Abstract
Purpose of Review
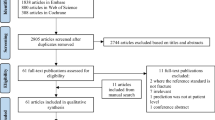
We re-evaluated clinical applications of image-to-FE models to understand if clinical advantages are already evident, which proposals are promising, and which questions are still open.
Recent Findings
CT-to-FE is useful in longitudinal treatment evaluation and groups discrimination. In metastatic lesions, CT-to-FE strength alone accurately predicts impending femoral fractures. In osteoporosis, strength from CT-to-FE or DXA-to-FE predicts incident fractures similarly to DXA-aBMD. Coupling loads and strength (possibly in dynamic models) may improve prediction. One promising MRI-to-FE workflow may now be tested on clinical data. Evidence of artificial intelligence usefulness is appearing.
Summary
CT-to-FE is already clinical in opportunistic CT screening for osteoporosis, and risk of metastasis-related impending fractures. Short-term keys to improve image-to-FE in osteoporosis may be coupling FE with fall risk estimates, pool FE results with other parameters through robust artificial intelligence approaches, and increase reproducibility and cross-validation of models. Modeling bone modifications over time and bone fracture mechanics are still open issues.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Leslie WD, Morin SN. New developments in fracture risk assessment for current osteoporosis reports. Curr Osteoporos Rep. 2020;18:115–29. Reviews non FE-specific specific risk factors used to assess fracture risk. Motivates further reviewing for FE-specific risk factors
Keaveny TM, Clarke BL, Cosman F, Orwoll ES, Siris ES, Khosla S, Bouxsein ML. Biomechanical Computed Tomography analysis (BCT) for clinical assessment of osteoporosis. Osteoporos Int. 2020;31:1025–48. Reviews applications of BCT, the most clinically used and FDA-approved CT-to-FE workflow, having opportunistic CT diagnosis of osteoporosis as primary clinical indication. Acknowledges equivalent fracture prediction of strength estimates from CT-to-FE vs. aBMD (hip) or vBMD (spine)
Benemerito I, Griffiths W, Allsopp J, Furnass W, Bhattacharya P, Li X, Marzo A, Wood S, Viceconti M, Narracott A. Delivering computationally-intensive digital patient applications to the clinic: An exemplar solution to predict femoral bone strength from CT data. Comput Methods Prog Biomed. 2021;208:106200.
Lee Y, Ogihara N, Lee T. Assessment of finite element models for prediction of osteoporotic fracture. J Mech Behav Biomed Mater. 2019;97:312–20. Reviews methodological aspects of CT-to-FE, and claims consolidation of advancements in FE analysis before entering clinical scenarios
Falcinelli C, Whyne C. Image-based finite-element modeling of the human femur. Comput Methods Biomech Biomed Engin. 2020;23:1138–61. Reviews methodological aspects of femoral CT-to-FE; highlights similar (encouraging) results from different workflows; motivates the adoption of a standardized workflow
Zysset P, Qin L, Lang T, Khosla S, Leslie WD, Shepherd JA, Schousboe JT, Engelke K. Clinical Use of Quantitative Computed Tomography–Based Finite Element Analysis of the Hip and Spine in the Management of Osteoporosis in Adults: the 2015 ISCD Official Positions—Part II. J Clin Densitom. 2015;18:359–92.
Samelson EJ, Broe KE, Xu H, Yang L, Boyd S, Biver E, Szulc P, Adachi J, Amin S, Atkinson E, Berger C, Burt L, Chapurlat R, Chevalley T, Ferrari S, Goltzman D, Hanley DA, Hannan MT, Khosla S, et al. Cortical and trabecular bone microarchitecture as an independent predictor of incident fracture risk in older women and men in the Bone Microarchitecture International Consortium (BoMIC): a prospective study. Lancet Diabetes Endocrinol. 2019;7:34–43.
Cody DD, Gross GJ, Hou FJ, Spencer HJ, Goldstein SA, Fyhrie DP. Femoral strength is better predicted by nite element models than QCT and DXA. J Biomech. 1999;32:1013–20.
Orwoll ES, Marshall LM, Nielson CM, Cummings SR, Lapidus J, Cauley JA, Ensrud K, Lane N, Hoffmann PR, Kopperdahl DL, Keaveny TM, for the Osteoporotic Fractures in Men (MrOS) Study Group. Finite element analysis of the proximal femur and hip fracture risk in older men. J Bone Miner Res. 2009;24:475–83.
Keyak JH, Sigurdsson S, Karlsdottir G, Oskarsdottir D, Sigmarsdottir A, Zhao S, Kornak J, Harris TB, Sigurdsson G, Jonsson BY, Siggeirsdottir K, Eiriksdottir G, Gudnason V, Lang TF. Male–female differences in the association between incident hip fracture and proximal femoral strength: A finite element analysis study. Bone. 2011;48:1239–45.
Amin S, Kopperdhal DL, Melton LJ, Achenbach SJ, Therneau TM, Riggs BL, Keaveny TM, Khosla S. Association of hip strength estimates by finite-element analysis with fractures in women and men. J Bone Miner Res. 2011;26:1593–600.
Wang X, Sanyal A, Cawthon PM, Palermo L, Jekir M, Christensen J, Ensrud KE, Cummings SR, Orwoll E, Black DM, for the Osteoporotic Fractures in Men (MrOS) Research Group, Keaveny TM. Prediction of new clinical vertebral fractures in elderly men using finite element analysis of CT scans. J Bone Miner Res. 2012;27:808–16.
Imai K, Ohnishi I, Matsumoto T, Yamamoto S, Nakamura K. Assessment of vertebral fracture risk and therapeutic effects of alendronate in postmenopausal women using a quantitative computed tomography-based nonlinear finite element method. Osteoporos Int. 2009;20:801–10.
Falcinelli C, Schileo E, Balistreri L, Baruffaldi F, Bordini B, Viceconti M, Albisinni U, Ceccarelli F, Milandri L, Toni A, Taddei F. Multiple loading conditions analysis can improve the association between finite element bone strength estimates and proximal femur fractures: A preliminary study in elderly women. Bone. 2014;67:71–80.
Nishiyama KK, Ito M, Harada A, Boyd SK. Classification of women with and without hip fracture based on quantitative computed tomography and finite element analysis. Osteoporos Int. 2014;25:619–26.
Kopperdahl DL, Aspelund T, Hoffmann PF, Sigurdsson S, Siggeirsdottir K, Harris TB, Gudnason V, Keaveny TM. Assessment of incident spine and hip fractures in women and men using finite element analysis of CT scans. J Bone Miner Res. 2014;29:570–80.
Adams AL, Fischer H, Kopperdahl DL, et al. Osteoporosis and hip fracture risk from routine computed tomography scans: the fracture, osteoporosis, and CT utilization study (FOCUS): osteoporosis and hip fracture risk from routine CT scans. J Bone Miner Res. 2018;33:1291–301. Largest CT-to-FE cohort study (close to 4000 subjects), showing evidence of equivalent incidence fracture prediction for CT-to-FE strength and DXA aBMD
Allaire BT, Lu D, Johannesdottir F, Kopperdahl D, Keaveny TM, Jarraya M, Guermazi A, Bredella MA, Samelson EJ, Kiel DP, Anderson DE, Demissie S, Bouxsein ML. Prediction of incident vertebral fracture using CT-based finite element analysis. Osteoporos Int. 2019;30:323–31.
Johannesdottir F, Allaire B, Kopperdahl DL, Keaveny TM, Sigurdsson S, Bredella MA, Anderson DE, Samelson EJ, Kiel DP, Gudnason VG, Bouxsein ML. Bone density and strength from thoracic and lumbar CT scans both predict incident vertebral fractures independently of fracture location. Osteoporos Int. 2021;32:261–9.
Michalski AS, Besler BA, Burt LA, Boyd SK. Opportunistic CT screening predicts individuals at risk of major osteoporotic fracture. Osteoporos Int. 2021;32:1639–49. https://doi.org/10.1007/s00198-021-05863-0.
Viceconti M, Qasim M, Bhattacharya P, Li X. Are CT-based finite element model predictions of femoral bone strengthening clinically useful? Curr Osteoporos Rep. 2018;16:216–23.
Winsor C, Li X, Qasim M, Henak CR, Pickhardt PJ, Ploeg H, Viceconti M. Evaluation of patient tissue selection methods for deriving equivalent density calibration for femoral bone quantitative CT analyses. Bone. 2021;143:115759.
Prado M, Khosla S, Chaput C, Giambini H. Opportunistic application of phantom-less calibration methods for fracture risk prediction using QCT/FEA. Eur Radiol. 2021; https://doi.org/10.1007/s00330-021-08071-w.
Rayudu NM, Anitha DP, Mei K, Zoffl F, Kopp FK, Sollmann N, Löffler MT, Kirschke JS, Noël PB, Subburaj K, Baum T. Low-dose and sparse sampling MDCT-based femoral bone strength prediction using finite element analysis. Arch Osteoporos. 2020;15:17.
Nakanowatari K, Watanabe K, Mori K, Nakajima S, Sekine N, Mutsuzaki H. Evaluation of vertebral bone strength with a finite element method using low dose computed tomography imaging. J Orthop Sci. 2021;S0949-2658(21):00121–4.
Rayudu NM, Subburaj K, Mei K, Dieckmeyer M, Kirschke JS, Noël PB, Baum T. Finite element analysis-based vertebral bone strength prediction using MDCT data: how low can we go? Front Endocrinol. 2020;11:442. Reports CT dose reductions up to 90% at the vertebrae (by sparse sampling) and 50% at the femur (by sparse sampling or tube current reduction) combined with iterative reconstruction algorithms may not worsen CT-to-FE strength predictions derived from standard clinical protocols
Qasim M, Farinella G, Zhang J, Li X, Yang L, Eastell R, Viceconti M. Patient-specific finite element estimated femur strength as a predictor of the risk of hip fracture: the effect of methodological determinants. Osteoporos Int. 2016;27:2815–22.
Bhattacharya P, Altai Z, Qasim M, Viceconti M. A multiscale model to predict current absolute risk of femoral fracture in a postmenopausal population. Biomech Model Mechanobiol. 2019;18:301–18. Improves CT-to-FE prevalent fracture association using the ratio between the estimate of the fall-loads (stochastic sampling of directions, personalised inverse pendulum model) and bone strengts rather than bone strength alone
Fleps I, Guy P, Ferguson SJ, Cripton PA, Helgason B. Explicit finite element models accurately predict subject-specific and velocity-dependent kinetics of sideways fall impact. J Bone Miner Res. 2019;34:1837–50. Validates novel personalised, dynamic explicit FE model of the human body against controlled ex-vivo experiments (n=12) of sideways fall impacts from standing height. Reports good accuracy for peak impact force, effective pelvic stiffness, and actual fracture outcome upon the impact
Enns-Bray WS, Bahaloo H, Fleps I, et al. Biofidelic finite element models for accurately classifying hip fracture in a retrospective clinical study of elderly women from the AGES Reykjavik cohort. Bone. 2019;120:25–37. Applies dynamic CT-to-FE to predict incident fracture in the AGES cohort, using a metric of tensile tissue damage. On fallers, dynamic CT-to-FE improves incident fracture prediction (AUC 0.85 vs. 0.74 for aBMD). On the whole sample, Dynamic FE and aBMD are indistinguishable (AUC 0.72 vs 0.70). This work demonstrates that fall risk estimates have the highest priority
Sternheim A, Giladi O, Gortzak Y, Drexler M, Salai M, Trabelsi N, Milgrom C, Yosibash Z. Pathological fracture risk assessment in patients with femoral metastases using CT-based finite element methods. A retrospective clinical study. Bone. 2018;110:215–20. Derives, using validated CT-to-FE models, a typical strain ratio of pathological vs. contralateral healthy femurs in a cohort of pathological femoral fracture cases
Yosibash Z, Plitman Mayo R, Dahan G, Trabelsi N, Amir G, Milgrom C. Predicting the stiffness and strength of human femurs with real metastatic tumors. Bone. 2014;69:180–90.
Sternheim A, Traub F, Trabelsi N, Dadia S, Gortzak Y, Snir N, Gorfine M, Yosibash Z. When and where do patients with bone metastases actually break their femurs?: a CT-based finite element analysis. The Bone & Joint Journal. 2020;102-B:638–45. CT-to-FE, using the strain ratio threshold derived from pathological cases [31], outperforms a clinical standard (Mirels score) in terms of specificity and AUC (0.90 vs. 0.58) when predicting impending femoral fracture due to metastatic lesions in a clinical cohort
Eggermont F, Derikx LC, Verdonschot N, van der Geest ICM, de Jong MAA, Snyers A, van der Linden YM, Tanck E. Can patient-specific finite element models better predict fractures in metastatic bone disease than experienced clinicians?: Towards computational modelling in daily clinical practice. Bone & Joint Research. 2018;7:430–9.
Eggermont F, van der Wal G, Westhoff P, et al. Patient-specific finite element computer models improve fracture risk assessments in cancer patients with femoral bone metastases compared to clinical guidelines. Bone. 2020;130:115101. Obtains sensitivity and specificity prediction gains for metastasis-related femoral fractures that are impressively similar to those reported by [33], even though with a slightly different workflow and metric, and compared to a different clinical standard
Sas A, Ohs N, Tanck E, van Lenthe GH. Nonlinear voxel-based finite element model for strength assessment of healthy and metastatic proximal femurs. Bone Reports. 2020;12:100263.
Stadelmann MA, Schenk DE, Maquer G, Lenherr C, Buck FM, Bosshardt DD, Hoppe S, Theumann N, Alkalay RN, Zysset PK. Conventional finite element models estimate the strength of metastatic human vertebrae despite alterations of the bone’s tissue and structure. Bone. 2020;141:115598.
Haider IT, Simonian N, Schnitzer TJ, Edwards WB. Stiffness and strength predictions from finite element models of the knee are associated with lower-limb fractures after spinal cord injury. Ann Biomed Eng. 2021;49:769–79.
Brown JP, Engelke K, Keaveny TM, et al. Romosozumab improves lumbar spine bone mass and bone strength parameters relative to alendronate in postmenopausal women: results from the ARCH trial. J Bone Miner Res. 2021; https://doi.org/10.1002/jbmr.4409.
Ono K, Ohashi S, Oka H, Kadono Y, Yasui T, Matsumoto T, Omata Y, Tanaka S. Evaluations of daily teriparatide using finite-element analysis over 12 months in rheumatoid arthritis patients. J Bone Miner Metab. 2021;39:270–7. Uses CT-to-FE strength to longitudinally assess treatment with teriparatide, and finds association of increased N-terminal type I procollagen propeptide (PINP) at 1 and 3 months with increased CT-to-FE strength (although only at the lumbar spine) at 12 months
Hong N, Lee DC, Khosla S, Keaveny TM, Rhee Y. Comparison of vertebral and femoral strength between White and Asian adults using finite element analysis of computed tomography scans. J Bone Miner Res. 2020;35:2345–54.
Keyak JH, Kaneko TS, Khosla S, Amin S, Atkinson EJ, Lang TF, Sibonga JD. Hip load capacity and yield load in men and women of all ages. Bone. 2020;137:115321.
Sibonga J, Matsumoto T, Jones J, Shapiro J, Lang T, Shackelford L, Smith SM, Young M, Keyak J, Kohri K, Ohshima H, Spector E, LeBlanc A. Resistive exercise in astronauts on prolonged spaceflights provides partial protection against spaceflight-induced bone loss. Bone. 2019;128:112037.
Burkhart K, Allaire B, Anderson DE, Lee D, Keaveny TM, Bouxsein ML. Effects of long-duration spaceflight on vertebral strength and risk of spine fracture. J Bone Miner Res. 2020;35:269–76. Reports that long-duration spaceflight could induce persistent risk of vertebral fracture using CT-to-FE supplemented with musculoskeletal models to define a load-to-strength ratio
Kersh ME, Martelli S, Zebaze R, Seeman E, Pandy MG. Mechanical loading of the femoral neck in human locomotion: mechanical loading of the femoral neck in human locomotion. J Bone Miner Res. 2018;33:1999–2006.
Pellikaan P, Giarmatzis G, Vander Sloten J, Verschueren S, Jonkers I. Ranking of osteogenic potential of physical exercises in postmenopausal women based on femoral neck strains. PLoS One. 2018;13:e0195463.
Martelli S, Beck B, Saxby D, Lloyd D, Pivonka P, Taylor M. Modelling human locomotion to inform exercise prescription for osteoporosis. Curr Osteoporos Rep. 2020;18:301–11.
Warden SJ, Carballido-Gamio J, Weatherholt AM, Keyak JH, Yan C, Kersh ME, Lang TF, Fuchs RK. Heterogeneous spatial and strength adaptation of the proximal femur to physical activity: a within-subject controlled cross-sectional study. J Bone Miner Res. 2020;35:681–90. Supplements CT-to-FE with computational anatomy algorithms to understand effect of physical activity on bone adaptation
Fuchs RK, Carballido-Gamio J, Keyak JH, Kersh ME, Warden SJ. Physical activity induced adaptation can increase proximal femur strength under loading from a fall onto the greater trochanter. Bone. 2021;152:116090.
Treece GM, Gee AH. Independent measurement of femoral cortical thickness and cortical bone density using clinical CT. Med Image Anal. 2015;20:249–64.
Väänänen SP, Grassi L, Venäläinen MS, Matikka H, Zheng Y, Jurvelin JS, Isaksson H. Automated segmentation of cortical and trabecular bone to generate finite element models for femoral bone mechanics. Med Eng Phys. 2019;70:19–28.
Schileo E, Pitocchi J, Falcinelli C, Taddei F. Cortical bone mapping improves finite element strain prediction accuracy at the proximal femur. Bone. 2020;136:115348. Reports improvement in ex-vivo strain prediction by coupling a computational anatomy algorithm (Cortical Bone Mapping) and CT-to-FE to counteract CT blurring of thin cortical layers due mostly to partial volume effect
Rajapakse CS, Chang G. Micro-finite element analysis of the proximal femur on the basis of high-resolution magnetic resonance images. Curr Osteoporos Rep. 2018;16:657–64.
Rajapakse CS, Farid AR, Kargilis DC, Jones BC, Lee JS, Johncola AJ, Batzdorf AS, Shetye SS, Hast MW, Chang G. MRI-based assessment of proximal femur strength compared to mechanical testing. Bone. 2020;133:115227. First time validation of an MRI-to-FE workflow for the prediction of strength, stiffness and strain measured ex-vivo in proximal femurs
Rajapakse CS, Hotca A, Newman BT, Ramme A, Vira S, Kobe EA, Miller R, Honig S, Chang G. Patient-specific hip fracture strength assessment with microstructural MR imaging-based finite element modeling. Radiology. 2017;283:854–61. Detailed description and thorough verification of an MRI-to-FE workflow for the proximal femur (then validated in [54])
Zhang L, Wang L, Fu R, Wang J, Yang D, Liu Y, Zhang W, Liang W, Yang R, Yang H, Cheng X. In vivo assessment of age- and loading configuration-related changes in multiscale mechanical behavior of the human proximal femur using MRI-based finite element analysis. J Magn Reson Imaging. 2021;53:905–12.
Luo Y, Ahmed S, Leslie WD. Automation of a DXA-based finite element tool for clinical assessment of hip fracture risk. Comput Methods Prog Biomed. 2018;155:75–83.
Yang L, Parimi N, Orwoll ES, Black DM, Schousboe JT, Eastell R. Association of incident hip fracture with the estimated femoral strength by finite element analysis of DXA scans in the osteoporotic fractures in men (MrOS) study. Osteoporos Int. 2018;29:643–51.
Yang S, Luo Y, Yang L, Dall’Ara E, Eastell R, Goertzen AL, McCloskey EV, Leslie WD, Lix LM. Comparison of femoral strength and fracture risk index derived from DXA-based finite element analysis for stratifying hip fracture risk: A cross-sectional study. Bone. 2018;110:386–91.
Leslie WD, Luo Y, Yang S, Goertzen AL, Ahmed S, Delubac I, Lix LM. Fracture risk indices from DXA-based finite element analysis predict incident fractures independently from FRAX: the Manitoba BMD registry. J Clin Densitom. 2019;22:338–45. Largest so far reported image-to-FE study in osteoporosis (n=13978, from the Manitoba BMD registry). DXA-to-2DFE independently predics incident hip fracture, but was inferior to femoral neck T-score and FRAX including BMD
Colombo C, Libonati F, Rinaudo L, Bellazzi M, Ulivieri FM, Vergani L. A new finite element based parameter to predict bone fracture. PLoS One. 2019;14:e0225905.
Messina C, Acquasanta M, Rinaudo L, Tortora S, Arena G, Albano D, Sconfienza LM, Ulivieri FM. Short-term precision error of bone strain index, a new DXA-based finite element analysis software for assessing hip strength. J Clin Densitom. 2021;24:330–7.
Ulivieri FM, Rinaudo L. Beyond bone mineral density: a new dual X-ray absorptiometry index of bone strength to predict fragility fractures, the bone strain index. Front Med. 2021;7:590139. Clear explanation of the Bone Strain Index (BSI) concept from DXA-to-2DFE, and useful review of its clinical applications so far
Choisne J, Valiadis J-M, Travert C, Kolta S, Roux C, Skalli W. Vertebral strength prediction from Bi-Planar dual energy x-ray absorptiometry under anterior compressive force using a finite element model: An in vitro study. J Mech Behav Biomed Mater. 2018;87:190–6.
Väänänen SP, Grassi L, Flivik G, Jurvelin JS, Isaksson H. Generation of 3D shape, density, cortical thickness and finite element mesh of proximal femur from a DXA image. Med Image Anal. 2015;24:125–34.
Jazinizadeh F, Quenneville CE. 3D Analysis of the proximal femur compared to 2D analysis for hip fracture risk prediction in a clinical population. Ann Biomed Eng. 2021;49:1222–32.
Grassi L, Fleps I, Sahlstedt H, Väänänen SP, Ferguson SJ, Isaksson H, Helgason B. Validation of 3D finite element models from simulated DXA images for biofidelic simulations of sideways fall impact to the hip. Bone. 2021;142:115678. DXA-to-3DFE matches impressively well CT-to-FE [29] (including the actual fracture outcome classification) in the validation against impact experiments
Grassi L, Väänänen SP, Ristinmaa M, Jurvelin JS, Isaksson H. Prediction of femoral strength using 3D finite element models reconstructed from DXA images: validation against experiments. Biomech Model Mechanobiol. 2017;16:989–1000.
Ruiz Wills C, Olivares AL, Tassani S, Ceresa M, Zimmer V, González Ballester MA, del Río LM, Humbert L, Noailly J. 3D patient-specific finite element models of the proximal femur based on DXA towards the classification of fracture and non-fracture cases. Bone. 2019;121:89–99.
O’Rourke D, Beck BR, Harding AT, Watson SL, Pivonka P, Martelli S. Assessment of femoral neck strength and bone mineral density changes following exercise using 3D-DXA images. J Biomech. 2021;119:110315.
König N, Taylor WR, Armbrecht G, Dietzel R, Singh NB. Identification of functional parameters for the classification of older female fallers and prediction of ‘first-time’ fallers. J R Soc Interface. 2014;11:20140353.
Gillain S, Boutaayamou M, Schwartz C, Brüls O, Bruyère O, Croisier J-L, Salmon E, Reginster J-Y, Garraux G, Petermans J. Using supervised learning machine algorithm to identify future fallers based on gait patterns: a two-year longitudinal study. Exp Gerontol. 2019;127:110730.
Rhodes S, Batzdorf A, Sorci O, Peng M, Jankelovits A, Hornyak J, An J, Noël PB, Høilund-Carlsen PF, Alavi A, Rajapakse CS. Assessment of femoral neck bone metabolism using 18F-sodium fluoride PET/CT imaging. Bone. 2020;136:115351.
Colloca M, Blanchard R, Hellmich C, Ito K, van Rietbergen B. A multiscale analytical approach for bone remodeling simulations: Linking scales from collagen to trabeculae. Bone. 2014;64:303–13.
Iori G, Du J, Hackenbeck J, Kilappa V, Raum K. Estimation of cortical bone microstructure from ultrasound backscatter. IEEE Trans Ultrason Ferroelectr Freq Control. 2021;68:1081–95.
Peralta L, Maeztu Redin JD, Fan F, Cai X, Laugier P, Schneider J, Raum K, Grimal Q. Bulk wave velocities in cortical bone reflect porosity and compression strength. Ultrasound Med Biol. 2021;47:799–808.
Buckley K, Kerns JG, Vinton J, Gikas PD, Smith C, Parker AW, Matousek P, Goodship AE. Towards the in vivo prediction of fragility fractures with Raman spectroscopy. J Raman Spectrosc. 2015;46:610–8.
Manhard MK, Uppuganti S, Granke M, Gochberg DF, Nyman JS, Does MD. MRI-derived bound and pore water concentrations as predictors of fracture resistance. Bone. 2016;87:1–10.
Jones BC, Jia S, Lee H, Feng A, Shetye SS, Batzdorf A, Shapira N, Noël PB, Pleshko N, Rajapakse CS. MRI-derived porosity index is associated with whole-bone stiffness and mineral density in human cadaveric femora. Bone. 2021;143:115774.
Gustafsson A, Tognini M, Bengtsson F, Gasser TC, Isaksson H, Grassi L. Subject-specific FE models of the human femur predict fracture path and bone strength under single-leg-stance loading. J Mech Behav Biomed Mater. 2021;113:104118.
Demirtas A, Rajapakse CS, Ural A. Assessment of the multifactorial causes of atypical femoral fractures using a novel multiscale finite element approach. Bone. 2020;135:115318.
The American Socuety of Mechanical Engineers (2018) ASME V&V 40 – 2018, Assessing credibility of computational modeling through verification and validation: application to medical devices.
Smets J, Shevroja E, Hügle T, Leslie WD, Hans D. Machine learning solutions for osteoporosis—a review. J Bone Miner Res. 2021;36:833–51.
Ulivieri FM, Rinaudo L, Piodi LP, Messina C, Sconfienza LM, Sardanelli F, Guglielmi G, Grossi E. Bone strain index as a predictor of further vertebral fracture in osteoporotic women: An artificial intelligence-based analysis. PLoS One. 2021;16:e0245967. Promising AI approach to complement DXA-to-2DFE, whose accuracy should be however confirmed on independent cohorts
Villamor E, Monserrat C, Del Río L, Romero-Martín JA, Rupérez MJ. Prediction of osteoporotic hip fracture in postmenopausal women through patient-specific FE analyses and machine learning. Comput Methods Prog Biomed. 2020;193:105484.
Zhang M, Gong H, Zhang K, Zhang M. Prediction of lumbar vertebral strength of elderly men based on quantitative computed tomography images using machine learning. Osteoporos Int. 2019;30:2271–82.
Chandran V, Maquer G, Gerig T, Zysset P, Reyes M. Supervised learning for bone shape and cortical thickness estimation from CT images for finite element analysis. Med Image Anal. 2019;52:42–55.
Galbusera F, Cina A, Panico M, Albano D, Messina C. Image-based biomechanical models of the musculoskeletal system. Eur Radiol Exp. 2020;4:49.
Acknowledgements
This work was partially supported by the Italian Ministry of Health (qSINS project, grant number: RF-2016-02364359).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Imaging
Rights and permissions
About this article
Cite this article
Schileo, E., Taddei, F. Finite Element Assessment of Bone Fragility from Clinical Images. Curr Osteoporos Rep 19, 688–698 (2021). https://doi.org/10.1007/s11914-021-00714-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-021-00714-7