Abstract
Purpose of review
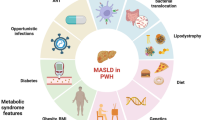
To update information about the relationship between metabolic dysfunction-associated steatotic liver disease (MASLD) and atherosclerosis. This review emphasizes the potential mechanisms linking MASLD with atherosclerosis and the possible causal relationships between these conditions.
Recent findings
An increased risk of cardiovascular disease is related to MASLD. Several molecular, cellular, and metabolic mechanisms have been described to explain the development of atherothrombosis in MASLD patients. These include atherogenic dyslipidemia, low-grade vascular inflammation, endothelial dysfunction, foam cell formation, proliferation of vascular smooth muscle cells, insulin resistance, gut microbiota dysbiosis, activation of renin-angiotensin and sympathetic nervous systems, hypercoagulability, and decreased fibrinolysis. Also, there is recent evidence suggesting an association between genetically driven liver fat and coronary heart disease mediated by the causal effect of apoB-containing lipoproteins. Several meta-analyses and systematic reviews have reported a strong association between MASLD and cardiovascular outcomes.
Summary
MASLD is an important and independent risk factor for atherosclerosis development. Multiple mechanisms may be involved in this association. Further research is required to establish a causal association between MASLD and atherosclerosis.

Similar content being viewed by others
Data Availability
No datasets were generated or analysed during the current study.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bril F, Cusi K. Nonalcoholic fatty liver disease: The new complication of type 2 diabetes mellitus. Endocrinol Metab Clin N Am. 2016;45:765–81.
Bril F, Cusi K. Management of nonalcoholic fatty liver disease in patients with type 2 diabetes: A call to action. Diabetes Care. 2017;40:419–30.
Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J Hepatol. 2020;73:202–9.
Rinella ME, Lazarus JV, Ratziu V, Francque SM, Sanyal AJ, et al. A multi-society Delphi consensus statement on new fatty liver disease nomenclature. J Hepatol. 2023;79:1542–56.
Zheng KI, Sun DQ, Jin Y, Zhu PW, Zheng MH. Clinical utility of the MAFLD definition. J Hepatol. 2021;74:989–91.
Hagström H, Vessby J, Ekstedt M, Shang Y. 99% of patients with NAFLD meet MASLD criteria and natural history is therefore identical. J Hepatol. 2024;80(2):e76–7.
Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, Charlton M, Sanyal AJ. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology. 2012;142:1592–609.
Balta S. Atherosclerosis and non-alcoholic fatty liver disease. Angiology. 2022;73:701–11.
Niederseer D, Wernly B, Aigner E, Stickel F, Datz C. NAFLD and Cardiovascular Diseases: Epidemiological, Mechanistic and Therapeutic Considerations. J Clin Med. 2021;10(3):467.
Brea A, Puzo J. Non-alcoholic fatty liver disease and cardiovascular risk. Int J Cardiol. 2013;167:1109–17.
Leey J, Cusi K. Editorial: diabetes, obesity and clinical inertia-the recipe for advanced NASH. Aliment Pharmacol Ther. 2018;47:1220–1.
Davis TME. Diabetes and metabolic dysfunction-associated fatty liver disease. Metabolism. 2021;123: 154868.
Wen W, Li H, Wang C, Chen C, Tang J, Zhou M, Hong X, Cheng Y, Wu Q, Zhang X, Feng Z, Wang M. Metabolic dysfunction-associated fatty liver disease and cardiovascular disease: a meta-analysis. Front Endocrinol (Lausanne). 2022;13: 934225.
Mantovani A, Csermely A, Tilg H, Byrne CD, Targher G. Comparative effects of non-alcoholic fatty liver disease and metabolic dysfunction-associated fatty liver disease on risk of incidente cardiovascular events: a meta-analysis of about 13 million individuals. Gut. 2023;72:1433–6.
Schonmann Y, Yeshua H, Bentov I, Zelber-Sagi S. Liver fbrosis marker is an independent predictor of cardiovascular morbidity and mortality in the general population. Dig Liver Dis. 2021;53:79–85.
Baratta F, Pastori D, Angelico F, Balla A, Paganini AM, Cocomello N, Ferro D, Violi F, Sanyal AJ, Del Ben M. Nonalcoholic fatty liver disease and fibrosis associated with increased risk of cardiovascular events in a prospective study. Clin Gastroenterol Hepatol. 2020;18:2324-2331.e4.
Tamaki N, Kurosaki M, Takahashi Y, Itakura Y, Inada K, Kirino S, Yamashita K, Sekiguchi S, Hayakawa Y, Osawa L, Higuchi M, Takaura K, Maeyashiki C, Kaneko S, Yasui Y, Tsuchiya K, Nakanishi H, Itakura J, Izumi N. Liver fbrosis and fatty liver as independent risk factors for cardiovascular disease. J Gastroenterol Hepatol. 2021;36:2960–6.
Han E, Lee YH, Lee JS, Lee HW, Kim BK, Park JY, Kim DY, Ahn SH, Lee BW, Kang ES, Cha BS, Kim SU. Fibrotic burden determines cardiovascular risk among subjects with metabolic dysfunction-associated fatty liver disease. Gut Liver. 2022;16:786–97.
Duell PB, Welty FK, Miller M, Chait A, Hammond G, Ahmad Z, et al. Nonalcoholic fatty liver disease and cardiovascular risk: a scientific statement from the American Heart Association. Arterioscler Thromb Vasc Biol. 2022;42:e168–85.
Kasper P, Martin A, Lang S, Kütting F, Goeser T, Demir M, Steffen HM. NAFLD and cardiovascular diseases: a clinical review. Clin Res Cardiol. 2021;110:921–93721.
•Zhang L, She ZG, Li H, Zhang XJ. Non-alcoholic fatty liver disease: a metabolic burden promoting atherosclerosis. Clin Sci (Lond). 2020;134:1775–99. This review summarizes the key molecular events and cellular factors contributing to the metabolic burden induced by NAFLD on atherosclerosis.
•Li M, Wang H, Zhang XJ, Cai J, Li H. NAFLD: an emerging causal factor for cardiovascular disease. Physiology (Bethesda). 2023;38(6):0. This review summarizes the evidence from prospective clinical and Mendelian randomization studies that underscore the potential causal relationship between NAFLD and cardiovascular disease.
Bali AD, Rosenzveig A, Frishman WH, Aronow WS. Nonalcoholic fatty liver disease and cardiovascular disease: causation or association. Cardiol Rev. 2023;24:e000537.
Bril F, Lomonaco R, Cusi K. The challenge of managing dyslipidemia in patients with nonalcoholic fatty liver disease. Clin Lipidol. 2012;7:471–81.
Martin A, Lang S, Goeser T, Demir M, Steffen HM, Kasper P. Management of dyslipidemia in patients with non-alcoholic fatty liver disease. Curr Atheroscler Rep. 2022;24:533–46.
Behbodikhah J, Ahmed S, Elsayi A, Kasselman LJ, De Leon J, Glass AD, Reiss AB. Apolipoprotein B and cardiovascular disease: biomarker and potential therapeutic target. Metabolites. 2021;11:690.
Cole J, Zubirán R, Wolska A, Jialal I, Remaley AT. Use of apolipoprotein B in the era of precision medicine: time for a paradigm change? J Clin Med. 2023;12:5737.
Matikainen N, Taskinen MR, Stennabb S, Lundbom N, Hakkarainen A, Vaaralahti K, Raivio T. Decrease in circulating fibroblast growth factor 21 after an oral fat load is related to postprandial triglyceride-rich lipoproteins and liver fat. Eur J Endocrinol. 2012;166:487–92.
Mehta A, Shapiro MD. Apolipoproteins in vascular biology and atherosclerotic disease. Nat Rev Cardiol. 2022;19:168–79.
Hegele RA. Apolipoprotein C-III inhibition to lower triglycerides: one ring to rule them all? Eur Heart J. 2022;43:1413–5.
de la Parra Soto LG, Gutiérrez-Uribe JA, Sharma A, Ramírez-Jiménez AK. Is apo-CIII the new cardiovascular target? An analysis of its current clinical and dietetic therapies. Nutr Metab Cardiovasc Dis. 2022;32:295–308.
Deprince A, Hennuyer N, Kooijman S, Pronk ACM, Baugé E, Lienard V, et al. Apolipoprotein F is reduced in humans with steatosis and controls plasma triglyceride-rich lipoprotein metabolism. Hepatology. 2023;77:1287–302.
Hafiane A, Gianopoulos I, Sorci-Thomas MG, Daskalopoulou SS. Current models of apolipoproteina A-I lipidation by adenosine triphosphate binding cassette transporter A1. Curr Opin Lipidol. 2022;33:139–45.
Naito C, Hashimoto M, Watanabe K, Shirai R, Takahashi Y, Kojima M, Watanabe R, Sato K, Iso Y, Matsuyama TA, Suzuki H, Ishibashi-Ueda H, Watanabe T. Facilitatory effects of fetuin-A on atherosclerosis. Atherosclerosis. 2016;246:344–51.
Gupta RM, Libby P, Barton M. Linking regulation of nitric oxide to endothelin-1: the yin and yang of vascular tone in the atherosclerotic plaque. Atherosclerosis. 2020;292:201–3.
Rafnsson A, Matic LP, Lengquist M, Mahdi A, Shemyakin A, Paulsson-Berne G, Hansson GK, Gabrielsen A, Hedin U, Yang J, Pernow J. Endothelin-1 increases expression and activity of arginase 2 via ETB receptors and is co-expressed with arginase 2 in human atherosclerotic plaques. Atherosclerosis. 2020;292:215–23.
Loffredo L, Baratta F, Ludovica P, Battaglia S, Carnevale R, Nocella C, Novo M, Pannitteri G, Ceci F, Angelico F, Violi F, Del Ben M. Effects of dark chocolate on endothelial function in patients with non-alcoholic steatohepatitis. Nutr Metab Cardiovasc Dis. 2018;28:143–9.
Jiang M, Zhao XM, Jiang ZS, Wang GX, Zhang DW. Protein tyrosine nitration in atherosclerotic endothelial dysfunction. Clin Chim Acta. 2022;529:34–41.
Love KM, Barrett EJ, Malin SK, Reusch JEB, Rogensteiner JG, Liu Z. Diabetes pathogenesis and management: the endothelium comes of age. J Mol Cell Biol. 2021;13:500–12.
Su X, Chen S, Liu J, Feng Y, Han E, Hao X, Liao M, Cai J, Zhang S, Niu J, He S, Huang S, Lo K, Zeng F. Composition of gut microbiota and non-alcoholic fatty liver disease: a systematic review and meta-analysis. Obes Rev. 2023;9: e13646.
Jadhav PA, Thomas AB, Nanda RK, Chitlange SS. Unveiling the role of gut dysbiosis in non-alcoholic fatty liver disease. Eur J Gastroenterol Hepatol. 2023;35(12):1324–33.
AL Samarraie A, Pichette M, Rousseau G. Role of the gut microbiome in the development of atherosclerotic cardiovascular disease. Int J Mol Sci. 2023;24:5420.
Oktaviono YH, Dyah Lamara A, Saputra PBT, Arnindita JN, Pasahari D, Saputra ME, Suasti NMA. The roles of trimethylamine-N-oxide in atherosclerosis and its potential therapeutic aspect: a literature review. Biomol Biomed. 2023;23(6):936–48.
Jing L, Zhang H, Xiang Q, Shen L, Guo X, Zhai C, Hu H. Targeting trimethylamine N-oxide: a new therapeutic strategy for alleviating atherosclerosis. Front Cardiovasc Med. 2022;9: 864600.
Querio G, Antoniotti S, Geddo F, Levi R, Gallo MP. Modulation of endothelial function by TMAO, a gut microbiota-derived metabolite. Int J Mol Sci. 2023;24:5806.
Bataller R, Sancho-Bru P, Ginès P, Lora JM, Al-Garawi A, Solé M, Colmenero J, Nicolás JM, Jiménez W, Weich N, Gutiérrez-Ramos JC, Arroyo V, Rodés J. Activated human hepatic stellate cells express the renin-angiotensin system and synthesize angiotensin II. Gastroenterology. 2003;125:117–25.
Aminuddin A, Cheong SS, Roos NAC, Ugusman A. Smoking and unstable plaque in acute coronary syndrome: a systematic review of the role of matrix metalloproteinases. Int J Med Sci. 2023;20:482–92.
Mantovani A, Csermely A, Petracca G, Beatrice G, Corey KE, Simon TG, Byrne CD, Targher G. Non-alcoholic fatty liver disease and risk of fatal and non-fatal cardiovascular events: an updated systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2021;6:903–13.
Koulaouzidis G, Charisopoulou D, Kukla M, Marlicz W, Rydzewska G, Koulaouzidis A, Skonieczna-Zydecka K. Association of non-alcoholic fatty liver disease with coronary artery calcification progression: a systematic review and meta-analysis. Prz Gastroenterology. 2021;16:196–206.
Alon L, Corica B, Raparelli V, Cangemi R, Basili S, Proietti M, Romiti GF. Risk of cardiovascular events in patients with non-alcoholic fatty liver disease: a systematic review and meta-analysis. Eur J Prev Cardiol. 2022;29:938–46.
Lee H, Lee YH, Kim SU, Kim HC. Metabolic dysfunction-associated fatty liver disease and incident cardiovascular risk: a nationwide cohort study. Clin Gastroenterol Hepatol. 2021;19:2138–47.
Quek J, Ng CH, Tang ASP, Chew N, Chan M, Khoo CM, et al. Metabolic associated fatty liver disease increases the risk of systemic complications and mortality. A meta-analysis and systematic review of 12,620,736 individuals. Endocr Pract. 2022;28:667–72.
Fu CE, Ng CH, Yong JN, Chan KE, Xiao J, et al. A meta-analysis on associated risk of mortality in nonalcoholic fatty liver disease. Endocr Pract. 2023;29:33–9.
Bisaccia G, Ricci F, Khanji MY, Sorella A, Melchiorre E, et al. Cardiovascular morbidity and mortality related to non-alcoholic fatty liver disease: A systematic review and meta-analysis. Curr Probl Cardiol. 2023;48: 101643.
Jamalinia M, Zare F, Lankarani KB. Systematic review and meta-analysis: Association between liver fibrosis and subclinical atherosclerosis in nonalcoholic fatty liver disease. Aliment Pharmacol Ther. 2023;58:384–94.
Lauridsen BK, Stender S, Kristensen TS, Kofoed KF, Køber L, Nordestgaard BG, Tybjaerg-Hansen A. Liver fat content, non-alcoholic fatty liver disease, and ischaemic heart disease: Mendelian randomization and meta-analysis of 279,013 individuals. Eur Heart J. 2018;39:385–93.
Brouwers MCGJ, Simons N, Stehouwer CDA, Koek GH, Schaper NC, Isascs A. Relationship between nonalcoholic fatty liver disease susceptibility genes and coronary artery disease. Hepatol Commun. 2019;3:587–96.
Castillo-Núnez Y, Morales-Villegas E, Aguilar-Salinas CA. Triglyceride-rich lipoproteins: Their role in atherosclerosis. Rev Invest Clin. 2022;74:061–70.
Björnson E, Samaras D, Adiels M, Kullberg J, Bäckhed F, Bergström G, Gummesson A. Mediating role of atherogenic lipoproteins in the relationship between liver fat and coronary artery calcification. Sci Rep. 2023;13:13217.
••Björnson E, Adiels M, Bergström G, Gummesson A. The relationship between genetic liver fat and coronary heart disease is explained by apoB-containing lipoproteins. Atherosclerosis. 2024;388:117397. https://doi.org/10.1016/j.atherosclerosis.2023.117397. this is a genome-wide association study in the UK Biobank, using MR analyses, suggesting that the relationship between genetically-determinated liver fat and coronary heart disease is mediated by the causal effect of apoB.
Ren Z, Simons PIHG, Wesselius A, Stehouwer CDA, Brouwers MCGJ. Relationship between NAFLD and coronary artery disease: A Mendelian randomization study. Hepatology. 2023;77:230–8.
Author information
Authors and Affiliations
Contributions
All the authors wrote and reviewed the manuscript's text (YC, GG, PA, RA). YC prepared Fig. 1.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing of interests.
Human and Animal Rights and Informed of Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Castillo-Núñez, Y., Almeda-Valdes, P., González-Gálvez, G. et al. Metabolic dysfunction-associated steatotic liver disease and atherosclerosis. Curr Diab Rep (2024). https://doi.org/10.1007/s11892-024-01542-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s11892-024-01542-6