Abstract
Purpose of the Review
To discuss the pivotal role of Interventional radiology (IR) for the management of colorectal liver metastases (CRLM).
Recent Findings
IR has three main objectives for the treatment of CRLM:
Complete tumor destruction using percutaneous ablation, as an alternative to or more frequently in combination with surgery
Intra-arterial therapies to improve objective response rate and to prolong survival
All support therapies such as portal vein embolization or fiducial placement to allow or facilitate further treatments
Summary
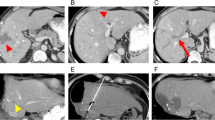
Radiofrequency ablation (RFA) is the most reported percutaneous ablation technique and provides high local control rates that exceed 90% for small metastases (< 3 cm). Novel technologies such as microwave ablation could help overcome some limitations of RFA. Liver metastases non-amenable to radical treatment can, because of their arterial supply, be targeted with hepatic arterial infusion chemotherapy (HAIC) or selective internal radiation therapy (SIRT). HAIC has demonstrated encouraging response rates in patients who have previously failed intravenous chemotherapy or as adjuvant therapies to decrease post-operative recurrence rates. Although large SIRT trials are negative, there is a benefit in terms of progression-free survival in the liver when used as first-line treatment in combination with systemic therapy as well as in selected patients with advanced disease that justifies further interest in this technique. More recent developments, such as stereotactic body radiation therapy of liver metastases or local administration of immunotherapies, require the contribution of IR. Interventional radiology is growing and is becoming standard of care for colorectal liver metastases. Further innovations are likely to improve its impact.



Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Torzilli G, Adam R, Vigano L, Imai K, Goransky J, Fontana A, et al. Surgery of colorectal liver metastases: pushing the limits. Liver Cancer. 2016;6(1):80–9. https://doi.org/10.1159/000449495.
Tsitskari M, Filippiadis D, Kostantos C, Palialexis K, Zavridis P, Kelekis N, et al. The role of interventional oncology in the treatment of colorectal cancer liver metastases. Ann Gastroenterol. 2019;32(2):147–55. https://doi.org/10.20524/aog.2018.0338.
•• Van Cutsem E, Cervantes A, Adam R, Sobrero A, Van Krieken JH, Aderka D, et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol. 2016;27(8):1386–422. https://doi.org/10.1093/annonc/mdw235Most used guidelines for the management of CRLM including IR technics.
de Baere T, Deschamps F, Briggs P, Dromain C, Boige V, Hechelhammer L, et al. Hepatic malignancies: percutaneous radiofrequency ablation during percutaneous portal or hepatic vein occlusion. Radiology. 2008;248(3):1056–66. https://doi.org/10.1148/radiol.2483070222.
Van Tilborg AA, Meijerink MR, Sietses C, Van Waesberghe JH, Mackintosh MO, Meijer S, et al. Long-term results of radiofrequency ablation for unresectable colorectal liver metastases: a potentially curative intervention. Br J Radiol. 2011;84(1002):556–65. https://doi.org/10.1259/bjr/78268814.
Shady W, Petre EN, Do KG, Gonen M, Yarmohammadi H, Brown KT, et al. Percutaneous microwave versus radiofrequency ablation of colorectal liver metastases: ablation with clear margins (A0) provides the best local tumor control. J Vasc Interv Radiol. 2018;29(2):268–75 e1. https://doi.org/10.1016/j.jvir.2017.08.021.
• Tanis E, Nordlinger B, Mauer M, Sorbye H, van Coevorden F, Gruenberger T, et al. Local recurrence rates after radiofrequency ablation or resection of colorectal liver metastases. Analysis of the European Organisation for Research and Treatment of Cancer #40004 and #40983. Eur J Cancer. 2014;50(5):912–9. https://doi.org/10.1016/j.ejca.2013.12.008Comparison of local recurrence after RFA and surgical management of CRLM showing no difference for tumor smaller than 4 cm.
•• Ruers T, Van Coevorden F, Punt CJ, Pierie JE, Borel-Rinkes I, Ledermann JA, et al. Local treatment of unresectable colorectal liver metastases: results of a randomized phase II trial. J Natl Cancer Inst. 2017;109(9). https://doi.org/10.1093/jnci/djx015Pivotal prospective study showing the positive impact on survival of tumor ablation for bilateral CRLM.
Karanicolas PJ, Jarnagin WR, Gonen M, Tuorto S, Allen PJ, DeMatteo RP, et al. Long-term outcomes following tumor ablation for treatment of bilateral colorectal liver metastases. JAMA Surg. 2013;148(7):597–601. https://doi.org/10.1001/jamasurg.2013.1431.
Song P, Sheng L, Sun Y, An Y, Guo Y, Zhang Y. The clinical utility and outcomes of microwave ablation for colorectal cancer liver metastases. Oncotarget. 2017;8(31):51792–9. https://doi.org/10.18632/oncotarget.15244.
van Riel JM, Peters GJ, Mammatas LH, Honeywell RJ, Laan AC, Ruyter R, et al. A phase I and pharmacokinetic study of gemcitabine given by 24-h hepatic arterial infusion. Eur J Cancer. 2009;45(14):2519–27. https://doi.org/10.1016/j.ejca.2009.05.025.
Florcken A, Schaefer C, Bichev D, Breithaupt K, Dogan Y, Schumacher G, et al. Hepatic arterial infusion chemotherapy for liver metastases from gastric cancer: an analysis in Western patients. Tumori. 2011;97(1):19–24.
Ensminger WD, Rosowsky A, Raso V, Levin DC, Glode M, Come S, et al. A clinical-pharmacological evaluation of hepatic arterial infusions of 5-fluoro-2′-deoxyuridine and 5-fluorouracil. Cancer Res. 1978;38(11 Pt 1):3784–92.
Dzodic R, Gomez-Abuin G, Rougier P, Bonnay M, Ardouin P, Gouyette A, et al. Pharmacokinetic advantage of intra-arterial hepatic oxaliplatin administration: comparative results with cisplatin using a rabbit VX2 tumor model. Anti-Cancer Drugs. 2004;15(6):647–50.
Mocellin S, Pasquali S, Nitti D. Fluoropyrimidine-HAI (hepatic arterial infusion) versus systemic chemotherapy (SCT) for unresectable liver metastases from colorectal cancer. Cochrane Database Syst Rev. 2009;3:CD007823. https://doi.org/10.1002/14651858.CD007823.pub2.
Chapelle N, Matysiak-Budnik T, Douane F, Metairie S, Rougier P, Touchefeu Y. Hepatic arterial infusion in the management of colorectal cancer liver metastasis: current and future perspectives. Dig Liver Dis. 2018;50(3):220–5. https://doi.org/10.1016/j.dld.2017.12.004.
Kemeny NE, Melendez FD, Capanu M, Paty PB, Fong Y, Schwartz LH, et al. Conversion to resectability using hepatic artery infusion plus systemic chemotherapy for the treatment of unresectable liver metastases from colorectal carcinoma. J Clin Oncol. 2009;27(21):3465–71. https://doi.org/10.1200/JCO.2008.20.1301.
Goere D, Deshaies I, de Baere T, Boige V, Malka D, Dumont F, et al. Prolonged survival of initially unresectable hepatic colorectal cancer patients treated with hepatic arterial infusion of oxaliplatin followed by radical surgery of metastases. Ann Surg. 2010;251(4):686–91. https://doi.org/10.1097/SLA.0b013e3181d35983.
Boige V, Malka D, Elias D, Castaing M, De Baere T, Goere D, et al. Hepatic arterial infusion of oxaliplatin and intravenous LV5FU2 in unresectable liver metastases from colorectal cancer after systemic chemotherapy failure. Ann Surg Oncol. 2008;15(1):219–26. https://doi.org/10.1245/s10434-007-9581-7.
Ducreux M, Ychou M, Laplanche A, Gamelin E, Lasser P, Husseini F, et al. Hepatic arterial oxaliplatin infusion plus intravenous chemotherapy in colorectal cancer with inoperable hepatic metastases: a trial of the gastrointestinal group of the federation Nationale des Centres de Lutte Contre le Cancer. J Clin Oncol. 2005;23(22):4881–7. https://doi.org/10.1200/JCO.2005.05.120.
•• Kemeny N, Huang Y, Cohen AM, Shi W, Conti JA, Brennan MF, et al. Hepatic arterial infusion of chemotherapy after resection of hepatic metastases from colorectal cancer. N Engl J Med. 1999;341(27):2039–48. https://doi.org/10.1056/NEJM199912303412702First important paper on the impact of hepatic arterial infusion for CRLM.
Lygidakis NJ, Sgourakis G, Vlachos L, Raptis S, Safioleas M, Boura P, et al. Metastatic liver disease of colorectal origin: the value of locoregional immunochemotherapy combined with systemic chemotherapy following liver resection. Results of a prospective randomized study. Hepatogastroenterology. 2001;48(42):1685–91.
House MG, Kemeny NE, Gonen M, Fong Y, Allen PJ, Paty PB, et al. Comparison of adjuvant systemic chemotherapy with or without hepatic arterial infusional chemotherapy after hepatic resection for metastatic colorectal cancer. Ann Surg. 2011;254(6):851–6. https://doi.org/10.1097/SLA.0b013e31822f4f88.
Kerr DJ, McArdle CS, Ledermann J, Taylor I, Sherlock DJ, Schlag PM, et al. Intrahepatic arterial versus intravenous fluorouracil and folinic acid for colorectal cancer liver metastases: a multicentre randomised trial. Lancet. 2003;361(9355):368–73. https://doi.org/10.1016/S0140-6736(03)12388-4.
Deschamps F, Rao P, Teriitehau C, Hakime A, Malka D, Boige V, et al. Percutaneous femoral implantation of an arterial port catheter for intraarterial chemotherapy: feasibility and predictive factors of long-term functionality. J Vasc Interv Radiol. 2010;21(11):1681–8. https://doi.org/10.1016/j.jvir.2010.08.003.
Deschamps F, Elias D, Goere D, Malka D, Ducreux M, Boige V, et al. Intra-arterial hepatic chemotherapy: a comparison of percutaneous versus surgical implantation of port-catheters. Cardiovasc Intervent Radiol. 2011;34(5):973–9. https://doi.org/10.1007/s00270-010-9996-6.
Fiorentini G, Aliberti C, Tilli M, Mulazzani L, Graziano F, Giordani P, et al. Intra-arterial infusion of irinotecan-loaded drug-eluting beads (DEBIRI) versus intravenous therapy (FOLFIRI) for hepatic metastases from colorectal cancer: final results of a phase III study. Anticancer Res. 2012;32(4):1387–95.
Akinwande O, Dendy M, Ludwig JM, Kim HS. Hepatic intra-arterial injection of irinotecan drug eluting beads (DEBIRI) for patients with unresectable colorectal liver metastases: a systematic review. Surg Oncol. 2017;26(3):268–75. https://doi.org/10.1016/j.suronc.2017.05.003.
Benzakoun J, Ronot M, Lagadec M, Allaham W, Garcia Alba C, Sibert A, et al. Risks factors for severe pain after selective liver transarterial chemoembolization. Liver Int. 2016. https://doi.org/10.1111/liv.13235.
Denys A, Pracht M, Duran R, Guiu B, Adib S, Boubaker A, et al. How to prepare a patient for transarterial radioembolization? Pract Guide Cardiovasc Intervent Radiol. 2015;38(4):794–805. https://doi.org/10.1007/s00270-015-1071-x.
•• van Hazel GA, Heinemann V, Sharma NK, Findlay MP, Ricke J, Peeters M, et al. SIRFLOX: randomized phase III trial comparing first-line mFOLFOX6 (plus or minus bevacizumab) versus mFOLFOX6 (plus or minus bevacizumab) plus selective internal radiation therapy in patients with metastatic colorectal cancer. J Clin Oncol. 2016;34(15):1723–31. https://doi.org/10.1200/JCO.2015.66.1181Negative Randomized phase 3 trial on the added value of SIRT for metastatic colorectal cancer at 1st line.
Wasan HS, Gibbs P, Sharma NK, Taieb J, Heinemann V, Ricke J, et al. First-line selective internal radiotherapy plus chemotherapy versus chemotherapy alone in patients with liver metastases from colorectal cancer (FOXFIRE, SIRFLOX, and FOXFIRE-global): a combined analysis of three multicentre, randomised, phase 3 trials. Lancet Oncol. 2017;18(9):1159–71. https://doi.org/10.1016/S1470-2045(17)30457-6.
Sofocleous CT, Violari EG, Sotirchos VS, Shady W, Gonen M, Pandit-Taskar N, et al. Radioembolization as a salvage therapy for heavily pretreated patients with colorectal cancer liver metastases: factors that affect outcomes. Clin Colorectal Cancer. 2015;14(4):296–305. https://doi.org/10.1016/j.clcc.2015.06.003.
Sangro B, Gil-Alzugaray B, Rodriguez J, Sola I, Martinez-Cuesta A, Viudez A, et al. Liver disease induced by radioembolization of liver tumors: description and possible risk factors. Cancer. 2008;112(7):1538–46. https://doi.org/10.1002/cncr.23339.
Smits ML, Nijsen JF, van den Bosch MA, Lam MG, Vente MA, Mali WP, et al. Holmium-166 radioembolisation in patients with unresectable, chemorefractory liver metastases (HEPAR trial): a phase 1, dose-escalation study. Lancet Oncol. 2012;13(10):1025–34. https://doi.org/10.1016/S1470-2045(12)70334-0.
de Baere T, Denys A, Paradis V. Comparison of four embolic materials for portal vein embolization: experimental study in pigs. Eur Radiol. 2009;19(6):1435–42. https://doi.org/10.1007/s00330-008-1277-2.
• Guiu B, Chevallier P, Denys A, Delhom E, Pierredon-Foulongne MA, Rouanet P, et al. Simultaneous trans-hepatic portal and hepatic vein embolization before major hepatectomy: the liver venous deprivation technique. Eur Radiol. 2016;26(12):4259–67. https://doi.org/10.1007/s00330-016-4291-9Novel technic of venous pre-operative liver embolization technic to improve results.
Petrelli F, Comito T, Barni S, Pancera G, Scorsetti M, Ghidini A, et al. Stereotactic body radiotherapy for colorectal cancer liver metastases: a systematic review. Radiother Oncol. 2018;129(3):427–34. https://doi.org/10.1016/j.radonc.2018.06.035.
Chang DT, Swaminath A, Kozak M, Weintraub J, Koong AC, Kim J, et al. Stereotactic body radiotherapy for colorectal liver metastases: a pooled analysis. Cancer. 2011;117(17):4060–9. https://doi.org/10.1002/cncr.25997.
Park SH, Won HJ, Kim SY, Shin YM, Kim PN, Yoon SM, et al. Efficacy and safety of ultrasound-guided implantation of fiducial markers in the liver for stereotactic body radiation therapy. PLoS One. 2017;12(6):e0179676. https://doi.org/10.1371/journal.pone.0179676.
Marsico M, Gabbani T, Livi L, Biagini MR, Galli A. Therapeutic usability of two different fiducial gold markers for robotic stereotactic radiosurgery of liver malignancies: a pilot study. World J Hepatol. 2016;8(17):731–8. https://doi.org/10.4254/wjh.v8.i17.731.
Jarraya H, Chalayer C, Tresch E, Bonodeau F, Lacornerie T, Mirabel X, et al. Novel technique for hepatic fiducial marker placement for stereotactic body radiation therapy. Int J Radiat Oncol Biol Phys. 2014;90(1):119–25. https://doi.org/10.1016/j.ijrobp.2014.05.002.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
F. Deschamps, M. Ronot, M. Gelli, J. Durand-Labrunie, M. Tazdait, and P. Dartigues each declare no potential conflicts of interest. A. Hollebecque has received personal fees from Incyte, Spectrum Pharmaceuticals, Debiopharm, and EISAI and nonfinancial support from Lilly, Servier, and Bayer. Dr. Hollebecque has also received grants from Astra Zeneca, BMS, Boehringer Ingelheim, Janssen Cilag, Merck, Novartis, Pfizer, Sanofi, and Roche. T. de Baere has received personal fees from Terumo, BTG, SIRTEX, GE, COOK, GUERBET, and CANON. L. Tselikas has received grants from Terumo and BMS and personal fees from COOK, EISAI, and AMGEN.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Diagnostic and Interventional Radiology Innovations in Colorectal Cancer
Rights and permissions
About this article
Cite this article
Deschamps, F., Ronot, M., Gelli, M. et al. Interventional Radiology for Colorectal Liver Metastases. Curr Colorectal Cancer Rep 16, 29–37 (2020). https://doi.org/10.1007/s11888-020-00449-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11888-020-00449-0