Abstract
Purpose of Review
Our goal in writing this review was to provide a comprehensive appraisal of current therapies for idiopathic recurrent pericarditis with a particular focus on the newest therapeutic agents. We sought to understand the role of the inflammasome in the pathophysiology of pericarditis and how it informs the use of interleukin-1 (IL-1)-directed therapies.
Recent Findings
The latest research on this topic has focused on the critical role of the NLRP3 (NACHT, leucine-rich repeat, and pyrin domain-containing protein) inflammasome. Very recently, components of the NLRP3 inflammasome were detected by immune staining in pericardial tissue from patients with recurrent idiopathic pericarditis. In a mouse model of pericarditis, anti-IL-1 agents anakinra and rilonacept reduced NLRP3 immunostaining. Subsequent study of these drugs in human subjects with idiopathic recurrent pericarditis demonstrated their efficacy.
Summary
Recurrent idiopathic pericarditis, while relatively rare, poses a continued treatment challenge and contributes to a diminished quality of life for those patients who are afflicted. Recent developments, including an animal model of the disease and the use of IL-1-directed therapies, represent an exciting leap forward in our understanding of treatment targets. These advances offer not only new tools in our fight against this disease, but also the promise of earlier intervention and attenuation of disease morbidity. As our experience with these new agents expands, we can address questions about the ideal timing of introduction of anti-IL-1 therapy and duration of therapy and better understand the potential side effect profile.
Similar content being viewed by others
Introduction
Recent developments in our understanding of the pathophysiology of recurrent idiopathic pericarditis have transformed the treatment landscape and may favorably alter the long-term trajectory of this difficult problem. The following is a case presentation that will set the stage for a discussion of these new approaches.
Case Presentation
A 52-year-old man with no significant past medical history presented to the emergency department (ED) with progressive, pleuritic, substernal chest pain and dyspnea for 1 week. He felt markedly worse when supine. He denied a preceding illness or other symptoms. In the ED, T 38.1 °C, HR 98/min, BP 130/80 mmHg and O2 saturation 97% on RA. He appeared uncomfortable, and his cardiac examination was notable for a 3-component pericardial friction rub. ECG revealed ST elevation in all leads except AVR and V1. Lab data: WBC 10.7, hs-CRP 75 mg/L, troponin I normal. Echocardiogram was completely normal except for a small, circumferential pericardial effusion. Chest X-ray was also normal.
Acute idiopathic pericarditis was diagnosed, and the patient was discharged on ibuprofen 800 mg three times daily, colchicine 0.6 mg twice daily, and omeprazole. His symptoms resolved within 2–3 days. After 10 days of treatment, hs-CRP was < 1.0 mg/L. Repeat echocardiogram revealed resolution of the effusion. Ibuprofen and omeprazole were stopped at this point, and colchicine was continued for a total of 3 months of treatment.
Acute Pericarditis
Acute pericarditis is the most common form of pericardial disease [1, 2]. There are numerous causes, including infection, auto-immune diseases, uremia, malignancy, and post-injury (post-thoracotomy, post-MI, post-cardiac catheterization, and electrophysiology device or ablation procedures). However, idiopathic cases are by far the most common (idiopathic is taken to mean that no specific etiology emerges following a standard evaluation, as outlined in the case report). Most cases of acute idiopathic pericarditis are considered to be viral in origin, but this has never been systematically tested. Epidemiologic data are limited, but this diagnosis has an approximately 1% incidence at autopsy and accounts for approximately 5% of all emergency room patients diagnosed with non-ischemic chest pain [1, 2]. It is more common in males than females and in middle age versus younger and older patients. The etiology and epidemiology of pericarditis differs markedly based on geography, with tuberculosis now rare in the developed world but still quite common in underdeveloped countries. At least two of four key findings are required for diagnosis: typical chest pain, pericardial friction rub, typical ECG changes (PR depression, “diffuse” ST segment elevations), and pericardial effusion [3]. Although elevated CRP levels are supportive, they are not required for diagnosis. The cornerstones of treatment for an initial case of acute idiopathic pericarditis are exercise restriction, an anti-inflammatory regimen consisting of high-dose non-steroidal anti-inflammatories (most commonly ibuprofen or aspirin), and colchicine along with a PPI for gastric protection [3,4,5,6,7,8,9]. Corticosteroids are considered second-line therapy for an initial episode due to both short- and long-term side effects and the observation that they appear to increase the risk of recurrence, especially when used at high dose with a rapid taper [7, 10, 11]. Duration of therapy is guided by symptomatic improvement and serial assessment of CRP with a goal of normalization (approximately 75–80% of pericarditis patients have an elevated CRP upon presentation) [2, 3, 12, 13].
Case Update
The patient returned to the office 2 months after completion of colchicine therapy with the recent onset of identical symptoms of pleuritic chest pain and dyspnea. He did not have a friction rub, and his ECG was normal. Labs were notable for WBC 8.5, hs-CRP 25 mg/L, and a normal troponin I. Repeat echocardiogram revealed only a trivial pericardial effusion. Ibuprofen, colchicine, and omeprazole were re-initiated with resolution of symptoms within several days and hs-CRP normalization within 1 week. Ibuprofen was tapered off, and omeprazole was discontinued, and colchicine continued for a planned 3 months. Two months later, symptoms recurred. The patient was treated with prednisone 20 mg daily, and colchicine was continued. Symptoms cleared within a few days. The prednisone dose was gradually tapered over 3–4 months. With prednisone tapered to a dose of 4 mg daily, the patient had another recurrence of symptoms.
What Are the Therapeutic Options at this Point?
Diagnosis and Natural History of Recurrent Idiopathic Pericarditis
Recurrent pericarditis presents not only a painful and life-altering constellation of symptoms for the patient but is often a treatment conundrum for the clinician. Up to 30% of patients with a first episode of acute idiopathic pericarditis have at least 1 recurrence and of those around 1/3 to 1/2 have multiple recurrences [1, 9, 14]. Through their 2021 retrospective US database analysis of recurrent pericarditis, Dr. Klein and associates updated and deepened our understanding of the burden of this disease. Over a 2-year observation period after a first episode of pericarditis, 27.9% of patients had at least a single recurrence, with a mean recurrence number of 2.16. Interestingly, each recurrence made a next recurrence more likely. This was seen more often in patients with corticosteroid-dependent and refractory pericarditis. The timing of recurrent bouts of pericarditis was found to be shorter in patients with a higher burden of recurrent disease. Patients with recurrent pericarditis were also found to have higher rates of complications such as pericardial effusion and tamponade when compared to the acute pericarditis population [15•].
To diagnose recurrent pericarditis, the patient must have experienced complete remission of symptoms for at least 4 to 6 weeks prior to developing new symptoms and recurrent signs as outlined above [1, 2]. While some recurrences may result from incomplete or inadequate treatment of a first episode, they are not thought to be caused by a new viral or other insult. Recurrences often but not always present with milder symptoms than the first presentation, with less in the way of objective signs of pericardial inflammation. When idiopathic pericarditis first recurs, conventional treatment stays centered around anti-inflammatory medications, i.e., NSAIDs and colchicine, at similar doses as those used for an initial episode. Typically, a first recurrence responds very well to treatment with the typical anti-inflammatory medications listed in Table 1. However, treatment of subsequent recurrences often becomes problematic, with many patients receiving repeated courses of corticosteroids (CS) with their attendant difficulties. Immunosuppressive drugs such as azathioprine have had some success as corticosteroid-sparing therapy for recurrent pericarditis [16]. Methotrexate, mycophenolate mofetil, and intravenous immunoglobulin also demonstrated some apparent efficacy in CS-dependent cases or in those suffering unacceptable side effects from CS [17, 18]. Recurrent pericarditis is often a long-term problem with frequent, unpredictable flares that can markedly impair quality of life. Although most cases eventually resolve and complications such as constrictive pericarditis are extremely rare, the time to resolution is unpredictable. This has led to the continued search for new treatment targets.
Mechanistic Basis of Recurrent Idiopathic Pericarditis and Newer Therapies
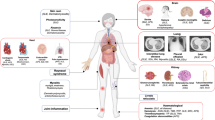
It has been theorized that recurrent idiopathic pericarditis is an auto-inflammatory disease caused by dysregulated production of the pro-inflammatory cytokines IL-1α/β. Pericardial injury results in the release of what are termed damage-associated molecular patterns (DAMPs) and/or pathogen-associated molecular patterns (PAMPs), leading to the inflammatory cascade illustrated in Fig. 1. This hypothesis was originally based on its resemblance to the periodic fever syndromes, especially Familial Mediterranean Fever. Periodic fever syndromes are inherited diseases which often feature recurrent bouts of pericarditis and respond dramatically to IL-1 directed treatment, for example, the IL-1 α/β blocking agent anakinra [19, 20]. Many patients with recurrent idiopathic pericarditis also have evidence of a more generalized polyserositis, e.g., pleural effusions, which is also reminiscent of periodic fever disorders. The underlying basis of the periodic fever syndromes is genetically determined dysregulation of the NLRP3 (NACHT, leucine-rich repeat, and pyrin domain-containing protein) inflammasome. NLRP3 is one of several inflammasomes that have been identified. NLRP3 is a complex, multi-protein component of the innate immune system which is assembled in macrophages mainly in vascular endothelium and becomes activated in response to various “danger” signals (PAMPs and DAMPs), where its caspase component functions to convert inactive to active IL-1β [21••, 22]. In contrast, IL-1α is produced locally in damaged tissues. Very recently, components of the NLRP3 inflammasome were detected by immune staining in pericardial tissue from patients with recurrent idiopathic pericarditis. Staining was not evident in pericardial tissue from control subjects without pericardial disease. This is the first direct proof of the involvement of the NLRP3 inflammasome in recurrent pericarditis (Fig. 1) [21••, 22]. In a parallel study in a mouse model of pericarditis, both anakinra and rilonacept reduced NLRP3 immunostaining [23]. The role of NLRP3 in pericarditis is discussed in more detail below.
The role of the NLRP3 inflammasome in the pathophysiology of recurrent idiopathic pericarditis and as a therapeutic target. Colchicine reduces the activation of IL-1β via inhibition of NLRP3 inflammasome aggregation and caspase activation. Corticosteroids have numerous anti-inflammatory properties including inhibition of NFkB and phospholipase A2 and their downstream inflammatory effects. NSAIDs and aspirin inhibit COX-2 activity, thereby preventing the conversion of arachidonic acid to various proinflammatory molecules which contribute to clinical pericarditis. Anakinra blocks IL-1α and IL-1β from binding with IL receptors and inhibits their local, NFkB-mediated pro-inflammatory response. Rilonacept exerts similar effects via “trapping” of IL-1α and IL-1β to prevent their binding to IL-1 receptors. The monoclonal antibody Canakinumab selectively inhibits IL-1β. ASC, apoptosis-associated speck-like protein containing a caspase recruitment domain; COX-2, cyclooxygenase-2; CRP, C-reactive protein; DAMP, damage-associated molecular pattern; IL, interleukin; IL-1Ra, interleukin 1 receptor antagonist; NFkB, nuclear factor k-light-chain-enhancer of activated B cells; TLR, Toll-like receptor; NLR, nod-like receptor; NSAIDs, non-steroidal anti-inflammatory drugs; PAMP, pathogen-associated molecular pattern; PLA2, phospholipase A2. Similar mechanistic components are illustrated in a different cell type in the JACC review by Chiabrando et al. [34]
Evidence for Clinical Use of Anti-IL-1 Agents
Three IL-1 directed agents are currently available: anakinra, rilonacept, and canakinumab. Based on the proposed mechanistic role of IL-1, each has been tested in recurrent pericarditis (Fig. 1). Support for the safety and clinical use of these therapies, particularly anakinra and rilonacept, is provided by randomized, placebo-controlled clinical trials and registry results.
Anakinra-AIRTRIP Trial
Anakinra is recombinant human IL-1Ra, a naturally occurring protein that blocks both IL-1α and β receptors. It is administered subcutaneously (s.c.) daily and is currently used in certain periodic fever syndromes and rheumatoid arthritis. AIRTRIP was a small, event-driven, double-blind, placebo-controlled, randomized withdrawal trial preceded by an open-label run-in phase during which anakinra (2 mg/kg s.c.) was administered to all patients during an active recurrence of idiopathic pericarditis associated with CRP elevation. During the run-in phase, symptoms rapidly resolved, and other anti-inflammatories including corticosteroids were successfully discontinued. During the randomized phase, patients were followed for 6 months or until recurrent pericarditis occurred. Recurrent pericarditis occurred in 90% of patients assigned to placebo and in 18% of those assigned to anakinra, a highly significant difference. Side effects of treatment were minor and most related to injection site skin reactions, which were quite common. No patients discontinued anakinra treatment [24]. Drug dosing and monitoring are summarized in Table 2. Study design and results are summarized in Table 3.
IRAP Registry
The International Registry of Anakinra for Pericarditis (IRAP) has confirmed the safety and efficacy of this treatment in a real-world clinical cohort of 224 patients. Most patients had an elevated CRP and a pericardial effusion (91% and 88%, respectively). After a median treatment of 6 months, recurrent pericarditis was reduced sixfold, emergency room visits were reduced 11-fold, and hospitalizations were reduced sevenfold. Corticosteroid use markedly decreased from 80 to 27% when anakinra was used. No serious adverse events were recorded, and, as in AIRTRIP, the most common was a transient skin reaction at the injection site, leading to discontinuation of this therapy in 3% of patients. Treatment of greater than 3 months followed by a slow taper over a period of at least 3 months was associated with lowering the risk of recurrence of pericarditis [25].
Rilonacept-RHAPSODY Trial
Rilonacept is the newest anti-IL-1 agent to be trialed in recurrent pericarditis. It is approved for use in certain periodic fever syndromes and recently received FDA approval for recurrent idiopathic pericarditis. Rilonacept is a fusion protein that acts to bind or “trap” both IL-1α and IL-1β, blocking their function and role in the inflammatory cascade leading to recurrent pericarditis. In an open-label phase II study, 25 adult patients with idiopathic or post-pericardiotomy pericarditis with at least two recurrences and/or corticosteroid-dependence (again with at least 2 recurrences) were enrolled. They received a 320 mg s.c. loading dose followed by weekly injections of 160 mg during a 6-week treatment period followed by an optional 18-week treatment extension. There was a rapid and sustained decrease in CRP and pericarditis manifestations as well as health-related improvement in quality of life [26].
This positive trial led to RHAPSODY, a phase III, multicenter, double-blind, event-driven, randomized withdrawal trial of rilonacept in patients suffering from acute symptoms of recurrent pericarditis (utilizing a patient-reported scale) and systemic inflammation (demonstrated by elevated CRP levels) [27•]. Like AIRTRIP, the enrolled patients received rilonacept for a 12-week run-in period at the same dosing as the phase II trial; during this phase, their other pericarditis treatments, including CS, were successfully discontinued. All enrollees met prespecified clinical response criteria (CRP level ≤ 0.5 mg/dl and mean daily pain score of ≤ 2, i.e., minimal to no pain) and then were randomly assigned to either continue therapy or switch to placebo. The median time to the primary endpoint of first pericarditis recurrence was 8.6 weeks. Recurrent pericarditis was defined as the return of pericarditis pain or an increase in the CRP level. If only elevated CRP was present, other objective evidence was required such as pericardial effusion, rub, or ECG changes. Only 2 patients (7%) receiving rilonacept experienced a recurrence of pericarditis, while 23 of 31 placebo patients (74%) experienced a recurrence. Four patients experienced adverse events that led to discontinuation of rilonacept during the run-in period. Injection site reactions (mild to moderate; 34% of participants affected, all of whom were rilonacept recipients) and upper respiratory tract infections (23% of rilonacept patients) were the most common reported adverse events, as summarized in Table 2 [27•]. Drug dosing and monitoring are summarized in Table 2. Study design and results are summarized in Table 3.
Canakinumab-CANTOS Trial
Canakinumab is a selective monoclonal antibody that blocks the effects of IL-1β. CANTOS was a large, phase III trial in which canakinumab was shown to have favorable effects on long-term outcomes in patients with prior myocardial infarction who were receiving optimal guideline-directed treatment, including lipid lowering therapy [28]. Its limited published use in pericarditis is based on case studies and uncontrolled case series, the results of which have been mixed and clearly not as favorable as anakinra or rilonacept [29, 30]. These results with canakinumab have led to the concept that both IL-1β and IL-1α activity underlie recurrent idiopathic pericarditis.
Safety of Anti-IL-1 Agents
Anakinra and rilonacept both have an excellent safety profile to date. The most common side effect in AIRTRIP and RHAPSODY was skin reactions at the injection. This occurred in most patients treated with anakinra [24, 25] as well as rilonacept [26, 27•]. It is recommended that patients inject after the solution has come to room temperature to minimize this reaction. Topical corticosteroids and oral antihistamines can provide relief. If patients are educated about these generally self-limited (resolving in up to 2 months) and non-progressive skin reactions, this will set expectations and avoid potential unnecessary discontinuation of therapy.
Infections of skin and upper respiratory system are the second most common reported side effect. Anakinra appears to have a lower risk than rilonacept or canakinumab [26, 27•, 29, 31]. Thus far, these infections have been mild and have not resulted in discontinuation. Laboratory abnormalities, listed in Table 2, are typically not clinically significant. However, based on these lab abnormalities, the measurement of white blood count and transaminases at baseline and 1-, 3-, and 6-month intervals during therapy is recommended. Further lab testing is dictated by clinical events and/or length of therapy. It is important to realize that while the safety profiles of anakinra and rilonacept appear excellent, a relatively small number of patients have received these drugs, especially in the case of rilonacept. Going forward, it will be important to be alert for more serious infections than those already encountered. While there has not been a signal to date, development of cancers is another concern with long-term IL-1 antagonism.
The NLRP3 Inflammasome: a Key Player in Pericarditis
Recent insights into the vital role of the inflammasome in pericarditis further explain the efficacy of the anti-IL-1 therapies we have reviewed. The intense activation of the NLRP3 inflammasome in pericarditis has advanced our understanding of the pathophysiology and most important treatment targets for recurrent pericarditis. The inflammasome is an intracellular complex capable of sensing stress or injury and triggering a systemic inflammatory cascade that starts with the release of the pro-inflammatory cytokine IL-1β (Fig. 1) [21••, 22, 23, 32]; IL-1α is produced locally in damaged tissues. Its role in pericarditis, however, had never been studied in an animal model.
Drs. Stefano Toldo and Adolfo Mauro and colleagues endeavored to meet three goals in their 2021 preclinical research publication: determine if the inflammasome was detectable in human pericarditis, develop a mouse model of pericarditis through activation of the inflammasome, and determine if the inflammasome itself or IL-1α/β would be suitable treatment targets in pericarditis [23].
To accomplish the first goal, pericardial tissue samples from patients with chronic pericarditis who were experiencing a flare and undergoing pericardiectomy for constriction were compared to control tissue from autopsied patients without a history of pericardial disease. Expression of the NLRP3 inflammasome, using its scaffold ASC as a surrogate, was detected in all pericarditis samples. A mouse model of pericarditis was then undertaken and found to share common features of inflammation in the pericardium to those observed in human pericarditis cases. Various treatment strategies were undertaken in the mice. Ibuprofen, a COX-2 (cyclooxygenase 2) inhibitor, reduced pericardial effusion size but did not prevent pericardial thickening or expression of the inflammasome scaffold (i.e., formation of the inflammasome). Colchicine, which is already a cornerstone in treatment of acute and chronic pericarditis, and more recently shown to inhibit the NLRP3 inflammasome (Fig. 1) [33], significantly reduced formation of the NLRP3 inflammasome components by day 7 of treatment [23].
The effects of IL-1 blockade were studied initially with anakinra, a blocker of cytokines IL-1β and IL-1α. This was followed by use of the IL-1β and IL-1α trap (i.e., rilonacept) which prevents these cytokines from binding with their receptor. Both anti-IL-1 therapies demonstrated significant reduction in pericardial effusion, pericardial thickening, and formation of the inflammasome as measured by ASC aggregates. Anakinra reduced pericardial effusion by 13% compared to control, pericardial thickening was diminished by 20%, and the presence of the inflammasome was reduced by 75%. The IL-1 trap was studied at 3 separate doses and reduced pericardial effusion by 33–43% depending on dose administered, decreased pericardial thickening by 36–44%, and reduced presence of the inflammasome by 69–96%. This important study was the first to describe the presence and activation of the NLRP3 inflammasome in human pericardial tissue and characterize effective treatment targets. It also offered tissue-specific, cellular-level explanations for these findings.
Case Conclusion
In view of multiple recurrences requiring corticosteroid therapy, the patient was an excellent candidate for IL-1-directed therapy. He was placed on rilonacept 320 mg s.c. followed by a 160 mg maintenance dose with resolution of chest pain and dyspnea over 2–3 days. His hs-CRP normalized, and he has had no recurrence of symptoms during the first 3 months of therapy.
Treatment Algorithm for Recurrent Idiopathic Pericarditis
The current treatment algorithm for recurrent pericarditis includes NSAIDs and colchicine (first-line therapy) with prednisone (2nd-line therapy) or the combination of 1st- and 2nd-line therapies held in reserve. Pericardiectomy is a “last resort,” 4th line option of uncertain efficacy. As shown in Fig. 2, future modification of the algorithm could include anti-IL-1 therapy after an initial episode of acute pericarditis to potentially reduce any recurrences or after a first recurrence or second recurrence. Optimal use of these agents will require additional research.
Pericarditis and Recurrent Pericarditis in COVID-19 and COVID-19 Vaccination
Both pericarditis and myocarditis, alone and in combination, have been reported during and after COVID-19 infection as well as after vaccination. Post vaccination pericarditis/myocarditis is rare and tends to occur in younger males [35,36,37,38,39,40,41,42,43]. Protection from acute infection and/or reduction in the severity of breakthrough infections with approved vaccines has been very well-documented in the scientific literature. Although we will undoubtedly continue to learn about variabilities in the pathophysiology and course of COVID-19 associated pericarditis, current data suggest that standard treatments for pericarditis and recurrent idiopathic pericarditis, as well as anti-IL-1 agents, remain safe and effective in this population [44].
Conclusions
The past 5–10 years have heralded significant advances in our understanding of the mechanistic role of the NLRP3 inflammasome and IL-1 as a cause of the auto-inflammatory syndrome of recurrent idiopathic pericarditis. Biologics targeting IL-1, such as anakinra and rilonacept, have shown great promise in treating this difficult problem and reducing the need for other anti-inflammatory drugs, which very likely carry more significant side effects.
Several questions remain. How long should anti-IL-1 agents be administered and how should they be discontinued? Will more serious side effects surface as more patients are treated for longer periods of time? To what extent should IL-1 directed therapy supplant the use of corticosteroids and other anti-inflammatory agents? Is IL-1 activation a mechanism underlying initial episodes of acute idiopathic pericarditis, in contrast to the conventional wisdom that most cases have a viral etiology?
Undoubtedly, answers to these and other questions will be forthcoming as more experience is gained. The development and use of anti-IL-1 therapy for recurrent idiopathic pericarditis is yet another example of the success of modern approaches to understanding the molecular basis of disease and the ability to target therapy appropriately.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Imazio M, Gaita F, LeWinter M. Evaluation and treatment of pericarditis: a systematic review. JAMA. 2015;314(14):1498–506.
Adler Y, Charron P. The 2015 ESC Guidelines on the diagnosis and management of pericardial diseases. Eur Heart J. 2015;36(42):2873–4.
Imazio M. Contemporary management of pericardial diseases. Curr Opin Cardiol. 2012;27(3):308–17.
Imazio M, et al. Controversial issues in the management of pericardial diseases. Circulation. 2010;121(7):916–28.
Imazio M, Gaita F. Diagnosis and treatment of pericarditis. Heart. 2015;101(14):1159–68.
Imazio M, et al. Colchicine in addition to conventional therapy for acute pericarditis: results of the COlchicine for acute PEricarditis (COPE) trial. Circulation. 2005;112(13):2012–6.
Imazio M, et al. Colchicine as first-choice therapy for recurrent pericarditis: results of the CORE (COlchicine for REcurrent pericarditis) trial. Arch Intern Med. 2005;165(17):1987–91.
Imazio M, et al. Colchicine for recurrent pericarditis (CORP): a randomized trial. Ann Intern Med. 2011;155(7):409–14.
Imazio M, et al. Efficacy and safety of colchicine for treatment of multiple recurrences of pericarditis (CORP-2): a multicentre, double-blind, placebo-controlled, randomised trial. Lancet. 2014;383(9936):2232–7.
Lotrionte M, et al. International collaborative systematic review of controlled clinical trials on pharmacologic treatments for acute pericarditis and its recurrences. Am Heart J. 2010;160(4):662–70.
Kilbourne ED, Wilson CB, Perrier D. The induction of gross myocardial lesions by a Coxsackie (pleurodynia) virus and cortisone. J Clin Invest. 1956;35(4):362–70.
Imazio M, et al. Prevalence of C-reactive protein elevation and time course of normalization in acute pericarditis: implications for the diagnosis, therapy, and prognosis of pericarditis. Circulation. 2011;123(10):1092–7.
Imazio M, et al. A randomized trial of colchicine for acute pericarditis. N Engl J Med. 2013;369(16):1522–8.
Cremer PC, et al. Complicated pericarditis: understanding risk factors and pathophysiology to inform imaging and treatment. J Am Coll Cardiol. 2016;68(21):2311–28.
• Klein A, et al. US database study of clinical burden and unmet need in recurrent pericarditis. J Am Heart Assoc. 2021;10(15): e018950. This offered the most up-to-date discussion of the course and clinical burden of recurrent pericarditis.
Vianello F, et al. Azathioprine in isolated recurrent pericarditis: a single centre experience. Int J Cardiol. 2011;147(3):477–8.
Peiffer-Smadja N, et al. Corticosteroids and immunosuppressive agents for idiopathic recurrent pericarditis. Autoimmun Rev. 2019;18(6):621–6.
Moretti M, et al. Usefulness of high-dose intravenous human immunoglobulins treatment for refractory recurrent pericarditis. Am J Cardiol. 2013;112(9):1493–8.
Tutar HE, et al. Isolated recurrent pericarditis in a patient with familial Mediterranean fever. Eur J Pediatr. 2001;160(4):264–5.
Vassilopoulos D, et al. Successful treatment of adult patients with idiopathic recurrent pericarditis with an interleukin-1 receptor antagonist (anakinra). Int J Cardiol. 2012;160(1):66–8.
•• Toldo S, Abbate A. The NLRP3 inflammasome in acute myocardial infarction. Nat Rev Cardiol. 2018;15(4):203–14. Findings from this study delineated the role of the inflammasome in pericarditis as well as successful treatment using IL-1-directed therapies.
Mauro AG, et al. NLRP3 inflammasome in acute myocardial infarction. J Cardiovasc Pharmacol. 2019;74(3):175–87.
Mauro AG, et al. The role of NLRP3 inflammasome in pericarditis: potential for therapeutic approaches. JACC Basic Transl Sci. 2021;6(2):137–50.
Brucato A, et al. Effect of anakinra on recurrent pericarditis among patients with colchicine resistance and corticosteroid dependence: the AIRTRIP randomized clinical trial. JAMA. 2016;316(18):1906–12.
Imazio M, et al. Anakinra for corticosteroid-dependent and colchicine-resistant pericarditis: the IRAP (International Registry of Anakinra for Pericarditis) study. Eur J Prev Cardiol. 2020;27(9):956–64.
Klein AL, et al. Efficacy and safety of rilonacept for recurrent pericarditis: results from a phase II clinical trial. Heart, 2020.
• Klein AL, et al. Phase 3 trial of interleukin-1 trap rilonacept in recurrent pericarditis. N Engl J Med. 2021;384(1):31–41. This study demonstrated the safety and recommended monitoring for IL-1-directed therapy.
Shah SR, et al. Canakinumab and cardiovascular outcomes: results of the CANTOS trial. J Community Hosp Intern Med Perspect. 2018;8(1):21–2.
Kougkas N, et al. Canakinumab for recurrent rheumatic disease associated-pericarditis: a case series with long-term follow-up. Rheumatology (Oxford). 2018;57(8):1494–5.
Signa S, et al. Failure of anti interleukin-1 beta monoclonal antibody in the treatment of recurrent pericarditis in two children. Pediatr Rheumatol Online J. 2020;18(1):51.
Andreis A, et al. Anakinra for constrictive pericarditis associated with incessant or recurrent pericarditis. Heart. 2020;106(20):1561–5.
Imazio M, Gaita F. Acute and recurrent pericarditis. Cardiol Clin. 2017;35(4):505–13.
Bayes-Genis A, et al. Colchicine in pericarditis. Eur Heart J. 2017;38(22):1706–9.
Chiabrando JG, et al. Management of acute and recurrent pericarditis: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75(1):76–92.
Foltran D, et al. Myocarditis and pericarditis in adolescents after first and second doses of mRNA COVID-19 Vaccines. Eur Heart J Qual Care Clin Outcomes, 2021.
Istampoulouoglou I, et al. Myocarditis and pericarditis in association with COVID-19 mRNA-vaccination: cases from a regional pharmacovigilance centre. Glob Cardiol Sci Pract. 2021;2021(3): e202118.
Lamprinos N, et al. Pericarditis following recovery from COVID-19 infection in a 15-year-old boy: a postinflammatory immune-mediated presentation or a new-onset autoimmune disease. Cureus. 2021;13(11): e19255.
Lazaros G, et al. A case series of acute pericarditis following COVID-19 vaccination in the context of recent reports from Europe and the United States. Vaccine. 2021;39(45):6585–90.
Li M, et al. Myocarditis and pericarditis following COVID-19 vaccination: inequalities in age and vaccine types. J Pers Med. 2021;11(11).
Ghosh S, et al. COVID-19 presenting as acute pericarditis. BMJ Case Rep. 2022;15(1).
Mormile R. Myocarditis and pericarditis following mRNA COVID-19 vaccination in younger patients: is there a shared thread? Expert Rev Cardiovasc Ther. 2022;1–4.
Patone M, et al. Risks of myocarditis, pericarditis, and cardiac arrhythmias associated with COVID-19 vaccination or SARS-CoV-2 infection. Nat Med. 2022;28(2):410–22.
Yap J, et al. Pericarditis and myocarditis after COVID-19 mRNA vaccination in a nationwide setting. Ann Acad Med Singap. 2022;51(2):96–100.
Imazio M, et al. Anti-inflammatory therapies for pericardial diseases in the COVID-19 pandemic: safety and potentiality. J Cardiovasc Med (Hagerstown). 2020;21(9):625–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. LeWinter is a paid consultant for Kiniksa Pharmaceuticals. The other authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
Dr. LeWinter was an investigator for the Phase 3 Trial of Rilonacept (RHAPSODY; reference #27).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pericardial Disease
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hagerty, T., Kluge, M.A. & LeWinter, M.M. Recurrent Pericarditis: a Stubborn Opponent Meets New Treatments in 2022. Curr Cardiol Rep 24, 915–923 (2022). https://doi.org/10.1007/s11886-022-01719-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-022-01719-z