow-up of the PregMet randomised controlled trial. Lancet Child Adolesc. Health 3, 166–74 (2019). https://doi.org/10.1016/S2352-4642(18)30385-7
T.S. Løvvik, S.M. Carlsen, Ø. Salvesen, B. Steffensen, M. Bixo, F. Gómez-Real et al. Use of metformin to treat pregnant women with polycystic ovary syndrome (PregMet2): a randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol. 7, 256–66 (2019). https://doi.org/10.1016/S2213-8587(19)30002-6
L.-P. Zhao, X.-Y. Sheng, S. Zhou, T. Yang, L.-Y. Ma, Y. Zhou et al. Metformin versus insulin for gestational diabetes mellitus: a meta-analysis (2015). https://doi.org/10.1111/bcp.12672
K. Tertti, U. Ekblad, P. Koskinen, T. Vahlberg, T. Rönnemaa, Metformin vs. insulin in gestational diabetes. A randomized study characterizing metformin patients needing additional insulin. Diabetes Obes. Metab. 15, 246–51 (2013). https://doi.org/10.1111/DOM.12017
S.R. Eid, R.S.I. Moustafa, M.M. Salah, S.K. Hanafy, R.H. Aly, W.F.G. Mostafa et al. Is metformin a viable alternative to insulin in the treatment of gestational diabetes mellitus (GDM)? Comparison of maternal and neonatal outcomes. Egypt Pediatr. Assoc. Gaz 66, 15–21 (2018). https://doi.org/10.1016/J.EPAG.2018.01.002
Y. Feng, H. Yang, Metformin–a potentially effective drug for gestational diabetes mellitus: a systematic review and meta-analysis. J. Matern. Fetal Neonatal Med. 30, 1874–81 (2017). https://doi.org/10.1080/14767058.2016.1228061
J. Gui, Q. Liu, L. Feng, Metformin vs insulin in the management of gestational diabetes: a meta-analysis. PLoS ONE 8 (2013). https://doi.org/10.1371/JOURNAL.PONE.0064585
M. Balsells, A. García-Patterson, I. Solà, M. Roqué, I. Gich, R. Corcoy, Glibenclamide, metformin, and insulin for the treatment of gestational diabetes: a systematic review and meta-analysis. BMJ 350 (2015). https://doi.org/10.1136/BMJ.H102
D.S. Feig, L.E. Donovan, B. Zinman, J.J. Sanchez, E. Asztalos, E.A. Ryan et al. Metformin in women with type 2 diabetes in pregnancy (MiTy): a multicentre, international, randomised, placebo-controlled trial. Lancet Diabetes Endocrinol. 8, 834–44 (2020). https://doi.org/10.1016/S2213-8587(20)30310-7
S.M. Carlsen, M.P. Martinussen, E. Vanky, Metformin’s effect on first-year weight gain: a follow-up study. Pediatrics 130 (2012). https://doi.org/10.1542/peds.2012-0346.
O. Pellonperä, T. Rönemma, U. Ekblad, T. Vahlberg, K. Tertti, The effects of metformin treatment of gestational diabetes on maternal. Acta Obstet. Gynecol. Scand 95, 79–87 (2016). https://doi.org/10.1111/aogs.12788
M. Jahanshahi, A.R. Shahmirzadi, E. Kashani, R. Alipoor, S. Vosough, Effects of metformin and insulin therapy regimens on postpartum oral glucose tolerance test results in pregnant women with gestational diabetes mellitus: a comparative study. Horm. Mol. Biol. Clin. Investig. 41 (2020). https://doi.org/10.1515/hmbci-2020-0018
F. Dunne, C. Newman, D. Devane, A. Smyth, A. Alvarez-Iglesias, P. Gillespie et al. A randomised placebo-controlled trial of the effectiveness of early metformin in addition to usual care in the reduction of gestational diabetes mellitus effects (EMERGE): study protocol. Trials 23 (2022). https://doi.org/10.1186/S13063-022-06694-Y
ClinicalTrials.gov, Metabolic analysis for treatment choice in gestational diabetes mellitus - full text view (n.d). https://clinicaltrials.gov/ct2/show/NCT03029702. Accessed 24 Jan 2023.
M.L.R. De Souza, R.R.E. Silva, T.R.E. Silva, L.C. De Oliveira, G. Dienstmann, I.B. Do Nascimento et al. Factors associated with the need for insulin as a complementary treatment to metformin in gestational diabetes mellitus. Revisita Bras. Ginecol. Obstet. 41, 697–702 (2019). https://doi.org/10.1055/S-0039-1700796
X. Wang, W. Liu, H. Chen, Q. Chen, Comparison of insulin, metformin, and glyburide on perinatal complications of gestational diabetes mellitus: a systematic review and meta-analysis. Gynecol. Obstet. Invest. 86, 218–30 (2021). https://doi.org/10.1159/000515893
R. Gorgal, E. Gonçalves, M. Barros, G. Namora, Â. Magalhães, T. Rodrigues et al. Gestational diabetes mellitus: a risk factor for non-elective cesarean section. J. Obstet. Gynaecol. Res. 38, 154–9 (2012). https://doi.org/10.1111/J.1447-0756.2011.01659.X
D. Boriboonhirunsarn, R. Waiyanikorn, Emergency cesarean section rate between women with gestational diabetes and normal pregnant women. Taiwan J. Obstet. Gynecol. 55, 64–7 (2016). https://doi.org/10.1016/J.TJOG.2015.08.024
H.M. Ehrenberg, C.P. Durnwald, P. Catalano, B.M. Mercer, The influence of obesity and diabetes on the risk of cesarean delivery. Am. J. Obstet. Gynecol. 191, 969–74 (2004). https://doi.org/10.1016/J.AJOG.2004.06.057
S. Palomba, M.A. De Wilde, A. Falbo, M.P.H. Koster, G.B. La Sala, B.C.J.M. Fauser, Pregnancy complications in women with polycystic ovary syndrome. Hum. Reprod. Update 21, 575–92 (2015). https://doi.org/10.1093/HUMUPD/DMV029
E. Vanky, S. Stridsklev, R. Heimstad, P. Romundstad, K. Skogøy, O. Kleggetveit et al. Metformin versus placebo from first trimester to delivery in polycystic ovary syndrome: a randomized, controlled multicenter study (2010). https://doi.org/10.1210/jc.2010-0853
X.-L. Zeng, Y.-F. Zhang, Q. Tian, Y. Xue, R.-F. An, Effects of metformin on pregnancy outcomes in women with polycystic ovary syndrome A meta-analysis. Medicine 95 (2016). https://doi.org/10.1097/MD.0000000000004526
V. De Leo, M.C. Musacchio, P. Piomboni, A. Di Sabatino, G. Morgante, The administration of metformin during pregnancy reduces polycystic ovary syndrome related gestational complications. Eur. J. Obstet. Gynecol. Reprod. Biol. 157, 63–6 (2011). https://doi.org/10.1016/j.ejogrb.2011.03.024
C.J. Glueck, P. Wang, N. Goldenberg, L. Sieve-Smith, Pregnancy outcomes among women with polycystic ovary syndrome treated with metformin. Hum. Reprod. 17, 2858–64 (2002). https://doi.org/10.1093/HUMREP/17.11.2858
J.M. Dodd, J. Louise, A.R. Deussen, R.M. Grivell, G. Dekker, A.J. McPhee et al. Effect of metformin in addition to dietary and lifestyle advice for pregnant women who are overweight or obese: the GRoW randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol. 7, 15–24 (2019). https://doi.org/10.1016/S2213-8587(18)30310-3
E. Valdés, A. Sepúlveda-Martínez, P. Candia, N. Abusada, R. Orellana, B. Manukian et al. Metformin as a prophylactic treatment of gestational diabetes in pregnant patients with pregestational insulin resistance: a randomized study. J. Obstet. Gynaecol. Res. 44, 81–6 (2018). https://doi.org/10.1111/JOG.13477
S.A.R. Doi, L. Furuya-Kanamori, E. Toft, O.A.H. Musa, N. Islam, J. Clark et al. Metformin in pregnancy to avert gestational diabetes in women at high risk: Meta-analysis of randomized controlled trials. Obes. Rev. 21, e12964 (2020). https://doi.org/10.1111/OBR.12964
J.L. Tarry-Adkins, S.E. Ozanne, C.E. Aiken, Impact of metformin treatment during pregnancy on maternal outcomes: a systematic review/meta-analysis. Sci. Rep. 111, 1–13 (2021). https://doi.org/10.1038/s41598-021-88650-5
S. Joy, N. Istwan, D. Rhea, C. Desch, G. Stanziano, The impact of maternal obesity on the incidence of adverse pregnancy outcomes in high-risk term pregnancies. Am. J. Perinatol. 26, 345–9 (2009). https://doi.org/10.1055/S-0028-1110084
Clinical Trials Register - Search for eudract_number:2018-000003-16 (n.d). https://www.clinicaltrialsregister.eu/ctr-search/search?query=eudract_number:2018-000003-16. Accessed 24 Jan 2023
O. Diav-Citrin, S. Steinmetz-Shoob, S. Shechtman, A. Ornoy, In-utero exposure to metformin for type 2 diabetes or polycystic ovary syndrome: a prospective comparative observational study. Reprod. Toxicol. 80, 85–91 (2018). https://doi.org/10.1016/J.REPROTOX.2018.05.007
S. Scherneck, N. Schlinke, E. Beck, K. Grupe, C. Weber-Schoendorfer, C. Schaefer, Pregnancy outcome after first-trimester exposure to metformin: a prospective cohort study. Reprod. Toxicol. 81, 79–83 (2018). https://doi.org/10.1016/J.REPROTOX.2018.07.004
S.F. Lin, S.H. Chang, C.-F. Kuo, W.-T. Lin, M.-J. Chiou, Y.T. Huang, Association of pregnancy outcomes in women with type 2 diabetes treated with metformin versus insulin when becoming pregnant. BMC Pregnancy Childbirth 20 (2020). https://doi.org/10.1186/S12884-020-03207-0
J.E. Given, M. Loane, E. Garne, M.C. Addor, M. Bakker, B. Bertaut-Nativel et al. Metformin exposure in first trimester of pregnancy and risk of all or specific congenital anomalies: exploratory case-control study. BMJ 361 (2018). https://doi.org/10.1136/BMJ.K2477
J.L. Tarry-Adkins, C.E. Aiken, S.E. Ozanne, Neonatal, infant, and childhood growth following metformin versus insulin treatment for gestational diabetes: a systematic review and meta-analysis. PLoS Med. 16 (2019). https://doi.org/10.1371/JOURNAL.PMED.1002848
T.A. Wouldes, M. Battin, S. Coat, E.C. Rush, W.M. Hague, J.A. Rowan, Neurodevelopmental outcome at 2 years in offspring of women randomised to metformin or insulin treatment for gestational diabetes. Arch. Dis. Child Fetal Neonatal Ed 101, F488–93 (2016). https://doi.org/10.1136/ARCHDISCHILD-2015-309602
L. Guro, E. Hanem, S. Stridsklev, Ø. Salvesen, M. Roelants, S.M. Carlsen et al. Metformin use in PCOS pregnancies increases the risk of offspring overweight at 4 years of age: follow-up of two RCTs. J. Clin. Endocrinol. Metab. 103, 1612–21 (2018). https://doi.org/10.1210/jc.2017-02419
S.A. Paschou, B.H.R. Wolffenbuttel, Metformin use during pregnancy: is it really safe? J. Diabetes 10, 984–5 (2018). https://doi.org/10.1111/1753-0407.12813
P. Tartarin, D. Moison, E. Guibert, J. Dupont, R. Habert, V. Rouiller-Fabre et al. Metformin exposure affects human and mouse fetal testicular cells. Hum. Reprod. 27, 3304–14 (2012). https://doi.org/10.1093/HUMREP/DES264
K. Tertti, J. Toppari, H.E. Virtanen, S. Sadov, T. Rönnemaa, Metformin treatment does not affect testicular size in offspring born to mothers with gestational diabetes. Rev. Diabet. Stud. 13, 59 (2016). https://doi.org/10.1900/RDS.2016.13.59
S. Eyal, T.R. Easterling, D. Carr, J.G. Umans, M. Miodovnik, G.D. Hankins et al. Pharmacokinetics of metformin during pregnancy. Drug Metab. Distrib. 38, 833–40 (2010). https://doi.org/10.1124/dmd.109.031245
M.D. Owen, B.C. Baker, E.M. Scott, K. Forbes, Interaction between metformin, folate and vitamin B12 and the potential impact on fetal growth and long-term metabolic health in diabetic pregnancies. Int. J. Mol. Sci. 22 (2021). https://doi.org/10.3390/IJMS22115759
L.A. Barbour, C. Scifres, A.M. Valent, J.E. Friedman, T.A. Buchanan, D. Coustan et al. A cautionary response to SMFM statement: pharmacological treatment of gestational diabetes. Am. J. Obstet. Gynecol. 219, 367.e1 (2018). https://doi.org/10.1016/J.AJOG.2018.06.013
C.N. Hales, D.J.P. Barker, Type 2 (non-insulin-dependent) diabetes mellitus: the thrifty phenotype hypothesis. Diabetologia 35, 595–601 (1992). https://doi.org/10.1007/BF00400248
H. Salomäki, M. Heinäniemi, L.H. Vähätalo, L. Ailanen, K. Eerola, S.T. Ruohonen et al. Prenatal metformin exposure in a maternal high fat diet mouse model alters the transcriptome and modifies the metabolic responses of the offspring. PLoS ONE 9 (2014). https://doi.org/10.1371/journal.pone.0115778
J. Deng, M. Mueller, T. Geng, Y. Shen, Y. Liu, P. Hou et al. H19 lncrna alters methylation and expression of hnf4α in the liver of metformin-exposed fetuses. Cell Death Dis. 8, 1–8 (2017). https://doi.org/10.1038/cddis.2017.392
H. Salomäki, L.H. Vähätalo, K. Laurila, N.T. Jäppinen, A.M. Penttinen, L. Ailanen et al. Prenatal metformin exposure in mice programs the metabolic phenotype of the offspring during a high fat diet at adulthood. PLoS ONE 8 (2013). https://doi.org/10.1371/JOURNAL.PONE.0056594
L. Nguyen, S.-Y. Chan, A.K.K. Teo, Metformin from mother to unborn child - are there unwarranted effects? EBioMedicine 35, 394–404 (2018). https://doi.org/10.1016/j.ebiom.2018.08.047
A.R. Anness, A. Baldo, D.R. Webb, A. Khalil, T.G. Robinson, H.A. Mousa, Effect of metformin on biomarkers of placental- mediated disease: a systematic review and meta-analysis. Placenta 107, 51–8 (2021). https://doi.org/10.1016/J.PLACENTA.2021.02.021
F. Wang, G. Cao, W. Yi, L. Li, X. Cao, Effect of metformin on a preeclampsia-like mouse model induced by high-fat diet. Biomed. Res. Int. 2019 (2019). https://doi.org/10.1155/2019/6547019
J. Hu, J. Zhang, B. Zhu, Protective effect of metformin on a rat model of lipopolysaccharide-induced preeclampsia. Fundam. Clin. Pharmacol. 33, 649–58 (2019). https://doi.org/10.1111/FCP.12501
C.A. Cluver, R. Hiscock, E.H. Decloedt, D.R. Hall, S. Schell, B.W. Mol et al. Use of metformin to prolong gestation in preterm pre-eclampsia: randomised, double blind, placebo controlled trial. BMJ 374, 2103 (2021). https://doi.org/10.1136/bmj.n2103
S. Niromanesh, A. Alavi, F.R. Sharbaf, N. Amjadi, S. Moosavi, S. Akbari, Metformin compared with insulin in the management of gestational diabetes mellitus: A randomized clinical trial. Diabetes Res. Clin. Pract. 98, 422–9 (2012). https://doi.org/10.1016/j.diabres.2012.09.031
C.P. Spaulonci, L.S. Bernardes, T.C. Trindade, M. Zugaib, R.P.V. Francisco, Randomized trial of metformin vs insulin in the management of gestational diabetes. Am. J. Obstet. Gynecol. 209, 34.e1–34.e7 (2013). https://doi.org/10.1016/j.ajog.2013.03.022
Author contributions
S.A.P. conceived the idea of this review article. S.A.P., A.S., and E.G. selected the articles and extracted the data. S.A.P., A.S., E.G., and K.I.A. wrote the first draft of the manuscript. T.K., T.P., I.L., E.A., B.H.R.W., and D.G.G. critically revised the manuscript. All authors approved the final version of the article.
Funding
Open access funding provided by HEAL-Link Greece.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Paschou, S.A., Shalit, A., Gerontiti, E. et al. Efficacy and safety of metformin during pregnancy: an update. Endocrine 83, 259–269 (2024). https://doi.org/10.1007/s12020-023-03550-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-023-03550-0