Abstract
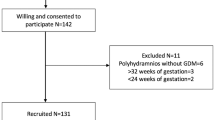
The purpose of this study is to investigate postprandial 1-h (PP1) and 2-h (PP2) blood glucose measurements’ correlation with adverse perinatal outcomes. This prospective cohort study consisted of 259 women with gestational diabetes mellitus. During each antenatal visit, HbA1c and fasting plasma glucose (FPG) as well as plasma glucose at PP1 and PP2 were analyzed. There were 144 patients on insulin therapy and 115 patients on diet therapy. A total of 531 blood glucose measurements were obtained at different gestational ages between 24 and 41 gestational weeks. PP2 plasma glucose measurements (but not PP1) were positively correlated with fetal macrosomia. But on adjusted analysis, neither PP1 nor PP2 measurements predicted perinatal complications. In addition to PP1 and PP2, neither FPG nor HbA1c were able to predict perinatal complications or fetal macrosomia when controlled for confounding factors except for a positive correlation between fetal macrosomia and HbA1c in patients on diet therapy. Postprandial 1-h and postprandial 2-h plasma glucose measurements were not superior to each other in predicting fetal macrosomia or perinatal complications. Based on our findings, it can be concluded that both methods may be suitable for follow-up as there are no clear advantages of one measurement over the other.

Similar content being viewed by others
References
Group H.S.C.R, B.E. Metzger, L.P. Lowe, A.R. Dyer, E.R. Trimble, U. Chaovarindr, D.R. Coustan, D.R. Hadden, D.R. McCance, M. Hod, H.D. McIntyre, J.J. Oats, B. Persson, M.S. Rogers, D.A. Sacks, Hyperglycemia and adverse pregnancy outcomes. N. Engl. J. Med. 358(19), 1991–2002 (2008). doi:10.1056/NEJMoa0707943
P.M. Catalano, H.D. McIntyre, J.K. Cruickshank, D.R. McCance, A.R. Dyer, B.E. Metzger, L.P. Lowe, E.R. Trimble, D.R. Coustan, D.R. Hadden, B. Persson, M. Hod, J.J. Oats, Group H.S.C.R, The hyperglycemia and adverse pregnancy outcome study: associations of GDM and obesity with pregnancy outcomes. Diabetes Care 35(4), 780–786 (2012). doi:10.2337/dc11-1790
C. Yogev, C. Hod, M. Oats, L. Metzger, D. Dyer, M. Trimble, P. Hadden, Rogers, Hyperglycemia Adverse Pregnancy Outcome Study Cooperative Research G, Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study: preeclampsia. Am. J. Obstet. Gynecol. 255(3), e251–e257 (2010). doi:10.1016/j.ajog.2010.01.024
M.V. Rudge, I.M. Calderon, M.D. Ramos, J.F. Abbade, L.M. Rugolo, Perinatal outcome of pregnancies complicated by diabetes and by maternal daily hyperglycemia not related to diabetes. A retrospective 10-year analysis. Gynecol. Obstet. Invest. 50(2), 108–112 (2000)
M. Farren, N. Daly, A.C. O’Higgins, A. McKeating, P.J. Maguire, M.J. Turner, The interplay between maternal obesity and gestational diabetes mellitus. J. Perinat. Med. (2014). doi:10.1515/jpm-2014-0272
G. Bayhan, M. Bahceci, A. Yalinkaya, M. Yayla, A.C. Erden, Diabetes mellitus in pregnancy and perinatal outcome. Gynecol. Obstet. Reprod. Med. 6(2), 99–103 (2000)
J. Pedersen, Weight and length at birth of infants of diabetic mothers. Acta Endocrinol. 16(4), 330–342 (1954)
Committee on Practice B-O, Practice Bulletin No. 137: gestational diabetes mellitus. Obstet. Gynecol. 122(2 Pt 1), 406–416 (2013). doi:10.1097/01.AOG.0000433006.09219.f1
R.G. Moses, E.M. Lucas, S. Knights, Gestational diabetes mellitus. At what time should the postprandial glucose level be monitored? Aust. N. Z. J. Obstet. Gynaecol. 39(4), 457–460 (1999)
B. Weisz, A. Shrim, C.J. Homko, E. Schiff, G.S. Epstein, E. Sivan, One hour versus two hours postprandial glucose measurement in gestational diabetes: a prospective study. J. Perinatol. 25(4), 241–244 (2005). doi:10.1038/sj.jp.7211243
E. Sivan, B. Weisz, C.J. Homko, E.A. Reece, E. Schiff, One or two hours postprandial glucose measurements: are they the same? Am. J. Obstet. Gynecol. 185(3), 604–607 (2001). doi:10.1067/mob.2001.117184
M. de Veciana, C.A. Major, M.A. Morgan, T. Asrat, J.S. Toohey, J.M. Lien, A.T. Evans, Postprandial versus preprandial blood glucose monitoring in women with gestational diabetes mellitus requiring insulin therapy. N. Engl. J. Med. 333(19), 1237–1241 (1995). doi:10.1056/NEJM199511093331901
C.P. Durnwald, L. Mele, C.Y. Spong, S.M. Ramin, M.W. Varner, D.J. Rouse, A. Sciscione, P. Catalano, G. Saade, Y. Sorokin, J.E. Tolosa, B. Casey, G.D. Anderson, Eunice Kennedy Shriver National Institute of Child H, Human Development Maternal-Fetal Medicine Units N, Glycemic characteristics and neonatal outcomes of women treated for mild gestational diabetes. Obstet. Gynecol. 117(4), 819–827 (2011). doi:10.1097/AOG.0b013e31820fc6cf
M.I. Yeral, A.S. Ozgu-Erdinc, D. Uygur, K.D. Seckin, M.F. Karsli, A.N. Danisman, Prediction of gestational diabetes mellitus in the first trimester, comparison of fasting plasma glucose, two-step and one-step methods: a prospective randomized controlled trial. Endocrine (2013). doi:10.1007/s12020-013-0111-z
C. Erem, N. Cihanyurdu, O. Deger, C. Karahan, G. Can, M. Telatar, Screening for gestational diabetes mellitus in northeastern Turkey (Trabzon City). Eur. J. Epidemiol. 18(1), 39–43 (2003)
World Medical A, World Medical Association declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 310(20), 2191–2194 (2013). doi:10.1001/jama.2013.281053
M.W. Carpenter, D.R. Coustan, Criteria for screening tests for gestational diabetes. Am. J. Obstet. Gynecol. 144(7), 768–773 (1982)
E. Li, D. Zhang, M. Davidian, Conditional estimation for generalized linear models when covariates are subject-specific parameters in a mixed model for longitudinal measurements. Biometrics 60(1), 1–7 (2004). doi:10.1111/j.0006-341X.2004.00170.x
M.H. Beall, C. Spong, J. McKay, M.G. Ross, Objective definition of shoulder dystocia: a prospective evaluation. Am. J. Obstet. Gynecol. 179(4), 934–937 (1998)
American College of O, Gynecologists, Task Force on Hypertension in P, Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet. Gynecol. 122(5), 1122–1131 (2013). doi:10.1097/01.AOG.0000437382.03963.88
F. Faul, E. Erdfelder, A.G. Lang, A. Buchner, G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 39(2), 175–191 (2007)
American Diabetes A, Standards of medical care in diabetes–2014. Diabetes Care 37(Suppl 1), S14–S80 (2014). doi:10.2337/dc14-S014
A. Ben-Haroush, Y. Yogev, R. Chen, B. Rosenn, M. Hod, O. Langer, The postprandial glucose profile in the diabetic pregnancy. Am. J. Obstet. Gynecol. 191(2), 576–581 (2004). doi:10.1016/j.ajog.2004.01.055
P. Dandona, H.S. Besterman, D.B. Freedman, F. Boag, A.M. Taylor, A.G. Beckett, Macrosomia despite well-controlled diabetic pregnancy. Lancet 1(8379), 737 (1984)
J.C. Hauth, R.G. Clifton, J.M. Roberts, L. Myatt, C.Y. Spong, K.J. Leveno, M.W. Varner, R.J. Wapner, J.M. Thorp Jr, B.M. Mercer, A.M. Peaceman, S.M. Ramin, M.W. Carpenter, P. Samuels, A. Sciscione, J.E. Tolosa, G. Saade, Y. Sorokin, G.D. Anderson, Eunice Kennedy Shriver National Institute of Child H, Human Development Maternal-Fetal Medicine Units N, Maternal insulin resistance and preeclampsia. Am. J. Obstet. Gynecol. 204(4), 327 (2011). doi:10.1016/j.ajog.2011.02.024. e321-326
M.S. Rendell, L. Jovanovic, Targeting postprandial hyperglycemia. Metab. Clin. Exp. 55(9), 1263–1281 (2006). doi:10.1016/j.metabol.2006.05.012
E. Lenters-Westra, R.K. Schindhelm, H.J. Bilo, R.J. Slingerland, Haemoglobin A1c: historical overview and current concepts. Diabetes Res. Clin. Pract. 99(2), 75–84 (2013). doi:10.1016/j.diabres.2012.10.007
S. Lurie, D. Danon, Life span of erythrocytes in late pregnancy. Obstet. Gynecol. 80(1), 123–126 (1992)
J.L. Mills, L. Jovanovic, R. Knopp, J. Aarons, M. Conley, E. Park, Y.J. Lee, L. Holmes, J.L. Simpson, B. Metzger, Physiological reduction in fasting plasma glucose concentration in the first trimester of normal pregnancy: the diabetes in early pregnancy study. Metab. Clin. Exp. 47(9), 1140–1144 (1998)
R.A. Gandhi, J. Brown, A. Simm, R.C. Page, I. Idris, HbA1c during pregnancy: its relationship to meal related glycaemia and neonatal birth weight in patients with diabetes. Eur. J. Obstet. Gynecol. Reprod. Biol. 138(1), 45–48 (2008). doi:10.1016/j.ejogrb.2007.08.011
G.K. Poomalar, Changing trends in management of gestational diabetes mellitus. World J Diabetes 6(2), 284–295 (2015). doi:10.4239/wjd.v6.i2.284
A. Garrison, Screening, diagnosis, and management of gestational diabetes mellitus. Am. Fam. Phys. 91(7), 460–467 (2015)
Acknowledgements
This paper is selected as a poster presentation in the 13th World Congress in Fetal Medicine, 29 June–3 July 2014 Nice, France.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Rights and permissions
About this article
Cite this article
Ozgu-Erdinc, A.S., Iskender, C., Uygur, D. et al. One-hour versus two-hour postprandial blood glucose measurement in women with gestational diabetes mellitus: which is more predictive?. Endocrine 52, 561–570 (2016). https://doi.org/10.1007/s12020-015-0813-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-015-0813-5