Abstract
Background
Non-functioning pituitary macroadenomas (NFPAs) with visual field defects are ideally managed by transsphenoidal tumour resection to improve vision, and long-term postsurgical follow up is necessary to monitor for tumour recurrence. Regular updates from global data are necessary for developing optimal management strategies of these tumours.
Methods
Pre- and postoperative visual and endocrine profile, imaging characteristics and details of surgical interventions among patients with NFPAs managed between 2008 and 2019 in a UK regional centre were assessed. The radiological and surgical outcomes including postoperative complications, recurrence risk and the factors influencing outcomes also were assessed.
Results
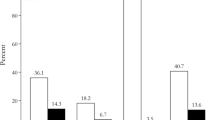
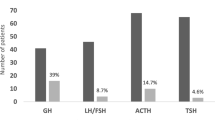
105 cases with mean (SD) age 60.1 (14.3) years and follow-up duration 60 (37) months were studied. 67 (64%) patients were male. Five-year recurrence-free survival rate was 71.5% (95% confidence interval [CI] 62.7% to 81.6%) with 33 (31%) tumour recurrences of whom 20 (60%) received radiotherapy and 9 (27%) underwent further surgery. Younger age, tumour volume, and bilateral cavernous sinus extension were the predictors of recurrence on univariate analysis, while younger age was the only factor on multivariate analysis (Hazard ratio 0.95; 95% CI: 0.92, 0.97). 72/78 patients (92%) with preoperative visual field defects improved after surgery, of whom 27 (35%) had full recovery. 20 (24%) patients had recovery of an abnormal hormone axis. 15 patients (16%) developed perioperative complications such as cerebrospinal fluid leak (12 cases), meningitis (2 cases), and bleeding (2 cases).
Conclusions
Five-year recurrence-free survival after transsphenoidal resection for NFPAs was 71.5% with older age at surgery conferring lower risk of recurrence. Visual recovery/ improvement occurred in 92% of cases with preoperative visual defects following surgery.


Similar content being viewed by others
References
H. Gittleman, Q.T. Ostrom, P.D. Farah, A. Ondracek, Y. Chen, Y. Wolinsky, C. Kruchko, J. Singer, V.R. Kshettry, E.R. Laws, A.E. Sloan, W.R. Selman, J.S. Barnholtz-Sloan, Descriptive epidemiology of pituitary tumors in the United States, 2004–2009. J. Neurosurg. 121, 527–535 (2014). https://doi.org/10.3171/2014.5.JNS131819
S. Ezzat, S.L. Asa, W.T. Couldwell, C.E. Barr, W.E. Dodge, M.L. Vance, I.E. McCutcheon, The prevalence of pituitary adenomas. Cancer 101(3), 613–619 (2004). https://doi.org/10.1002/cncr.20412
T.T. Agustsson, T. Baldvinsdottir, J.G. Jonasson, E. Olafsdottir, V. Steinthorsdottir, G. Sigurdsson, A.V. Thorsson, P.V. Carroll, M. Korbonits, R. Benediktsson, The epidemiology of pituitary adenomas in Iceland, 1955–2012: a nationwide population-based study. Eur. J. Endocrinol. 173(5), 655–664 (2015). https://doi.org/10.1530/EJE-15-0189
S. Melmed, Pituitary-tumor endocrinopathies. N. Engl. J. Med. 382(10), 937–950 (2020). https://doi.org/10.1056/NEJMra1810772
B.D. McDowell, R.B. Wallace, R.M. Carnahan, E.A. Chrischilles, C.F. Lynch, J.A. Schlechte, Demographic differences in incidence for pituitary adenoma. Pituitary 14(1), 23–30 (2011). https://doi.org/10.1007/s11102-010-0253-4
J.W. Lucas, M.E. Bodach, L.M. Tumialan, N.M. Oyesiku, C.G. Patil, Z. Litvack, M.K. Aghi, G. Zada, Congress of neurological surgeons systematic review and evidence-based guideline on primary management of patients with nonfunctioning pituitary adenomas. Neurosurgery 79(4), E533–E535 (2016). https://doi.org/10.1227/NEU.0000000000001389
O.M. Dekkers, A.M. Pereira, J.A. Romijn, Treatment and follow-up of clinically nonfunctioning pituitary macroadenomas. J. Clin. Endocrinol. Metab. 93(10), 3717–3726 (2008). https://doi.org/10.1210/jc.2008-0643
P. Mortini, M. Losa, R. Barzaghi, N. Boari, M. Giovanelli, Results of trans-sphenoidal surgery in a large series of patients with pituitary adenoma. Neurosurgery 56(6), 1222–1233 (2005). https://doi.org/10.1227/01.neu.0000159647.64275.9d
P. Chanson, G. Raverot, F. Castinetti, C. Cortet-Rudelli, F. Galland, S. Salenave, French Endocrinology Society non-functioning pituitary adenoma work-group. Management of clinically non-functioning pituitary adenoma. Ann. Endocrinol. (Paris). 76(3), 239–247 (2015). https://doi.org/10.1016/j.ando.2015.04.002
M.E. Molitch, Diagnosis and treatment of pituitary adenomas: a review. JAMA 317(5), 516–524 (2017). https://doi.org/10.1001/jama.2016.19699
A.S. Little, P.A. Gardner, J.C. Fernandez-Miranda, M.R. Chicoine, G. Barkhoudarian, D.M. Prevedello, K.C.J. Yuen, D.F. Kelly, TRANSSPHER study group. pituitary gland recovery following fully endoscopic transsphenoidal surgery for nonfunctioning pituitary adenoma: results of a prospective multicenter study. J. Neurosurg. 15, 1–7 (2019). https://doi.org/10.3171/2019.8.JNS191012. NovOnline ahead of print
M. Harary, A.C. DiRisio, H.Y. Dawood, J. Kim, N. Lamba, C.H. Cho, T.R. Smith, H.A. Zaidi, E.R. Laws, Endocrine function and gland volume after endoscopic transsphenoidal surgery for nonfunctional pituitary macroadenomas. J. Neurosurg. 1, 1–10 (2018). https://doi.org/10.3171/2018.5.JNS181054. NovOnline ahead of print
A. Najmaldin, M. Malek, N.H. Madani, M. Ghorbani, H. Akbari, A. Khajavi, O.A. Qadikolaei, M.E. Khamseh, Non-functioning pituitary macroadenoma: surgical outcomes, tumor regrowth, and alterations in pituitary function-3-year experience from the iranian pituitary tumor registry. Hormones (Athens). 18(2), 197–205 (2019). https://doi.org/10.1007/s42000-019-00109-5
J.H. Kim, Y.S. Dho, Y.H. Kim, J.H. Lee, J.H. Lee, A.R. Hong, C.S. Shin, Developing an optimal follow-up strategy based on the natural history of nonfunctioning pituitary adenomas. J. Neurosurg. 131(2), 500–506 (2018). https://doi.org/10.3171/2018.4.JNS172148
M.J. Levy, I.J. Robertson, N. Khalk, S. Vitello, N. Reddy, R. Bhake, T.A. Howlett, Long-term follow-up of a large prospective cohort of patients with nonfunctioning pituitary adenomas: the outcome of a conservative management policy. Clin. Endocrinol. (Oxf.). 89(3), 354–359 (2018). https://doi.org/10.1111/cen.13791
N.J. Gittoes, A.S. Bates, W. Tse, B. Bullivant, M.C. Sheppard, R.N. Clayton, P.M. Stewart, Radiotherapy for non-function pituitary tumours. Clin. Endocrinol. (Oxf.). 48(3), 331–337 (1998). https://doi.org/10.1046/j.1365-2265.1998.00393.x
Y. Chen, C.D. Wang, Z.P. Su, Y.X. Chen, L. Cai, Q.C. Zhuge, Z.B. Wu, Natural history of postoperative nonfunctioning pituitary adenomas: a systematic review and meta-analysis. Neuroendocrinology 96(4), 333–342 (2012). https://doi.org/10.1159/000339823
E.P. O’Sullivan, C. Woods, N. Glynn, L.A. Behan, R. Crowley, P. O’Kelly, D. Smith, C.J. Thompson, A. Agha, The natural history of surgically treated but radiotherapy-naïve nonfunctioning pituitary adenomas. Clin. Endocrinol. (Oxf.). 71(5), 709–714 (2009). https://doi.org/10.1111/j.1365-2265.2009.03583.x
J.P. Almeida, R. Tabasinejad, A. Kalyvas, H. Takami, N. Mohan, P.J. O’Halloran, M.M. Sanchez, C. Velasquez, G. Zadeh, F. Gentili, The importance of long term follow up after endoscopic pituitary surgery: durability of results and tumor recurrence. Neurol. India 68, S92–S100 (2020). https://doi.org/10.4103/0028-3886.287675
A.F. Haddad, J.S. Young, T. OH, M.P. Pereira, R.S. Joshi, K.M. Pereira, R.C. Osorio, K.C. Donohue, Z. Peeran, S. Sudhir, S. Jain, A. Beniwal, A.S. Chopra, N.S. Sandhu, P.V. Theodosopoulos, S. Kunwar, I.H. El-Sayed, J. Gurrola, L.S. Blevins, M.K. Aghi, Clinical characteristics and outcomes of null-cell versus silent gonadotroph adenomas in a series of 1166 pituitary adenomas from a single institution. Neurosurg. Focus. 48(6), E13 (2020). https://doi.org/10.3171/2020.3.FOCUS20114
M.M. Gerges, K. Rumalla, S.S. Godil, I. Younus, W. Elshamy, G.A. Dobri, A. Kacker, A. Tabaee, V.K. Anand, T.H. Schwartz, Long-term outcomes after endoscopic endonasal surgery for nonfunctioning pituitary macroadenomas. J. Neurosurg. 2020;1–12. https://doi.org/10.3171/2019.11.JNS192457
A.L. Pappy II., A. Savinkina, C. Bicknese, S. Neill, N.M. Oyesiku, A.G. Ioachimescu, Predictive modeling for pituitary adenomas: single center experience in 501 consecutive patients. Pituitary 22(5), 520–531 (2019). https://doi.org/10.1007/s11102-019-00982-8
R.L. Batista, E.B. Trarbach, M.D. Marques, V.A. Cescato, G.O. da Silva, C.G.B. Herkenhoff, M.B. Cunha-Neto, N.R. Musolino, Nonfunctioning pituitary adenoma recurrence and its relationship with sex, size, and hormonal immunohistochemical profile. World Neurosurg. 120, e241–e246 (2018). https://doi.org/10.1016/j.wneu.2018.08.043
R. Reddy, S. Cudlip, J.V. Byrne, N. Karavitaki, J.A. Wass, Can we ever stop imaging in surgically treated and radiotherapy-naive patients with non-functioning pituitary adenoma? Eur. J. Endocrinol. 165(5), 739–744 (2011). https://doi.org/10.1530/EJE-11-0566
J. Lelotte, A. Mourin, E. Fomekong, A. Michotte, C. Raftopoulos, D. Maiter, Both invasiveness and proliferation criteria predict recurrence of non-functioning pituitary macroadenomas after surgery: a retrospective analysis of a monocentric cohort of 120 patients. Eur. J. Endocrinol. 178(3), 237–246 (2018). https://doi.org/10.1530/EJE-17-0965
A.K. Watts, A. Easwaran, P. McNeill, Y.Y. Wang, W.J. Inder, C. Caputo, Younger age is a risk factor for regrowth and recurrence of nonfunctioning pituitary macroadenomas: Results from a single Australian centre. Clin. Endocrinol. (Oxf.). 87(3), 264–271 (2017). https://doi.org/10.1111/cen.13365
F. Langlois, D.S.T. Lim, E. Varlamov, C.G. Yedinak, J.S. Cetas, S. McCartney, A. Dogan A, M. Fleseriu, Clinical profile of silent growth hormone pituitary adenomas; higher recurrence rate compared to silent gonadotroph pituitary tumors, a large single center experience. Endocrine 58(3), 528–534 (2017). https://doi.org/10.1007/s12020-017-1447-6
T. Ogiwara, A. Nagm, T. Nakamura, T. Mbadugha, T. Horiuchi, K. Hongo, Significance and Indications of Surgery for Asymptomatic Nonfunctioning Pituitary Adenomas. World Neurosurg. 128, e752–e759 (2019). https://doi.org/10.1016/j.wneu.2019.04.250
I.C.M. Pelsma, M.J.T. Verstegen, F. de Vries, I.C. Notting, M.L.D. Broekman, W.R. van Furth, N.R. Biermasz, A.M. Pereira, Quality of care evaluation in non-functioning pituitary adenoma with chiasm compression: visual outcomes and timing of intervention clinical recommendations based on a systematic literature review and cohort study. Pituitary. 2020;23(4):417–429. https://doi.org/10.1007/s11102-020-01061-z
M. Araujo-Castro, E. Pascual-Corrales, A. Acitores Cancela, S. García Duque, L. Ley Urzaiz, V.Rodríguez Berrocal, Status and clinical and radiological predictive factors of presurgical anterior pituitary function in pituitary adenomas. Study of 232 patients. Endocrine 70(3), 584–592 (2020). https://doi.org/10.1007/s12020-020-02455-6
A. Jahangiri, J.R. Wagner, S.W. Han, M.T. Tran, L.M. Miller, R. Chen, M.W. Tom, L.R. Ostling, S. Kunwar, L. Blevins, M.K. Aghi, Improved versus worsened endocrine function after transsphenoidal surgery for nonfunctional pituitary adenomas: rate, time course, and radiological analysis. J. Neurosurg. 124(3), 589–595 (2016). https://doi.org/10.3171/2015.1.JNS141543
N. Fatemi, J.R. Dusick, C. Mattozo, D.L. McArthur, P. Cohan, J. Boscardin, C. Wang, R.S. Swerdloff, D.F. Kelly, Pituitary hormonal loss and recovery after transsphenoidal adenoma removal. Neurosurgery 63(4), 709–718 (2008). https://doi.org/10.1227/01.NEU.0000325725.77132.90
E. Magro, T. Graillon, J. Lassave, F. Castinetti, S. Boissonneau, E. Tabouret, S. Fuentes, L. Velly, R. Gras, H. Dufour, Complications related to the endoscopic endonasal transsphenoidal approach for nonfunctioning pituitary macroadenomas in 300 consecutive patients. World Neurosurg. 89, 442–453 (2016). https://doi.org/10.1016/j.wneu.2016.02.059
P. Riesgo, P. Mariño, A. Platero, F.J. Tarazona, C. Fajardo, J.L. Llácer, V. Rovira, R. Rodríguez, A. Flor-Goikoetxea, J. Piquer, Postoperative CSF leakages after transsphenoidal surgery for pituitary adenomas: analysis of a series of 302 surgical procedures. Fístulas posquirúrgicas de líquido cefalorraquídeo tras cirugía transesfenoidal de adenomas hipofisarios: análisis de una serie de 302 intervenciones. Neurocirugia (Astur.). 30(5), 215–221 (2019). https://doi.org/10.1016/j.neucir.2019.03.003
S.M. Graham, T.A. Iseli, L.H. Karnell, J.D. Clinger, P.W. Hitchon, J.D. Greenlee, Endoscopic approach for pituitary surgery improves rhinologic outcomes. Ann. Otol. Rhinol. Laryngol. 118(9), 630–635 (2009). https://doi.org/10.1177/000348940911800905
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Subramanian, V., Lee, R.S.M., Howell, S. et al. Non-functioning pituitary macroadenomas: factors affecting postoperative recurrence, and pre- and post-surgical endocrine and visual function. Endocrine 73, 407–415 (2021). https://doi.org/10.1007/s12020-021-02713-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-021-02713-1