Abstract
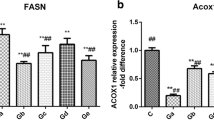
Copper (Cu) is a kind of widely used dietary supplement in poultry production, and a common environmental pollutant at the same time. Excess Cu exposure has been reported to accumulate in the liver and induce cytotoxicity, but the effect of Cu toxicity on hepatic cholesterol metabolism is still uncertain. Herein, we aimed to reveal the effect of excess Cu on the liver and primary hepatocytes of broilers at various concentrations. We found that 110 mg/kg Cu supplement remarkably increased blood cholesterol levels by detecting serum TC, LDL-C, and HDL-C in the broilers, while there was no significant difference in 220 and 330 mg/kg Cu supplements. In addition, high Cu exposure resulted in severe hepatic steatosis and hepatic cord derangement in the broilers. Oil red O staining of primary hepatocytes showed that Cu treatment caused intracellular neutral lipid accumulation. However, the hepatic TC content indicated a downward trend in both liver tissues and hepatocytes after Cu exposure. Furthermore, the expression of cholesterol metabolism-related indicators (SREBP2, HMGCR, LDLR, and CYP7A1) was notably decreased in the Cu-treated groups. While the expression of the key enzyme of cholesterol esterification (ACAT2) did not change significantly. Taken together, our findings preliminarily revealed excess Cu-induced hepatic cholesterol metabolism dysfunction, providing a deeper understanding of the molecular mechanisms of Cu-induced hepatotoxicity.
Graphical Abstract






Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Mandil R, Prakash A, Rahal A, Singh SP, Sharma D, Kumar R et al (2020) In vitro and in vivo effects of flubendiamide and copper on cyto-genotoxicity, oxidative stress and spleen histology of rats and its modulation by resveratrol, catechin, curcumin and α-tocopherol. BMC Pharmacol Toxicol 21(1):29. https://doi.org/10.1186/s40360-020-00405-6
Tisato F, Marzano C, Porchia M, Pellei M, Santini C (2010) Copper in diseases and treatments, and copper-based anticancer strategies. Med Res Rev 30(4):708–749. https://doi.org/10.1002/med.20174
Qu L, Huang H, Xia F, Liu Y, Dahlgren RA, Zhang M et al (2018) Risk analysis of heavy metal concentration in surface waters across the rural-urban interface of the Wen-Rui Tang River, China. Environ Pollut 237:639–649. https://doi.org/10.1016/j.envpol.2018.02.020
Kabala C, Galka B, Jezierski P (2020) Assessment and monitoring of soil and plant contamination with trace elements around Europe’s largest copper ore tailings impoundment. Sci Total Environ 738:139918. https://doi.org/10.1016/j.scitotenv.2020.139918
Zhang K, Su F, Liu X, Song Z, Feng X (2017) Heavy metal concentrations in water and soil along the Hun River, Liaoning China. Bull Environ Contam Toxicol 99(3):391–398. https://doi.org/10.1007/s00128-017-2142-2
Su F, Wang T, Zhang H, Song Z, Feng X, Zhang K (2018) The distribution and enrichment characteristics of copper in soil and Phragmites australis of Liao River estuary wetland. Environ Monit Assess 190(6):365. https://doi.org/10.1007/s10661-018-6746-8
Loland JØ, Singh BR (2004) Extractability and plant uptake of copper in contaminated coffee orchard soils as affected by different amendments. Acta Agric Scand, Sect B Soil Plant Sci 54(3):121–127. https://doi.org/10.1080/09064710410035640
Padrilah SN, Ahmad SA, Yasid NA, Sabullah MK, Daud HM, Khalid A et al (2017) Toxic effects of copper on liver and cholinesterase of Clarias gariepinus. Environ Sci Pollut Res Int 24(28):22510–22523. https://doi.org/10.1007/s11356-017-9923-3
Ameh T, Sayes CM (2019) The potential exposure and hazards of copper nanoparticles: A review. Environ Toxicol Pharmacol 71:103220. https://doi.org/10.1016/j.etap.2019.103220
Zischka H, Einer C (2018) Mitochondrial copper homeostasis and its derailment in Wilson disease. Int J Biochem Cell Biol 102:71–75. https://doi.org/10.1016/j.biocel.2018.07.001
Yang F, Cao H, Su R, Guo J, Li C, Pan J et al (2017) Liver mitochondrial dysfunction and electron transport chain defect induced by high dietary copper in broilers. Poult Sci 96(9):3298–3304. https://doi.org/10.3382/ps/pex137
Zubillaga M, Rosa D, Astiz M, Tricerri MA, Arnal N (2022) Effect of Sublethal Copper Overload on Cholesterol De Novo Synthesis in Undifferentiated Neuronal Cells. ACS Omega 7(29):25022–25030. https://doi.org/10.1021/acsomega.2c00703
Luo J, Yang H, Song BL (2020) Mechanisms and regulation of cholesterol homeostasis. Nat Rev Mol Cell Biol 21(4):225–245. https://doi.org/10.1038/s41580-019-0190-7
Li H, Yu X-H, Ou X, Ouyang X-P, Tang C-K (2021) Hepatic cholesterol transport and its role in non-alcoholic fatty liver disease and atherosclerosis. Prog Lipid Res 83:101109. https://doi.org/10.1016/j.plipres.2021.101109
Li H, Zhao L, Wang T, James Kang Y (2022) Dietary Cholesterol Supplements Disturb Copper Homeostasis in Multiple Organs in Rabbits: Aorta Copper Concentrations Negatively Correlate with the Severity of Atherosclerotic Lesions. Biol Trace Elem Res 200(1):164–171. https://doi.org/10.1007/s12011-021-02618-0
Kaya A, Altiner A, Ozpinar A (2006) Effect of copper deficiency on blood lipid profile and haematological parameters in broilers. J Vet Med A Physiol Pathol Clin Med 53(8):399–404. https://doi.org/10.1111/j.1439-0442.2006.00835.x
Allen KGD, Klevay LM (1978) Copper deficiency and cholesterol metabolism in the rat. Atherosclerosis 31(3):259–271. https://doi.org/10.1016/0021-9150(78)90062-X
Huster D, Purnat TD, Burkhead JL, Ralle M, Fiehn O, Stuckert F et al (2007) High Copper Selectively Alters Lipid Metabolism and Cell Cycle Machinery in the Mouse Model of Wilson Disease*. J Biol Chem 282(11):8343–8355. https://doi.org/10.1074/jbc.M607496200
El Sabry MI, Stino FKR, El-Ghany WAA (2021) Copper: benefits and risks for poultry, livestock, and fish production. Trop Anim Health Prod 53(5):487. https://doi.org/10.1007/s11250-021-02915-9
Fagnano M, Agrelli D, Pascale A, Adamo P, Fiorentino N, Rocco C et al (2020) Copper accumulation in agricultural soils: Risks for the food chain and soil microbial populations. Sci Total Environ 734:139434. https://doi.org/10.1016/j.scitotenv.2020.139434
Zhong G, L Li, Y Li, F Ma, J Liao, Y Li et al (2023) Cuproptosis is involved in copper-induced hepatotoxicity in chickens. Sci Total Environ 161458 https://doi.org/10.1016/j.scitotenv.2023.161458
Pesti GM, Bakalli RI (1996) Studies on the feeding of cupric sulfate pentahydrate and cupric citrate to broiler chickens. Poult Sci 75(9):1086–1091. https://doi.org/10.3382/ps.0751086
Nguyen HTT, Kheravii SK, Wu SB, Roberts JR, Swick RA, Toghyani M (2022) Sources and levels of copper affect liver copper profile, intestinal morphology and cecal microbiota population of broiler chickens fed wheat-soybean meal diets. Sci Rep 12(1):2249. https://doi.org/10.1038/s41598-022-06204-9
Ma F, Huo Y, Li H, Yang F, Liao J, Han Q et al (2022) New insights into the interaction between duodenal toxicity and microbiota disorder under copper exposure in chicken: Involving in endoplasmic reticulum stress and mitochondrial toxicity. Chemico-Biol Interact 366:110132. https://doi.org/10.1016/j.cbi.2022.110132
Huo Y, Ma F, Li T, Lei C, Liao J, Han Q et al (2023) Exposure to copper activates mitophagy and endoplasmic reticulum stress-mediated apoptosis in chicken (Gallus gallus) cerebrum. Environ Toxicol 38(2):392–402. https://doi.org/10.1002/tox.23701
Yang F, Liao J, Pei R, Yu W, Han Q, Li Y et al (2018) Autophagy attenuates copper-induced mitochondrial dysfunction by regulating oxidative stress in chicken hepatocytes. Chemosphere 204:36–43. https://doi.org/10.1016/j.chemosphere.2018.03.192
Lei C, Huo Y, Ma F, Liao J, Hu Z, Han Q et al (2023) Long-term copper exposure caused hepatocytes autophagy in broiler via miR-455–3p-OXSR1 axis. Chemico-Biol Interact 369:110256. https://doi.org/10.1016/j.cbi.2022.110256
Nguyen HTT, Morgan N, Roberts JR, Swick RA, Toghyani M (2020) Copper hydroxychloride is more efficacious than copper sulfate in improving broiler chicken’s growth performance, both at nutritional and growth-promoting levels. Poult Sci 99(12):6964–6973. https://doi.org/10.1016/j.psj.2020.09.053
da Cruz Ferreira Júnior H, da Silva DL, de Carvalho BR, de Oliveira HC, Cunha Lima Muniz J, Junior Alves W et al (2022) Broiler responses to copper levels and sources: growth, tissue mineral content, antioxidant status and mRNA expression of genes involved in lipid and protein metabolism. BMC Vet Res 18(1):223. https://doi.org/10.1186/s12917-022-03286-5
Yang F, Liao J, Yu W, Qiao N, Guo J, Han Q et al (2021) Exposure to copper induces mitochondria-mediated apoptosis by inhibiting mitophagy and the PINK1/parkin pathway in chicken (Gallus gallus) livers. J Hazard Mater 408:124888. https://doi.org/10.1016/j.jhazmat.2020.124888
Yang F, Liao J, Yu W, Pei R, Qiao N, Han Q et al (2020) Copper induces oxidative stress with triggered NF-κB pathway leading to inflammatory responses in immune organs of chicken. Ecotoxicol Environ Saf 200:110715. https://doi.org/10.1016/j.ecoenv.2020.110715
Konjufca VH, Pesti GM, Bakalli RI (1997) Modulation of cholesterol levels in broiler meat by dietary garlic and copper. Poult Sci 76(9):1264–1271. https://doi.org/10.1093/ps/76.9.1264
Pan YX, Zhuo MQ, Li DD, Xu YH, Wu K, Luo Z (2019) SREBP-1 and LXRα pathways mediated Cu-induced hepatic lipid metabolism in zebrafish Danio rerio. Chemosphere 215:370–379. https://doi.org/10.1016/j.chemosphere.2018.10.058
Chen QL, Luo Z, Liu X, Song YF, Liu CX, Zheng JL et al (2013) Effects of waterborne chronic copper exposure on hepatic lipid metabolism and metal-element composition in Synechogobius hasta. Arch Environ Contam Toxicol 64(2):301–315. https://doi.org/10.1007/s00244-012-9835-7
Madison BB (2016) Srebp2: A master regulator of sterol and fatty acid synthesis1. J Lipid Res 57(3):333–335. https://doi.org/10.1194/jlr.C066712
Xue L, Qi H, Zhang H, Ding L, Huang Q, Zhao D et al (2020) Targeting SREBP-2-Regulated Mevalonate Metabolism for Cancer Therapy. Front Oncol 10:1510. https://doi.org/10.3389/fonc.2020.01510
Yang Z, Lian W, Waiho K, Zhu L, Chen A, Cheng Y et al (2022) Effects of copper exposure on lipid metabolism and SREBP pathway in the Chinese mitten crab Eriocheir sinensis. Chemosphere 308:136556. https://doi.org/10.1016/j.chemosphere.2022.136556
Seo E, Kang H, Choi H, Choi W, Jun HS (2019) Reactive oxygen species-induced changes in glucose and lipid metabolism contribute to the accumulation of cholesterol in the liver during aging. Aging Cell 18(2):e12895. https://doi.org/10.1111/acel.12895
Cao X, Fang W, Li X, Wang X, Mai K, Ai Q (2022) Increased LDL receptor by SREBP2 or SREBP2-induced lncRNA LDLR-AS promotes triglyceride accumulation in fish. iScience 25(7):104670. https://doi.org/10.1016/j.isci.2022.104670
Yang Y-N, Wang Q-C, Xu W, Yu J, Zhang H, Wu C (2022) The berberine-enriched gut commensal Blautia producta ameliorates high-fat diet (HFD)-induced hyperlipidemia and stimulates liver LDLR expression. Biomed Pharmacother 155:113749. https://doi.org/10.1016/j.biopha.2022.113749
Rogers MA, Liu J, Song B-L, Li B-L, Chang CCY, Chang T-Y (2015) Acyl-CoA:cholesterol acyltransferases (ACATs/SOATs): Enzymes with multiple sterols as substrates and as activators. J Steroid Biochem Mol Biol 151:102–107. https://doi.org/10.1016/j.jsbmb.2014.09.008
Farooqui N, Elhence A, Shalimar, (2022) A Current Understanding of Bile Acids in Chronic Liver Disease. J Clin Exp Hepatol 12(1):155–173. https://doi.org/10.1016/j.jceh.2021.08.017
Erickson SK, Lear SR, Deane S, Dubrac S, Huling SL, Nguyen L et al (2003) Hypercholesterolemia and changes in lipid and bile acid metabolism in male and female cyp7A1-deficient mice. J Lipid Res 44(5):1001–1009. https://doi.org/10.1194/jlr.M200489-JLR200
Acknowledgements
This work was supported by grants from the National Natural Science Foundation of China (No. 32072930) and National Key R & D Program of China (No. 2016YFD0501205 and No. 2017YFD0502200).
Author information
Authors and Affiliations
Contributions
Yihui Huo: conceptualization, methodology, formal analysis, investigation, visualization, writing—original draft. Feiyang Ma: data curation, formal analysis, investigation, writing—review and editing. Lei Li: conceptualization, methodology. Yuanxu Li: data curation, formal analysis, investigation, writing—review and editing. Gaolong Zhong: investigation, writing—review and editing. Jianzhao Liao: data curation, formal analysis, investigation. Qingyue Han: methodology, formal analysis, investigation. Ying Li: writing—review and editing. Jiaqiang Pan: resources. Lianmei Hu: methodology. Hui Zhang: methodology, formal analysis. Jianying Guo: writing—review and editing. Zhaoxin Tang: conceptualization, methodology, supervision, project administration, funding acquisition.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yihui Huo and Feiyang Ma share the first authorship.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huo, Y., Ma, F., Li, L. et al. Effect of Copper Exposure on the Cholesterol Metabolism in Broiler Liver. Biol Trace Elem Res 201, 5747–5755 (2023). https://doi.org/10.1007/s12011-023-03609-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-023-03609-z