Abstract
Purpose of Review
Current hypertension guidelines do not provide recommendation on when-to-treat. Herein, we review the current evidence on ingestion-time differences of hypertension medications in blood pressure (BP)–lowering effects and prevention of cardiovascular disease (CVD) events.
Recent Findings
The vast (81.6%) majority of the 136 published short-term treatment-time trials document benefits, including enhanced reduction of asleep BP and increased sleep-time relative BP decline (dipping), when hypertension medications and their combinations are ingested before sleep rather than upon waking. Long-term outcome trials further document bedtime hypertension therapy markedly reduces risk of major CVD events. The inability of the very small 18.4% of the published trials to substantiate treatment-time difference in effects is mostly explained by deficiencies of study design and conduct.
Summary
Our comprehensive review of the published literature reveals no single study has reported better benefits of the still conventional, yet scientifically unjustified, morning than bedtime hypertension treatment scheme.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hermida RC, Ayala DE, Calvo C, Portaluppi F, Smolensky MH. Chronotherapy of hypertension: administration-time dependent effects of treatment on the circadian pattern of blood pressure. Adv Drug Deliv Rev. 2007;59:923–39.
Smolensky MH, Hermida RC, Ayala DE, Tiseo R, Portaluppi F. Administration-time-dependent effect of blood pressure-lowering medications: basis for the chronotherapy of hypertension. Blood Press Monit. 2010;15:173–80.
Hermida RC, Ayala DE, Fernández JR, Portaluppi F, Fabbian F, Smolensky MH. Circadian rhythms in blood pressure regulation and optimization of hypertension treatment with ACE inhibitor and ARB medications. Am J Hypertens. 2011;24:383–91.
Zhao P, Xu P, Wan C, Wang Z. Evening versus morning dosing regimen drug therapy for hypertension. Cochrane Database Syst Rev. 2011;10:CD004184.
De Giorgi A, Menegatti AM, Fabbian F, Portaluppi F, Manfredini R. Circadian rhythms and medical diseases: does it matter when drugs are taken? Eur J Intern Med. 2013;24:698–706.
Hermida RC, Ayala DE, Fernández JR, Mojón A, Smolensky MH, Fabbian F, et al. Administration-time-differences in effects of hypertension medications on ambulatory blood pressure regulation. Chronobiol Int. 2013;30:280–314.
Liu X, Liu X, Huang W, Leo S, Li Y, Liu M, et al. Evening – versus morning – dosing drug therapy for chronic kidney disease patients with hypertension: a systematic review. Kidney Blood Press Res. 2014;39:427–40.
Schillaci G, Battista F, Settimi L, Schillaci L, Pucci G. Antihypertensive drug treatment and circadian blood pressure rhythm: a review of the role of chronotherapy in hypertension. Curr Pharm Des. 2015;21:756–72.
• Smolensky MH, Hermida RC, Ayala DE, Portaluppi F. Bedtime hypertension chronotherapy: concepts and patient outcomes. Curr Pharm Des. 2015;21:773–90 This publication reviews the main principles and concepts of chronopharmacology and chronotherapy of hypertension and summarizes the differential reduction of awake and asleep SBP/DBP means by upon-awakening versus at-bedtime ingestion of conventional BP-lowering medications.
Stranges PM, Drew AM, Rafferty P, Shuster JE, Brooks AD. Treatment of hypertension with chronotherapy: is it time? Ann Pharmacother. 2015;49:323–34.
Hermida RC, Ayala DE, Smolensky MH, Fernández JR, Mojón A, Portaluppi F. Chronotherapy with conventional blood pressure medications improves management of hypertension and reduces cardiovascular and stroke risks. Hypertens Res. 2016;39:277–92.
Sun Y, Yu X, Liu J, Zhou N, Chen L, Zhao Y, et al. Effect of bedtime administration of blood-pressure lowering agents on ambulatory blood pressure monitoring results: a meta-analysis. Cardiol J. 2016;23:473–81.
Hermida RC, Ayala DE, Fernández JR, Mojón A, Crespo C, Ríos MT, et al. Bedtime blood pressure chronotherapy significantly improves hypertension management. Heart Fail Clin. 2017;13:759–73.
Bowles NP, Thosar SS, Herzig MX, Shea SA. Chronotherapy for hypertension. Curr Hypertens Rep. 2018;20:97.
Hermida RC, Ayala DE, Mojón A, Fernández JR. Influence of circadian time of hypertension treatment on cardiovascular risk: results of the MAPEC study. Chronobiol Int. 2010;27:1629–51.
• Roush GC, Fapohunda J, Kostis JB. Evening dosing of antihypertensive therapy to reduce cardiovascular events: a third type of evidence based on a systematic review and meta-analysis of randomized trials. J Clin Hypertens (Greenwich). 2014;16:561–8 This publication is a comprehensive meta-analysis verifying attenuation of CVD events is substantially improved when hypertension medications are consistently ingested in the evening/bedtime rather than morning/upon-awakening.
Sobiczewski W, Wirthwein M, Gruchala M, Kocic I. Mortality in hypertensive patients with coronary heart disease depends on chronopharmacotherapy and dipping status. Pharmacol Rep. 2014;66:448–52.
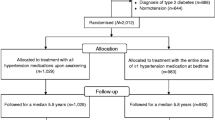
•• Hermida RC, Crespo JJ, Domínguez-Sardiña M, Otero A, Moyá A, Ríos MT, et al. Bedtime hypertension treatment improves cardiovascular risk reduction: the Hygia Chronotherapy Trial. Eur Heart J. 2019. https://doi.org/10.1093/eurheartj/ehz754This publication reports major findings of the Hygia Chronotherapy Trial, the so far largest randomized trial conducted at the primary care setting, documenting routine ingestion by hypertensive patients of ≥ 1 prescribed BP-lowering medications at bedtime, as opposed to upon-waking, results in improved ambulatory BP control and, most importantly, markedly diminished occurrence of major CVD events.
Gupta R, Malik AH, Popli T, Ranchal P, Yandrapalli S, Aronow WS. Impact of bedtime dosing of antihypertensives compared to morning therapy: a meta-analysis of randomised controlled trials. Eur J Prev Cardiol. 2020 Feb 3:204748732090361. https://doi.org/10.1177/2047487320903611.
National Institute for Health and Clinical Excellence. Hypertension: The clinical management of primary hypertension in adults. NICE Clinical Guidelines 127: Methods, evidence and recommendations. National Clinical Guidelines Centre, London, UK. 2011. http://guidance.nice.org.uk/CG/Wave2/14 (accessed 27 May 2020).
Chiang CE, Wang TD, Ueng KC, Lin TH, Yeh HI, Chen CY, et al. 2015 guidelines of the Taiwan Society of Cardiology and the Taiwan Hypertension Society for the Management of Hypertension. J Chin Med Assoc. 2015;78:1–47.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Himmerfarb CD, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:e127–248.
Williams B, Mancia G, Spiering W, Rosei EA, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur Heart J. 2018;39:3021–104.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Rabi DM, McBrien KA, Sapir-Pichhadze R, Nakhla M, Ahmed SB, Dumanski SM, et al. Hypertension Canada’s 2020 comprehensive guidelines for the prevention, diagnosis, risk assessment, and treatment of hypertension in adults and children. Can J Cardiol. 2020;36:596–624.
Ohkubo T, Hozawa A, Yamaguchi J, Kikuya M, Ohmori K, Michimata M, et al. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study. J Hypertens. 2002;20:2183–9.
Dolan E, Stanton A, Thijs L, Hinedi K, Atkins N, McClory S, et al. Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: the Dublin outcome study. Hypertension. 2005;46:156–61.
Ben-Dov IZ, Kark JD, Ben-Ishay D, Mekler J, Ben-Arie L, Bursztyn M. Predictors of all-cause mortality in clinical ambulatory monitoring. Unique aspects of blood pressure during sleep. Hypertension. 2007;49:1235–41.
Boggia J, Li Y, Thijs L, Hansen TW, Kikuya M, Björklund-Bodegård K, et al. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet. 2007;370:1219–29.
Fagard RH, Celis H, Thijs L, Staessen JA, Clement DL, De Buyzere ML, et al. Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension. 2008;51:55–61.
Fan HQ, Li Y, Thijs L, Hansen TW, Boggia J, Kikuya M, et al. Prognostic value of isolated nocturnal hypertension on ambulatory measurement in 8711 individuals from 10 populations. J Hypertens. 2010;28:2036–45.
Hermida RC, Ayala DE, Mojón A, Fernández JR. Decreasing sleep-time blood pressure determined by ambulatory monitoring reduces cardiovascular risk. J Am Coll Cardiol. 2011;58:1165–73.
Minutolo R, Agarwal R, Borrelli S, Chiodini P, Bellizzi V, Nappi F, et al. Prognostic role of ambulatory blood pressure measurement in patients with nondialysis chronic kidney disease. Arch Intern Med. 2011;171:1090–8.
Hermida RC, Ayala DE, Mojón A, Fernández JR. Blunted sleep-time relative blood pressure decline increases cardiovascular risk independent of blood pressure level – the “normotensive non-dipper” paradox. Chronobiol Int. 2013;30:87–98.
• Roush GC, Fagard RH, Salles GF, Pierdomenico SD, Reboldi G, Verdecchia P, et al. Prognostic impact from clinic, daytime, and nighttime systolic blood pressure in 9 cohorts on 13,844 patients with hypertension. J Hypertens. 2014;32:2332–40 This publication reports the meta-analysis of original data of nine hypertensive cohorts describing the asleep SBP mean as the best predictor of CVD events, independent of daytime OBPM or awake and 24h ABP means.
• Salles GF, Reboldi G, Fagard RH, Cardoso C, Pierdomenico SD, Verdecchia P, et al. Prognostic impact of the nocturnal blood pressure fall in hypertensive patients: The ambulatory blood pressure collaboration in patients with hypertension (ABC-H) meta-analysis. Hypertension. 2016;67:693–700 This publication reports the meta-analysis of original data of 17,312 hypertensive patients describing the significant prognostic value of sleep-time relative BP decline (BP dipping) as marker of CVD risk.
•• Hermida RC, Crespo JJ, Otero A, Domínguez-Sardiña M, Moyá A, Ríos MT, et al. Asleep blood pressure: Significant prognostic marker of vascular risk and therapeutic target for prevention. Eur Heart J. 2018;39:4159–71 This publication reports major findings of the large cohort primary care–based multicenter Hygia Project verifying the asleep SBP mean and sleep-time SBP relative decline are jointly the two most sensitive ABPM-derived variables predictive of CVD risk as well as novel BP targets for prevention.
Hermida RC, Ayala DE, Portaluppi F. Circadian variation of blood pressure: the basis for the chronotherapy of hypertension. Adv Drug Deliv Rev. 2007;59:904–22.
Smolensky MH, Hermida RC, Castriotta RJ, Portaluppi F. Role of sleep-wake cycle on blood pressure circadian rhythms and hypertension. Sleep Med. 2007;8:668–80.
Portaluppi F, Tiseo R, Smolensky MH, Hermida RC, Ayala DE, Fabbian F. Circadian rhythms and cardiovascular health. Sleep Med Rev. 2012;16:151–66.
Fabbian F, Smolensky MH, Tiseo R, Pala M, Manfredini R, Portaluppi F. Dipper and non-dipper blood pressure 24-hour patterns: circadian rhythm-dependent physiologic and pathophysiologic mechanisms. Chronobiol Int. 2013;30:17–30.
• Smolensky MH, Hermida RC, Portaluppi F. Circadian mechanisms of 24-hour blood pressure regulation and patterning. Sleep Med Rev. 2017;33:4–16 This publication constitutes a recent extensive review of the broad range of endogenous circadian rhythms and ambient environmental cyclic influences that are mechanistic of the 24-h BP pattern.
Angeli A, Gatti G, Masera R. Chronobiology of the hypothalamic-pituitary-adrenal and renin-angiotensin-aldosterone systems. In: Touitou Y, Haus E, editors. Biologic rhythms in clinical and laboratory medicine. Berlin: Springer-Verlag; 1992. p. 292–314.
Sothern RB, Vesely DL, Kanabrocki EL, Hermida RC, Bremner FW, Third JLHC, et al. Temporal (circadian) and functional relationship between atrial natriuretic peptides and blood pressure. Chronobiol Int. 1995;12:106–20.
Hermida RC, Smolensky MH, Ayala DE, Portaluppi F, Crespo JJ, Fabbian F, et al. ambulatory blood pressure monitoring recommendations for the diagnosis of adult hypertension, assessment of cardiovascular and other hypertension-associated risk, and attainment of therapeutic goals. Joint recommendations from the International Society for Chronobiology (ISC), American Association of Medical Chronobiology and Chronotherapeutics (AAMCC), Spanish Society of Applied Chronobiology, Chronotherapy, and Vascular Risk (SECAC), Spanish Society of Atherosclerosis (SEA), and Romanian Society of Internal Medicine (RSIM). Chronobiol Int. 2013;30:355–410.
Verdecchia P, Porcellati C, Schillaci G, Borgioni C, Ciucci A, Battistell M, et al. Ambulatory blood pressure: an independent predictor of prognosis in essential hypertension. Hypertension. 1994;24:793–801.
Clement DL, De Buyzere ML, De Bacquer DA, de Leeuw PW, Duprez DA, Fagard RH, et al. Prognostic value of ambulatory blood-pressure recordings in patients with treated hypertension. N Engl J Med. 2003;348:2407–15.
Eguchi K, Pickering TG, Hoshide S, Ishikawa J, Ishikawa S, Schwartz J, et al. Ambulatory blood pressure is a better marker than clinic blood pressure in predicting cardiovascular events in patients with/without type 2 diabetes. Am J Hypertens. 2008;21:443–50.
Salles GF, Cardoso CR, Muxfeldt ES. Prognostic influence of office and ambulatory blood pressures in resistant hypertension. Arch Intern Med. 2008;168:2340–6.
Frank M, Peyrard S, Bobrie G, Azizi M. Method of mean value calculation as an additional source of variability in ambulatory blood pressure measurement. Am J Hypertens. 2010;23:725–31.
Hermida RC, Calvo C, Ayala DE, Fernández JR, Ruilope LM, López JE. Evaluation of the extent and duration of the “ABPM effect” in hypertensive patients. J Am Coll Cardiol. 2002;40:710–7.
• Hermida RC, Ayala DE, Fontao MJ, Mojón A, Fernández JR. Ambulatory blood pressure monitoring: Importance of sampling rate and duration – 48 versus 24 hours – on the accurate assessment of cardiovascular risk. Chronobiol Int. 2013;30:55–67 This publication provides in-depth verification the duration of ABPM—48 h vs. 24 h—rather than the frequency of measurement more accurately derives representative awake and asleep SBP and DBP means as well as sleep-time relative BP decline (dipper status) and CVD risk.
Julious SA. Sample sizes for clinical trials with normal data. Stat Med. 2004;23(12):1921–86. https://doi.org/10.1002/sim.1783.
Ciobanu DM, Veresiu IA, Bala CG, Roman G, Mircea PA. Benefits of bedtime hypertension medication in type 2 diabetes demonstrated on ambulatory blood pressure monitoring. 49th Ann Sci Meeting Eur Soc Clin Invest. 2015:107–12.
Huangfu W, Duan P, Xiang D, Gao R. Administration time-dependent effects of combination therapy on ambulatory blood pressure in hypertensive subjects. Int J Clin Exp Med. 2015;8(10):19156–61.
Kasiakogias A, Tsioufis C, Thomopoulos C, Andrikou I, Aragiannis D, Dimitriadis K, et al. Evening versus morning dosing of antihypertensive drugs in hypertensive patients with sleep apnoea: a cross-over study. J Hypertens. 2015;33(2):393–400.
Lafeber M, Grobbee DE, Schrover IM, Thom S, Webster R, Rodgers A, et al. Comparison of a morning polypill, evening polypill and individual pills on LDL-cholesterol, ambulatory blood pressure and adherence in high-risk patients; a randomized crossover trial. Int J Cardiol. 2015;181:193–9.
Ponte-Márquez PH, Solé MJ, Arroyo JA, Matas L, Benet MT, Roca-Cusachs A. Differences in the reduction of blood pressure according to drug administration at activity hours or rest hours. Med Clin (Barc). 2015;144(2):51–4.
Ushijima K, Nakashima H, Shiga T, Harada K, Ishikawa S, Ioka T, et al. Different chronotherapeutic effects of valsartan and olmesartan in non-dipper hypertensive patients during valsartan treatment at morning. J Pharmacol Sci. 2015;127(1):62–8.
Zappe DH, Crikelair N, Kandra A, Palatini P. Time of administration important? Morning versus evening dosing of valsartan. J Hypertens. 2015;33(2):385–92.
Zhu GS. Therapeutic effect of various medication times on anti-hypertension in elderly patients. J Huaihai Med. 2015;33:356–7.
Crippa G, Zabzuni D, Cassi A, Bravi E. Effect of bedtime dosing of barnidipine hydrochloride in non-dipper hypertensive patients with obstructive sleep apnoea not treated with continuous positive airway pressure. Eur Rev Med Pharmacol Sci. 2016;20(2):339–44.
Hjortkjær HØ, Jensen T, Kofoed KF, Mogensen UM, Sigvardsen PE, Køber L, et al. Nocturnal antihypertensive treatment in patients with type 1 diabetes with autonomic neuropathy and non-dipping: a randomised, placebo-controlled, double-blind cross-over trial. BMJ Open. 2016;6(12):e012307.
Hou SF. Effect of levamlopine on elderly non-dipper hypertension at different time. World Clin Med. 2016;10:67–71.
Kario K, Hoshide S, Uchiyama K, Yoshida T, Okazaki O, Noshiro T, et al. Dose timing of an angiotensin II receptor blocker/calcium channel blocker combination in hypertensive patients with paroxysmal atrial fibrillation. J Clin Hypertens (Greenwich). 2016;18(10):1036–44.
Lin YJ, Wu CF. Clinical analysis of the pharmacology of levamlodipine on correcting elderly non-dipper hypertension. Strait Pharmaceut J. 2016;28:95–6.
Fujiwara T, Hoshide S, Yano Y, Kanegae H, Kario K. Comparison of morning vs bedtime administration of the combination of valsartan/amlodipine on nocturnal brachial and central blood pressure in patients with hypertension. J Clin Hypertens (Greenwich). 2017;19(12):1319–26.
Khodadoustan S, Ashrafi IN, Satheesh KV, Kumar C, Hs S, S C. Evaluation of the effect of time dependent dosing on pharmacokinetic and pharmacodynamics of amlodipine in normotensive and hypertensive human subjects. Clin Exp Hypertens 2017;39(6):520–526.
Serinel Y, Yee BJ, Grunstein RR, Wong KH, Cistulli PA, Arima H, et al. Chronotherapy for hypertension in obstructive sleep apnoea (CHOSA): a randomised, double-blind, placebo-controlled crossover trial. Thorax. 2017;72(6):550–8.
Poulter NR, Savoloulos C, Anjum A, Apostolopoulou M, Chapman N, Cross M, et al. Randomized crossover trial of the impact of morning or evening dosing of antihypertensive agents on 24-hour ambulatory blood pressure – the HARMONY trial. Hypertension. 2018;72:870–3.
Kuate LM, Ondoa HOB, Jean-Claude K, Tankeu AT, Bokam MCA, Bimbai AM, et al. Effects of morning versus evening administration of perindopril on the circadian control of blood pressure in Cameroonian type 2 diabetes individuals: a crossover randomized trial. Int Arch Cardiovasc Dis. 2019;3:014.
Sellén-Sanchén E, Ferrer-Herrera IM, Coll-Bujardon D. Ambulatory blood pressure monitoring and chronotherapy response in a diabetic hypertensive population. Rev Arch Med Camagüey. 2019;23(6):697–708.
Hermida RC, Calvo C, Ayala DE, López JE. Decrease in urinary albumin excretion associated to the normalization of nocturnal blood pressure in hypertensive subjects. Hypertension. 2005;46:960–8.
Hermida RC, Ayala DE, Mojon A, Fernandez JR. Chronotherapy with nifedipine GITS in hypertensive patients: improved efficacy and safety with bedtime dosing. Am J Hypertens. 2008;21:948–54.
Staessen JA, Fagard R, Thijs L, Celis H, Arabidze GG, Birkenhager WH, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. Lancet. 1997;350:757–64.
Liu L, Wang JG, Gong L, Liu G, Staessen JA. Comparison of active treatment and placebo in older Chinese patients with isolated systolic hypertension. Systolic Hypertension in China (Syst-China) Collaborative Group. J Hypertens. 1998;16:1823–9.
Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients: the Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med. 2000;342:145–53.
Tatti P, Pahor M, Byington RP, Di Mauro P, Guarisco R, Strollo G, et al. Outcome results of the fosinopril versus amlodipine cardiovascular events randomized trial (FACET) in patients with hypertension and NIDDM. Diabetes Care. 1998;21(4):597–603.
Black HR, Elliott WJ, Grandits G, Grambsch P, Lucente T, White WB, et al. Principal results of the Controlled Onset Verapamil Investigation of Cardiovascular End Points (CONVINCE) trial. JAMA. 2003;289:2073–82.
White WB, Black HR, Weber MA, Elliott WJ, Brysinski B, Fakourhi TD. Comparison of effects of controlled-onset extended-release verapamil at bedtime and nifedipine gastrointestinal therapeutic system on arising on early morning blood pressure, heart rate, and the heart rate-blood pressure product. Am J Cardiol. 1998;81:424–31.
Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665.
Carter BL, Chrischilles EA, Rosenthal G, Gryzlak BM, Eisenstein EL, Vander Weg MW. Efficacy and safety of nighttime dosing of antihypertensives: review of the literature and design of a pragmatic clinical trial. J Clin Hypertens (Greenwich). 2014;16:115–21.
Rorie DA, Rogers A, Mackenzie IS, Ford I, Webb DJ, Williams B, et al. Methods of a large prospective, randomized, open-label, blinded end-point study comparing morning versus evening dosing in hypertensive patients: the Treatment In Morning versus Evening (TIME) study. BMJ Open. 2016;6:e010313. https://doi.org/10.1136/bmjopen-2015-010313.
Hermida RC, Mojón A, Fernández JR. Comparing the design of the primary-care based Hygia Chronotherapy Trial and the internet-based TIME study. Eur Heart J. 2020;41:1608.
Kim SYH, Miller FG. Ethical complexities in standard of care randomized trials: a case study of morning versus nighttime docing of blood pressure drugs. Clin Trials. 2015;12:557–63.
Kanabrocki EL, George M, Hermida RC, Messmore HL, Ryan MD, Ayala DE, et al. Day-night variations in blood levels of nitric oxide, T-TFPI and E-selectin. Clin Appl Thrombosis/Hemostasis. 2001;7:339–45.
Sole MJ, Martino TA. Diurnal physiology: core principles with application to the pathogenesis, diagnosis, prevention, and treatment of myocardial hypertrophy and failure. J Appl Physiol. 2009;107:1318–27.
Martino TA, Tata N, Simpson JA, Vanderlaan R, Dawood F, Kabir MG, et al. The primary benefits of angiotensin-converting enzyme inhibition on cardiac remodeling occur during sleep time in murine pressure overload hypertrophy. J Am Coll Cardiol. 2011;57:2020–8.
Rana S, Prabhu SD, Young ME. Chronobiological influence over cardiovascular function. The good, the bad, and ugly. Circ Res. 2020;126:258–79.
Hermida RC, Ayala DE, Mojón A, Fernández JR. Cardiovascular risk of essential hypertension: influence of class, number, and treatment-time regimen of hypertension medications. Chronobiol Int. 2013;30:315–27.
Hermida RC, Crespo JJ, Domínguez-Sardiña M, for the Hygia Chronotherapy Trial investigators. Improved reduction of cardiovascular risk by bedtime ingestion of ARB and ACEI medication class therapies. Eur Heart J. 2020;41:1602–3.
Hermida RC, Ayala DE, Mojón A, Smolensky MH, Fernández JR. Diagnosis and management of hypertension: around-the-clock ambulatory blood pressure monitoring is substantially more effective and less costly than daytime office blood pressure measurements. Chronobiol Int. 2019;36:1515–27.
Hermida RC, Ayala DE, Mojón A, Fernández JR. Influence of time of day of blood pressure-lowering treatment on cardiovascular risk in hypertensive patients with type 2 diabetes. Diabetes Care. 2011;34:1270–6.
Hermida RC, Ayala DE, Mojón A, Fernández JR. Bedtime dosing of antihypertensive medications reduces cardiovascular risk in CKD. J Am Soc Nephrol. 2011;22:2313–21.
Ayala DE, Hermida RC, Mojón A, Fernández JR. Cardiovascular risk of resistant hypertension: dependence on treatment-time regimen of blood pressure-lowering medications. Chronobiol Int. 2013;30:340–52.
• Hermida RC, Ayala DE, Mojón A, Fernández JR. Bedtime ingestion of hypertension medications reduces the risk of new-onset type 2 diabetes: a randomised controlled trial. Diabetologia. 2016;59:255–65 This publication documents risk for new-onset type 2 diabetes can be significantly diminished when the asleep SBP mean is appropriately controlled by bedtime hypertension chronotherapy.
•• Hermida RC, Ayala DE, Mojón A, Fernánez JR. Risk of incident chronic kidney disease is better reduced by bedtime than upon awakening ingestion of hypertension medications. Hypertens Res. 2018;41:342–53 This publication demonstrates bedtime hypertension chronotherapy not only more effectively diminishes asleep SBP mean than upon-awakening treatment, but significantly reduces risk for incident CKD.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All reported studies with human subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional research committee standards, and institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Hypertension
Rights and permissions
About this article
Cite this article
Hermida, R.C., Hermida-Ayala, R.G., Smolensky, M.H. et al. Does Timing of Antihypertensive Medication Dosing Matter?. Curr Cardiol Rep 22, 118 (2020). https://doi.org/10.1007/s11886-020-01353-7
Published:
DOI: https://doi.org/10.1007/s11886-020-01353-7