Abstract
Purpose of review
Heart failure (HF) hospitalizations are common, costly, associated with poor outcomes and potentially avoidable. Reducing HF hospitalizations is therefore a major objective of US healthcare. This review aims to outline causes for HF hospitalizations and provides actionable strategies for HF hospitalization prevention.
Recent findings
Heart failure hospitalizations often have multifactorial and diverse etiologies associated with medical and social patient factors leading to increased congestion. The most recently updated American Heart Association/American College of Cardiology/Heart Failure Society of America Guidelines for the Management of HF were published in 2022 and utilize high-quality evidence to offer a framework for analyzing and preventing HF hospitalizations.
Summary
Prevention of hospitalizations can be achieved by optimizing guideline-directed medical therapies, incorporating appropriate device-based technologies, and utilizing systems-based practices. By identifying treatment gaps and opportunities for improved HF care, this review comprehensively defines the challenges associated with HF rehospitalizations as well as potential solutions.
Similar content being viewed by others
Introduction
Heart failure (HF) is one of the most commonly diagnosed clinical conditions affecting approximately 60 million people around the globe [1]. Six million Americans are already living with HF and account for more than 1 million hospitalizations annually [2]. Of these, nearly 1 in 4 are rehospitalized within 30 days of discharge and almost half return to the hospital within 6 months [1, 3, 4•]. HF has a staggering associated economic impact with estimated costs of greater than $40 billion in the USA in the year 2020. Without intervention, this figure is expected to balloon to nearly $70 billion annually by 2030 [5].
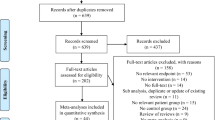
Hospital-based care accounts for the biggest share of direct HF medical costs and hospitalizations for HF are associated with worse clinical outcomes. Reduction in inpatient hospital stays is therefore a prime target for improving HF care in the USA [6, 7•]. Since up to a quarter of HF rehospitalizations are thought to be avoidable, additional strategies are needed to identify gaps in care that can prevent HF rehospitalizations [4•]. The enormous diversity of factors leading to a HF rehospitalization makes targeting preventable causes a difficult task. New tools and data aimed at preventing rehospitalizations may contribute to a changing landscape. For instance, the most recently updated American Heart Association (AHA)/American College of Cardiology (ACC)/Heart Failure Society of America (HFSA) Guidelines for the Management of HF were published in 2022, replacing the last iteration of the guidelines in 2013 and the focused update in 2017. These guidelines, based on high-quality evidence and contemporary studies, provide a framework for analyzing and preventing HF hospitalizations. The following review article will summarize contemporary published data and emphasize actionable strategies associated with pharmacologic interventions, device-based technologies, and systems-based practices to prevent HF rehospitalizations (Fig. 1).
Contextualizing Heart Failure Rehospitalizations in the US
As a result of the clinical and financial consequences associated with rehospitalizations for HF, improving this key metric has become a national priority [8]. The Centers for Medicare and Medicaid Services (CMS) began public reporting of hospital-level 30-day risk adjusted rehospitalization rates for HF in 2009. Three years later, CMS began the Hospital Readmissions Reduction Program (HRRP), which imposed financial penalties on hospitals with higher than expected 30-day readmissions for HF and other conditions [4•, 9]. The HRRP punishment-for-performance program was implemented across the country without necessary evidence-based tools to respond to higher-than-expected rehospitalization rates. Since that time there have been conflicting reports of the impact of these policy changes. For example, there is concern that the HRRP had unintended negative downstream impact such as increased post-discharge mortality, increased shuffling of patients from inpatient admissions to emergency rooms or observation stays, and increased financial penalties for hospitals serving a higher proportion of socioeconomically disadvantaged patients [4•, 9, 10]. Penalization for HF rehospitalizations therefore has the potential for negative impact not only on individual patients but also on caregivers, communities, and healthcare systems. The complexity of the HF rehospitalization problem highlights the need for strong evidence-base supporting strategies to prevent rehospitalizations in the vulnerable HF population.
Causes of Heart Failure Rehospitalizations
HF rehospitalizations have diverse, multifactorial etiologies related to both medical conditions and social factors [11]. Among the 17–35% of HF patients readmitted for true HF exacerbations, the primary pathophysiologic mechanism of decompensation leading to rehospitalization is congestion rather than a decrease in cardiac output [12]. Data suggests that the clinical milieu preceding hospitalization is often not truly acute but reflects a gradual increase of cardiac filling pressures. Identifiable precipitating factors that accelerate decompensation and lead to hospitalization include acute coronary syndromes, uncontrolled hypertension, arrhythmias, additional cardiac disease (e.g., endocarditis), infections, nonadherence with medications or dietary recommendations, anemia, thyroid disease, or ingestion of medications that cause sodium retention (e.g., NSAIDS) or negative inotropic effects (e.g., nondihydropyridine calcium channel blockers) [13••]. Prompt recognition of ischemia, arrhythmia, and other precipitating factors to inform the cause of a HF hospitalization is important for optimizing a patient’s clinical care while in the hospital and prevention of further events [13••]. While identifying precipitating factors is an important component of appropriate HF care, many hospitalizations do not have a clear etiology and simply represent ongoing progression of the underlying cardiomyopathy and/or the HF syndrome.
HF patients suffer from multimorbidity with > 85% of patients having 2 or more comorbid chronic conditions [13••]. Patients hospitalized for acute HF also have an increasing number of non-cardiovascular comorbidities over time and these are associated with worse outcomes [14]. It is not surprising that most HF readmissions are related to non-cardiovascular causes with up to 62% of readmissions due to other diagnoses. Among Medicare patients with HF, the 5 most common causes of readmissions accounting for > 50% of readmissions are HF, renal disorders, pneumonia, arrhythmias, and sepsis, with no other diagnoses accounting for more than 5% of readmissions [15]. Common comorbidities including anemia, hypertension, type 2 diabetes, coronary artery disease, atrial fibrillation, valvular heart disease, obstructive sleep apnea and cancer therapy-related cardiomyopathy play an important role in HF hospitalizations. Emphasis on comorbid disease management therefore plays an increasingly recognized role in both cause and control of hospitalizations[13••]. Patients with HF with preserved ejection fraction (HFpEF) in particular often have important comorbidities, particularly chronic kidney disease, that contribute indirectly to increased readmissions[16, 17]. Furthermore, older adults suffer disproportionately from HF and have additional risk factors for hospitalization related to polypharmacy for multiple concurrent diagnoses and challenges with self-care [18].
In addition to comorbidities and age, there are other patient-specific risk factors which also contribute to rehospitalizations. Socioeconomic factors such as mean neighborhood income and race are strongly associated with HF readmissions [11, 19]. Adverse social determinants of health including food and housing insecurity, low health literacy, lack of social support and financial barriers substantially contribute to poor HF outcomes. Such social factors act as barriers to obtaining optimal HF care by adding stress, competing with medical needs, channeling away time and financial resources, and reducing access to high-quality care [11, 20–22]. The 2022 ACC/AHA/HFSA HF Guidelines highlight the need for awareness of the biological factors, social determinants of health, and implicit biases that affect the risk factors, clinical care needs and outcomes of vulnerable populations [13••]. The impact of disparities on the HF readmissions metric is therefore being actively studied and cannot be underscored. To prevent unnecessary HF admissions and repeat hospitalizations, strategies for improvement must comprehensively address both the medical and socioeconomic factors that underlie these presentations.
Rehospitalization Prevention Strategies
Medications
Guideline-Directed Medical Therapy Classes
Medications have been well-established as a cornerstone for improving morbidity and mortality as well as preventing hospitalizations in patients with HF. As a result, there are 4 medication classes, termed “guideline-directed medical therapy” (GDMT), which have become the pillars of HF pharmacological therapy and include evidence-based beta-blockers, sodium-glucose cotransporter-2 inhibitors (SGLT2i), renin‐angiotensin system inhibitors, and mineralocorticoid receptor antagonists (MRA). Clinical treatment guidelines provide class I indications in support of the use of these medications, at targeted doses, based on HF severity [23]. Despite the robust survival benefits attributed to this set of medications, according to a recent editorial, “there is sobering evidence of inadequate implementation of life-saving GDMT in patients with HF” [24]. For example, in the Care Optimization Through Patient and Hospital Engagement Clinical Trial for Heart Failure (CONNECT- HF) trial which involved 161 US hospitals, renin–angiotensin–aldosterone system inhibitors and evidence-based β-blockers at 50% or more of their target doses were prescribed in less than 40% of eligible patients at hospital discharge or follow-up [25]. This widespread lack of proper GDMT use represents an opportunity for improvement with well-recognized potential positive outcomes.
Evidence-based beta-blockade works by blocking the cardiac β1-adrenergic receptor and preventing ventricular remodeling promoted by the stimulated renin–angiotensin–aldosterone system (RAAS) and sympathetic systems in patients with HF with reduced ejection fraction (HFrEF). As a result, beta-blockers (specifically bisoprolol, carvedilol, and sustained-release metoprolol succinate) have been proven to reduce morbidity and mortality in patients with symptomatic HFrEF and those with reduced left ventricular ejection fraction (LVEF) after myocardial infarction, unless contraindicated [26, 27]. The Initiation Management Predischarge: Process for Assessment of Carvedilol Therapy in Heart Failure (IMPACT-HF) trial showed that in-hospital initiation of beta-blockade in appropriate patients is not associated with worsening HF symptoms or other adverse outcomes. Pre-hospital discharge initiation of beta blockade is therefore a strategy which has been shown to be safe and effective at improving beta-blockade use at 60-days post discharge [27].
One of the more notable updates to the 2022 ACC/AHA/HFSA HF Guidelines includes recommendations involving SGLT2is. This medication class is now known specifically to prevent hospitalizations and reduce cardiovascular mortality in HF patients, regardless of LVEF. Though the SGLT2i mechanism of action works by lowering renal absorption of glucose, the beneficial effects on HF outcomes regardless of diabetes mellitus (DM) status have now been well-proven [28, 29]. SGLT2is therefore gained a class I recommendation in patients with symptomatic, chronic HFrEF irrespective of the presence of DM in the 2022 ACC/AHA/HFSA HF Guidelines [30]. The original evidence for these recommendations are drawn from the DAPA-HF and EMPEROR-Reduced trials which utilized different SGLT2i types (dapagliflozin and empagliflozin, respectively) however came to the same conclusion of 30% reduction in HF rehospitalizations [31, 32]. Particularly important is the addition of SGLT2is to the HFpEF armamentarium, since previously there were few interventions that had any proven clinical benefit in the HFpEF population. The EMPEROR-Preserved trial showed that SGLT is reduce first and recurrent HF hospitalizations as well as reduce decline in kidney function in HFpEF patients. They therefore now have a class IIa recommendation in this population [13••, 33]
More recent data supports the evidence for SGLT2i use in the acute HF hospitalization setting [28, 29]. For instance, the Effect of Sotagliflozin on Cardiovascular Events in Patients With Type 2 Diabetes Post Worsening Heart Failure (SOLOIST-WHF) trial showed that sotagliflozin (a nonspecific SGLTi) significantly reduced cardiovascular deaths and hospitalizations and urgent visits for HF in diabetics, compared to placebo [29]. Initiation of empagliflozin in-hospital for patients with acute HF also has been shown to have positive clinical impact. The Effects of Empagliflozin on Symptoms, Physical Limitations and Quality of Life in Patients Hospitalized for Acute Heart Failure (EMPULSE) trial showed that regardless of the degree of symptomatic impairment, in-hospital initiation of empagliflozin led to improved symptoms, physical limitations, and quality of life as soon as 15 days after initiation [28]. Further information regarding the safety and efficacy of in-hospital dapagliflozin initiation for patients with acute heart failure is forthcoming in the Dapagliflozin and Effect on Cardiovascular Events in Acute Heart Failure -Thrombolysis in Myocardial Infarction 68 (DAPA ACT HF-TIMI 68) trial [34].
An additional medication adjustment in the 2022 ACC/AHA/HFSA HF Guidelines update upgraded angiotensin-neprilysin inhibitors (ARNis) to the first-line recommendation among this class of RAAS regulatory medications for HFrEF patients, followed by angiotensin-inhibitor (ACEi) and then angiotensin receptor blockers (ARB) if ARNi not feasible. By blocking RAAS, these medications work by inhibiting the downstream effects of the angiotensin pathway which are deleterious in HF [26]. The ARNi sub-class earned this designation as a result of improved morbidity and mortality in ambulatory outpatients as shown in the landmark PARADIGM-HF trial [35]. ARNi has also been deemed appropriate for treatment-naïve hospitalized patients as a result of improvement of LV remodeling, health status and biomarkers as compared to ACEi/ARB [30, 36]. The Comparison of Sacubitril–Valsartan versus Enalapril on Effect on NT-proBNP in Patients Stabilized from an Acute Heart Failure Episode (PIONEER-HF) trial included stabilized inpatients with HFrEF who had been admitted for acute decompensated HF. The trial established the safety and efficacy of initiation of ARNI therapy during hospitalization for acute decompensated HF since it was associated with a reduction in the HF biomarker, NT-proBNP, and was generally well-tolerated [37]. Furthermore, studies have shown the potential applicability of this approach to the majority of US patients hospitalized for acute HF [38]. Increased emphasis of ARNI use and broader adoption of this medication represents one of several medication strategies that may influence HF outcomes.
MRAs have also shown consistent benefit across the spectrum of HFrEF etiologies and disease severities. When given in conjunction with ACE-inhibitors and beta-blockers, clinical trials proved that MRAs reduce the risk of morbidity and mortality in patients with EF ≤ 35%, though caution is advised in patients with renal dysfunction or hyperkalemia [26]. As a result, MRAs continue to be recommended in HFrEF patients with the New York Heart Association (NYHA) class II to IV symptoms provided patients have eGFR > 30 mL/min/1.73 m2 and serum potassium < 5.0 mEq [30].
Guideline-Directed Medical Therapy Implementation Strategies
The 2022 ACC/AHA/HFSA HF Guidelines present several novel strategies for GDMT prescribing. For instance, there is a new HF classification system based on left ventricular ejection fraction (LVEF) for patients with stage C (symptomatic) HF which helps define clinical trajectory and dictates pharmacologic management. The four classifications of HF now include (1) HF with reduced ejection fraction (HFrEF) for patients with LVEF ≤ 40%, (2) HF with improved ejection fraction (HFimpEF) includes patients with previous LVEF ≤ 40% and a follow-up measurement of LVEF > 40%, (3) HF with mildly reduced ejection fraction (HFmrEF) includes those with LVEF 41–49% and evidence of increased LV filling pressures, while (4) HFpEF includes individuals with LVEF ≥ 50% and evidence of increased LV filling pressures. This new schema has important implications for how these patients are treated [30]. There is now a class I indication that HFimpEF patients remain on GDMT to prevent relapse of left ventricular dysfunction and HF symptoms. The new acknowledgement of the HFmrEF category places emphasis on trajectory for these patients and presents an opportunity for clinicians to track progress and act accordingly. As such, diuretics as well as the medications in the GDMT arsenal may be appropriate for patients in this subgroup.
Though the impact of individual medications on improving HF morbidity and mortality cannot be understated, there is significant evidence that the way in which these medications are prescribed in clinical practice also impacts outcomes. Prior studies have shown that patients are most vulnerable to rehospitalization in the days and weeks immediately following a hospitalization [39, 40]. Patients hospitalized for HF often have medications discontinued during their hospitalization leading to higher risk of subsequent clinical events. Furthermore, delay of GDMT initiation to the outpatient setting leads to a greater than 75% chance that these medications will not be initiated within the next year [7•]. Such time delay represents a missed opportunity where patients are unable to benefit from the clinical effects of GDMT. The in-hospital initiation of GDMT among stable inpatients has therefore gained increasing traction. Though trials are ongoing regarding specific in-hospital initiation protocols, beta-blockers, SGLTis and ARNIs have adequate safety and tolerability profiles substantiating their use for appropriately selected inpatients with HF [7•, 37]. The early clinical benefits may contribute to their reduction in excess risk of rehospitalization following discharge [37].
Devices
Many attempts have been made at digital or device-based remote monitoring (RM) technologies to improve clinical outcomes in HF [41••]. Physical distancing and stay-at-home orders during the COVID-19 pandemic highlighted the need for RM strategies to provide early indications of HF decompensation and prevent HF admissions. Few devices already in use have established benefit for readmissions reductions. The most widely studied and successful RM technology used in clinical practice, the CardioMEMS, involves invasive hemodynamic monitoring through a pressure sensor percutaneously implanted in the pulmonary artery. CardioMEMS initially showed 28% reduction of rehospitalization rates due to pulmonary artery hemodynamic monitoring in the 2016 CHAMPION trial [42]. Subsequent analyses have continued to show clinical benefit, with average reduction in HF hospitalizations ranging from 37 to 62% [43]. Success of this strategy is attributed to real-time output and associated appropriate adjustment of medical therapy [41••].
Non-invasive devices utilized for RM of vital signs in HF patients have shown mixed results. Technology utilizing wearable sensors, web or phone-based digital platforms, multiparameter platforms, and machine learning are being actively investigated and have showed some promising preliminary data [41••, 44, 45]. Remote assessment of lung congestion has also been studied through both non-invasive means utilizing a wearable device as well as by taking advantage of thoracic sensors in pacemakers and implantable cardioverter defibrillators. Though there are encouraging preliminary results specifically for reduction in cardiovascular readmissions using remote dielectric sensing technology (ReDS), which utilizes electromagnetic signals transmitted through the thorax, more information is needed to recommend these strategies for widespread use to prevent readmissions [41••, 43, 45].
Systems-Based Strategies
In the USA, there is growing recognition of the value of addressing patient-centered precipitants of HF through teams- and systems-based strategies. These techniques seek to expand from the narrow focus on HF diagnosis and specific treatments to comprehensively address all aspects of patient care [46]. The impact of strategies including structured disease management programs, outpatient diuretics infusions, and electronic health records-based alerts is being actively studied and all have the potential to further improve systems of care for the HF population. Several recently established techniques include emphasis on social factors, patient self-care and timely referral for more advanced HF care.
HF rehospitalizations are intimately connected with the medical and social complexities associated with disparities in care and disadvantaged populations [10, 47]. As a result, increased emphasis is being placed on managing the social barriers to optimal care. A major teams-based strategy to address this issue involves comprehensively identifying and addressing social determinants of health [48]. Clinicians should have easy access to resources which recognize potential financial barriers to care, such as cheap pharmacy formulary lists and educational materials that include low-cost nutritional foods. Other simple systems-based strategies that promote recognition of possible social obstacles to HF care include ensuring patient availability to information in their own language and having established referral connections for specialty care including social work and mental health. To acknowledge the importance of equitable high-quality HF care, the 2022 ACC/AHA/HFSA HF Guidelines specifically identify a host of social barriers and potential management strategies ranging from homelessness to low health literacy to transportation limitations [24]. For the first time, the updated HF guidelines also incorporate previously published cost-effectiveness analyses into value statements for interventions. These value statements incorporate high-quality economic investigations and help further guide focus areas for care, particularly for patients with limited financial resources [30].
Another newer patient-centered strategy being utilized to combat HF readmissions is the recommendation to provide self-care support. Self-care involves patient engagement strategies which aid with detection, monitoring, and management of symptoms. Several educational and behavioral interventions have been studied which aid in this endeavor and have been shown to reduce unplanned readmissions [49]. Promotion of effective self-care involves utilizing adult education techniques to improve patient knowledge, promoting skill development including how to take medications as prescribed, and engaging patients such as through goal-setting [49]. Intimately involved with this strategy is the need to involve multidisciplinary teams to address potential self-care barriers, facilitate GDMT implementation and triage patient needs to prevent subsequent hospitalizations. The 2022 ACC/AHA/HFSA HF Guidelines suggest that multidisciplinary teams including cardiologists, primary care physicians, nurses, pharmacists, dieticians, mental health clinicians, and social workers all work together to promote patient treatment adherence through self-care. Furthermore, these teams are needed to identify and mitigate self-care barriers including cognitive dysfunction, social isolation, depression, and frailty [30, 49, 50]
Prior studies have shown that patients with more advanced HF and more frequent HF hospitalizations have higher readmissions rates [51]; therefore, an additional systems-based approach to improving HF outcomes involves timely referral for specialty HF care when appropriate. Ensuring that patients with higher comorbidity burden and more advanced HF have access to comprehensive HF-specific care is a key tenet to keeping these patients out of the hospital. These HF specialty teams can review HF management, determine candidacy for advanced HF therapies, evaluate patient goals of care, and engage palliative care teams when needed. Recognition of this strategy’s value has led to a nationwide push for early identification of advanced HF among all clinicians, not limited to cardiologists, and subsequent timely referral to specialty care [30, 52].
Treatment Gaps
Despite advances in the understanding of the multifactorial causes of HF hospitalizations, many challenges remain. Even basic tenets of HF care require additional investigation such as suggested dietary sodium recommendations [53] or how to incorporate widely used patient-reported outcomes into treatment frameworks [54]. As evidenced in the 2022 ACC/AHA/HFSA HF Guidelines, there are many promising medications and devices for all types of HF patients with proven clinical benefit. The remaining challenge centers on optimal implementation of these evidence-based therapies. Better understanding of how to use technologies or existing frameworks to streamline HF care is an additional area of investigation with significant therapeutic potential. For example, the CONNECT-HF study sought to evaluate the effects of a hospital and post-discharge quality improvement intervention on HF outcomes. This study highlighted the lack of practical interventions for improving GDMT prescribing which may be associated with stagnation in improvement in HF hospitalizations [25]. Similarly, the PROMPT-HF trial attempted to introduce tailored electronic health records alerts to improve HF medical management [55]. Though the medical science behind GDMT is well-established, the most effective way to prescribe GDMT to HF patients remains an ongoing challenge.
Future Directions
Due to the increased attention on HF rehospitalizations in the last decade, there is a rapid pace of innovation in HF. Entirely new medication classes as well as implementation strategies have been established. Devices aimed at improving RM or altering underlying HF physiology principles are being actively studied. Novel strategies to treat patients such as risk-prediction models or genetic profiling to tailor individualized therapy are all being developed. Though promising, these changes are all necessary principally because there is a lack of data on how to improve HF outcomes.
In our opinion, there are many challenges and opportunities for the HF community, and we believe future interventions should consider at least these four strategies to reduce rehospitalizations for HF care. First, HF care often requires assistance from caretakers such as family members. There are limited data on how to engage and activate caretakers in the care of HF patients, including during the vulnerable transition period from hospital to home. Second, with a growing emphasis on technology and devices for HF management, more work is necessary to understand how this may address or exacerbate disparities in care including for populations with low income, low education, or limited access to care due to obstacles such as rurality. Third, there is an appropriate emphasis on prescribing of new HF medications, including before hospital discharge. However, there are limited data understanding post-discharge barriers to medication use including prescription drug coverage and barriers to HF medication adherence. Finally, there is an emphasis on better understanding the transitional care period, but new tools and research are necessary to help patients and clinicians navigate the siloed nature of the current US healthcare system. There can be important differences in the communication and treatment plans between teams caring for patients in the hospital compared with the outpatient clinic and other clinicians including pharmacies.
Conclusion
We believe more work is necessary to comprehensively address both the medical and social issues that contribute to HF hospitalizations. Three broad categories that may be utilized to prevent HF hospitalizations include improved use of HF-specific medications, devices, and systems-based strategies. Though challenges remain, ongoing investigation seeks to identify strategies to optimize HF care in the USA which can prevent hospitalizations, improve quality of life and patient outcomes.
Reference and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Groenewegen A, Rutten FH, Mosterd A, Hoes AW. Epidemiology of heart failure. Eur J Heart Fail. vol. 22, no. 8, pp. 1342–1356, Aug. 2020. https://doi.org/10.1002/EJHF.1858.
Jackson SL, Tong X, King RJ, Loustalot F, Hong Y, Ritchey MD. National burden of heart failure events in the United States, 2006 to 2014. Circ Heart Fail. 2018;11(12): e004873. https://doi.org/10.1161/CIRCHEARTFAILURE.117.004873.
Roger VL. Epidemiology of heart failure. Circ Res. 2021;128:1421–34. https://doi.org/10.1161/CIRCRESAHA.121.318172.
• Khan MS, et al. Trends in 30- and 90-day readmission rates for heart failure. Circ Hear Fail. pp. 450–458, 2021. https://doi.org/10.1161/CIRCHEARTFAILURE.121.008335. This study investigates temporal trends of heart failure rehospitalizations extending out to 90-days post-hospitalization and contextualizes the impact of the hospital readmission reduction program on heart failure outcomes.
Urbich M, et al. A systematic review of medical costs associated with heart failure in the USA (2014–2020). PharmacoEconomics 2020 3811, vol. 38, no. 11, pp. 1219–1236, Aug. 2020. https://doi.org/10.1007/S40273-020-00952-0.
Patel J. Heart failure population health considerations. Am J Manag Care. vol. 27, pp. S191–S195, Jun. 2021. https://doi.org/10.37765/AJMC.2021.88673.
• Rao VN, et al. In-hospital initiation of sodium-glucose cotransporter-2 inhibitors for heart failure with reduced ejection fraction. J Am Coll Cardiol. 2021;78(20)2004 2012. https://doi.org/10.1016/J.JACC.2021.08.064. This article summarizes the rationale for in-hospital initation of guideline-directed medical therapy for patients with heart failure with reduced ejection fraction, specifically focusing on sodium-glucose cotransporter-2 inhibitors
Parizo JT, Kohsaka S, Sandhu AT, Patel J, Heidenreich PA. Trends in readmission and mortality rates following heart failure hospitalization in the veterans affairs health care system from 2007 to 2017. JAMA Cardiol. 2020;5(9):1042–7. https://doi.org/10.1001/JAMACARDIO.2020.2028.
Wadhera RK, Joynt Maddox KE, Wasfy JH, Haneuse S, Shen C, Yeh RW. Association of the hospital readmissions reduction program with mortality among medicare beneficiaries hospitalized for heart failure, acute myocardial infarction, and pneumonia. JAMA 2018;vol. 320, no. 24, pp. 2542–2552. https://doi.org/10.1001/JAMA.2018.19232.
Wadhera RK, et al. Performance in federal value-based programs of hospitals recognized by the American Heart Association and American College of Cardiology for High-Quality Heart Failure and Acute Myocardial Infarction Care. JAMA Cardiol. 2020;5(5):515–21. https://doi.org/10.1001/jamacardio.2020.0001.
Joynt Maddox KE, et al. Adjusting for social risk factors impacts performance and penalties in the hospital readmissions reduction program. Health Serv Res. 2019;vol. 54, no. 2, pp. 327–336. https://doi.org/10.1111/1475-6773.13133.
Ziaeian B, Fonarow GC. The prevention of hospital readmissions in heart failure ScienceDirect. 2015. https://doi.org/10.1016/j.pcad.2015.09.004.
•• Heidenreich PA, et al. AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022. https://doi.org/10.1161/CIR.0000000000001063. These clinical practice guidelines are the newest iteration of heart failure guidelines and utilize high-quality studies to summarize and dictate contemporary heart failure care.
Sharma A et al. Trends in noncardiovascular comorbidities among patients hospitalized for heart failure: insights from the get with the Guidelines-Heart Failure Registry. Circ Heart Fail. 2018;vol. 11, no. 6. https://doi.org/10.1161/CIRCHEARTFAILURE.117.004646.
Ziaeian B, Fonarow GC. The prevention of hospital readmissions in heart failure. Prog Cardiovasc Dis. 2016;58(4):379. https://doi.org/10.1016/J.PCAD.2015.09.004.
Jha A, et al. Outcomes, resource utilization and predictors of thirty day readmission in patients with heart failure with preserved ejection fraction (HFpEF): insights from the Nationwide Readmissions Database 2017. Eur Heart J. 2020;vol. 41, no. Supplement_2. https://doi.org/10.1093/EHJCI/EHAA946.0896.
Reddy YNV, Borlaug BA. Readmissions in heart failure: it’s more than just the medicine. Mayo Clin Proc. 2019;94(10):1919–21. https://doi.org/10.1016/J.MAYOCP.2019.08.015.
Wong Y, Chaudhry SI, Desai MM, Krumholz HM. Trends in comorbidity, disability, and polypharmacy in heart failure. Am J Med. 2011;124(2):136–43. https://doi.org/10.1016/J.AMJMED.2010.08.017.
Su A, Al'Aref SJ, Beecy AN, Min JK, Karas MG. Clinical and socioeconomic predictors of heart failure readmissions: a review of contemporary literature. Mayo Clin Proc. 2019;vol. 94, no. 7, pp. 1304–1320. https://doi.org/10.1016/j.mayocp.2019.01.017.
Hu J, Gonsahn MD, Nerenz DR. Socioeconomic status and readmissions: evidence from an urban teaching hospital. Health Aff (Millwood). 2014;33(5):778–85. https://doi.org/10.1377/HLTHAFF.2013.0816.
Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for medicare beneficiaries by race and site of care. JAMA - J Am Med Assoc. 2011. https://doi.org/10.1001/jama.2011.123.
Fabbri M, et al. Health literacy and outcomes in patients with heart failure: a prospective community study. Mayo Clin Proc. 2018;93(1):9–15. https://doi.org/10.1016/J.MAYOCP.2017.09.018.
Greene SJ, et al. Medical therapy for heart failure with reduced ejection fraction: the CHAMP-HF Registry. J Am Coll Cardiol. 2018;72(4):351–66. https://doi.org/10.1016/J.JACC.2018.04.070/SUPPL_FILE/MMC1.DOCX.
Kittleson MM, Angeles L. A clinician’s guide to the 2022 ACC/AHA/HFSA Guideline for the Management of Heart Failure. J Card Fail. 2022;vol. 0, no. 0. https://doi.org/10.1016/J.CARDFAIL.2022.03.346.
Devore AD, et al. Effect of a hospital and postdischarge quality improvement intervention on clinical outcomes and quality of care for patients with heart failure with reduced ejection fraction: the CONNECT-HF Randomized Clinical Trial. JAMA. 2021;326(4):314–23. https://doi.org/10.1001/JAMA.2021.8844.
Shah A, Gandhi D, Srivastava S, Shah KJ, Mansukhani R. Heart failure: a class review of pharmacotherapy. 2017.
Gattis WA, O’Connor CM, Gallup DS, Hasselblad V, Gheorghiade M. Predischarge initiation of carvedilol in patients hospitalized for decompensated heart failure: results of the initiation management predischarge: process for assessment of carvedilol therapy in heart failure (IMPACT-HF) trial. J Am Coll Cardiol. 2004;43(9):1534–41. https://doi.org/10.1016/J.JACC.2003.12.040.
Kosiborod MN, et al. Effects of empagliflozin on symptoms, physical limitations and quality of life in patients hospitalized for acute heart failure - results from the EMPULSE trial. Circulation. 2022. https://doi.org/10.1161/CIRCULATIONAHA.122.059725.
Bhatt L, et al. Sotagliflozin in patients with diabetes and recent worsening heart failure. N Engl J Med. 2021;384(2):117–28. https://doi.org/10.1056/NEJMOA2030183/SUPPL_FILE/NEJMOA2030183_DATA-SHARING.PDF.
Heidenreich PA, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;vol. 79, no. 17, pp. e263–e421. https://doi.org/10.1016/J.JACC.2021.12.012.
McMurray JJV, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381(21):1995–2008. https://doi.org/10.1056/NEJMOA1911303.
Packer M, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med. 2020;383(15):1413–24. https://doi.org/10.1056/NEJMOA2022190.
Anker SD, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. 2021;385(16):1451–61. https://doi.org/10.1056/NEJMOA2107038/SUPPL_FILE/NEJMOA2107038_DATA-SHARING.PDF.
“Dapagliflozin and Effect on cardiovascular events in acute heart failure -thrombolysis in myocardial infarction 68 (DAPA ACT HF-TIMI 68).” [Online]. Available: https://clinicaltrials.gov/ct2/show/NCT04363697.
McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, Rouleau JL, Shi VC, Solomon SD, Swedberg K, Zile MR. Angiotensin–neprilysin inhibition versus enalapril in heart failure. Mass Med Soc. 2014.
Desai AS, et al. Effect of sacubitril-valsartan vs enalapril on aortic stiffness in patients with heart failure and reduced ejection fraction: a randomized clinical trial. jamanetwork.com. 2019. https://doi.org/10.1001/jama.2019.12843.
Velazquez J, et al. Angiotensin-neprilysin inhibition in acute decompensated heart failure. N Engl J Med. 2019;380(6):539–48. https://doi.org/10.1056/NEJMOA1812851.
Fudim M, et al. Representativeness of the PIONEER-HF Clinical Trial Population in Patients Hospitalized With Heart Failure and Reduced Ejection Fraction. Circ Heart Fail. 2020;vol. 13, no. 4. https://doi.org/10.1161/CIRCHEARTFAILURE.119.006645.
Lam SP, et al. Clinical outcomes and response to vericiguat according to index heart failure event: insights from the VICTORIA Trial. JAMA Cardiol. 2021;6(6):706–12. https://doi.org/10.1001/JAMACARDIO.2020.6455.
Butler J, et al. Clinical course of patients with worsening heart failure with reduced ejection fraction. J Am Coll Cardiol. 2019;73(8):935–44. https://doi.org/10.1016/J.JACC.2018.11.049.
•• Mohebali D, Kittleson MM. Remote monitoring in heart failure: current and emerging technologies in the context of the pandemic. Heart. 2021;vol. 107, no. 5, pp. 366–372. https://doi.org/10.1136/HEARTJNL-2020-318062. This review summarizes the evidence on current remote monitoring technologies in heart failure patients and highlights how these advances may benefit patients, particularly as remote-monitoring becomes more important.
Abraham WT, Stevenson LW, Bourge RC, Lindenfeld JA, Bauman JG, Adamson PB. Sustained efficacy of pulmonary artery pressure to guide adjustment of chronic heart failure therapy: complete follow-up results from the CHAMPION randomised trial. 2016;vol. 387, p. 453. https://doi.org/10.1016/S0140-6736(15)00723-0.
Abraham WT, et al. Patient monitoring across the spectrum of heart failure disease management 10 years after the CHAMPION trial. ESC Hear Fail. 2021;8(5):3472–82. https://doi.org/10.1002/EHF2.13550.
Stehlik J, et al. Continuous wearable monitoring analytics predict heart failure hospitalization: the link-hf multicenter study. Circ Hear Fail. 2020. https://doi.org/10.1161/CIRCHEARTFAILURE.119.006513.
Faragli A et al. The role of non-invasive devices for the telemonitoring of heart failure patients. Hear Fail Rev. 2020;265, vol. 26, no. 5, pp. 1063–1080. https://doi.org/10.1007/S10741-020-09963-7.
Hollenberg SM, et al. 2019 ACC expert consensus decision pathway on risk assessment, management, and clinical trajectory of patients hospitalized with heart failure: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2019;74(15):1966–2011. https://doi.org/10.1016/J.JACC.2019.08.001.
Durstenfeld MS, Ogedegbe O, Katz SD, Park H, Blecker S. Racial and ethnic differences in heart failure readmissions and mortality in a large municipal healthcare system. JACC Hear Fail. 2016;4(11):885–93. https://doi.org/10.1016/J.JCHF.2016.05.008.
Havranek P, et al. Social determinants of risk and outcomes for cardiovascular disease. Circulation. 2015;132(9):873–98. https://doi.org/10.1161/CIR.0000000000000228.
Toukhsati SR, Jaarsma T, Babu AS, Driscoll A, Hare DL. Self-care interventions that reduce hospital readmissions in patients with heart failure; towards the identification of change agents. Clin Med Insights Cardiol. 2019;vol. 13. https://doi.org/10.1177/1179546819856855.
Kundi H, et al. Association of frailty with 30-day outcomes for acute myocardial infarction, heart failure, and pneumonia among elderly adults. JAMA Cardiol. 2019;4(11):1084–91. https://doi.org/10.1001/JAMACARDIO.2019.3511.
Samsky MD, et al. Trends in readmissions and length of stay for patients hospitalized with heart failure in Canada and the United States. JAMA Cardiol. 2019;4(5):444–53. https://doi.org/10.1001/JAMACARDIO.2019.0766.
Maddox TM, et al. 2021 Update to the 2017 ACC Expert Consensus Decision Pathway for Optimization of Heart Failure Treatment: answers to 10 Pivotal Issues About Heart Failure With Reduced Ejection Fraction: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2021;77(6):772–810. https://doi.org/10.1016/J.JACC.2020.11.022/SUPPL_FILE/MMC3.PDF.
Ezekowitz JA, et al. Reduction of dietary sodium to less than 100 mmol in heart failure (SODIUM-HF): an international, open-label, randomised, controlled trial. Lancet. 2022;399(10333):1391–400. https://doi.org/10.1016/S0140-.
Pokharel Y, et al. Association of Serial Kansas City Cardiomyopathy Questionnaire Assessments With Death and Hospitalization in Patients With Heart Failure With Preserved and Reduced Ejection Fraction: a secondary analysis of 2 randomized clinical trials. JAMA Cardiol. 2017;2(12):1315–21. https://doi.org/10.1001/JAMACARDIO.2017.3983.
Lama Ghazi MP, et al. Electronic alerts to improve heart failure therapy in outpatient practice: a cluster randomized trial. J Am Coll Cardiol. 2022. https://doi.org/10.1016/J.JACC.2022.03.338.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Jamie Diamond has nothing to disclose. Adam DeVore reports research funding through his institution from the American Heart Association, Biofourmis, Bodyport, Cytokinetics, American Regent, Inc, the NHLBI, Novartis, and Story Health. He also provides consulting services for and/or receives honoraria from Abiomed, AstraZeneca, Cardionomic, InnaMed, LivaNova, Natera, Novartis, Procyrion, Story Health, Vifor, and Zoll. He has also received non-financial support from Abbott for educational and research activities.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Heart Failure
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Diamond, J., DeVore, A.D. New Strategies to Prevent Rehospitalizations for Heart Failure. Curr Treat Options Cardio Med 24, 199–212 (2022). https://doi.org/10.1007/s11936-022-00969-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11936-022-00969-y