Abstract
Purpose of Review
This study aims to determine if percutaneous coronary intervention (PCI) does improve survival in stable ischemic heart disease (SIHD).
Recent Findings
The International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial will evaluate patients with moderate to severe ischemia and will be the largest randomized trial of an initial management strategy of coronary revascularization (percutaneous or surgical) versus optimal medical therapy alone for SIHD. Although the ISCHEMIA trial may show a benefit with upfront coronary revascularization in this high-risk population, cardiac events after PCI are largely caused by plaque rupture in segments outside of the original stented segment. Furthermore, given the robust data from prior randomized trials, which showed no survival benefit with PCI, and the likelihood that the highest risk patients in ISCHEMIA will be treated with surgery, it is unlikely that the ISCHEMIA trial will show a survival benefit particular to PCI.
Recent Findings
Although PCI relieves symptoms, the evidence base indicates that it does not prolong survival in SIHD.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: •Of importance ••Of major importance
Boden W, et al. Optimal medical therapy with or without PCI for stables coronary disease. N Engl J Med. 2007;356(15):1503–16.
The BARI 2D Study Group. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med. 2009;360(2503):2515.
•• Sedlis SP, et al. Effect of PCI on long-Tem survival in patients with stable ischemic heart disease. N Engl J Med. 2015;373:1937–46. Long-term follow-up of the COURAGE trial (0-15 year, median 11.9 years) with total of 561 deaths found no difference in survival between OMT and PCI groups.
Shaw L, et al. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy. Circulation. 2008;117(10):1283–91.
Hachamovitch R, et al. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation. 2003;107:2900–7.
www.ischemiatrial.org. Last Accessed 8/17/2016
O’Brien KD, et al. Comparison of apolipoprotein and proteoglycan deposits in human coronary atheroslerotic plaques: colocalization of biglycan with apolipoproteins. Circulation. 1998;98:519–27.
Virmani R, et al. Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler Thromb Vasc Bio. 2000;20(5):1262.
Crisby M, et al. Pravastatin treatment increases collagen content and decreases lipid content, inflammation, metalloproteinases, and cell death in human carotid plaques: implications for plaque stabilization. Circulation. 2001;103(7):926.
Stone GW, et al. Prospect study: a prospective natural-history study of coronary atherosclerosis. PROSPECT investigator. N Engl J Med. 2011;364(3):226.
Ambrose JA, et al. Angiographic progression of coronary artery disease and the development of myocardial infarction. J Am Coll Cardiol. 1988;12(1):56–62.
Little WC, et al. Can coronary angiography predict the site of a subsequent myocardial infarction in patients with mild-to-moderate coronary artery disease? Circulation. 1988;78(5 Pt 1):1157–66.
Mancini GBJ, et al. Angiographic disease progression and residual risk of cardiovascular events while on optimal medical therapy: observations from the COURAGE trial. Circ Card Int. 2011;4(6):545–52.
The Veterans Administration Coronary Artery Bypass Surgery Cooperative Study Group. Eleven year survival in the veterans administration randomized trial of coronary bypass surgery for stable angina. N Engl J Med. 1984;311:1333–9.
European Coronary Surgery Study Group. Long-term results of a prospective randomised trial of coronary artery bypass surgery in stable angina pectoris. Lancet. 982;1173–1180
Chaitman BR, et al. Coronary Artery Surgery Study (CASS): comparability of 10 year survival in randomized and randomizable patients. J Am Coll Cardiol. 1990;16:1071–8.
CASS Principal Investigators and Their Associates. Coronary Artery Surgery (CASS): a randomized trial of coronary artery bypass surgery. Survival data. Circulation. 1983;68:939–50.
Rihal CS, Raco DL, Gersh BJ, Yusuf S. Indications for coronary artery bypass surgery and percutaneous coronary intervention in chronic stable angina: review of the evidence and methodological considerations. Circulation 2003;108:2439–2445.
• Garcia S, et al. Outcomes after complete versus incomplete revascularization of patients with multivessel coronary artery disease: a meta-analysis of 89,883 patients enrolled in randomized clinical trials and observational studies. J Am Coll Cardiol. 2013;62(16):1421–31. Meta-analysis of 35 studies including 89,883 patients which compares complete revascularization versus incomplete revascularization by CABG or PCI in patients with multivessel CAD. Approximately half of the two groups received complete revascularization and the other half received incomplete revascularization. Most patients that were revascularized by CABG achieved complete versus those that were revascularized by PCI.
Hannan EL, et al. Drug-eluting stents vs coronary-artery bypass grafting in multivessel coronary disease. N Engl J Med. 2008;358:331–4.
Weintraub WS, et al. Comparative effectiveness of revascularization strategies. N Engl J Med. 2012;366:1467–76.
BARI investigators. The final 10-year follow-up results from the BARI randomized trial. J Am Coll Cardiol. 2007;49(15):1600–6.
Farkouh ME, et al. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med. 2012;367:2375–84.
• Mohr FW, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5 year follow-up of the randomized, clinical SYNTAX trial. Lancet. 2013;381(9867):629–38. Report of the 5 year follow-up of the SYNTAX trial, compared CABG with PCI for the treatment in patients with left main coronary disease or three vessel disease. This multicentered trial of 1800 patients randomly assigned patients to either CABG group or PCI group. After 5 year follow it was found that major adverse cardiac and cerebrovascular events were lower in the CABG versus the PCI group (26.9% vs 37.3%). This study determined that CABG should remain the standard of care in patients with complex lesions, determined by high or intermediate SYNTAX scores. For patients with low SYNTAX scores PCI was determined to be an acceptable alternative.
• Sipahi I, et al. Coronary artery bypass grafting vs percutaneous coronary intervention and long-term mortality and morbidity in multivessel disease. JAMA Intern Med. 2014;174(2):223–30. Meta-analysis of 6 randomized trials totaling 6055 patients set out to determine the comparative effects of CABG vs PCI on long term mortality and morbidity in patient with multivessel disease. This study concluded that in patients with multivessel disease, CABG compared to PCI results in a reduction in long-term mortality and myocardial infarction.
RITA-2 participants. Coronary angioplasty versus medical therapy for angina: the second Randomised Intervention Treatment of Angina (RITA-2) trial. Lancet. 1997;350(9076):461–8.
Folland ED, et al. Percuatneous transluminal coronary angioplasty versus medical therapy for stable angina pectoris: outcomes for patients with double-vessel versus single-vessel coronary artery disease in a Veterans Affairs Cooperative randomized trial. J Am Coll Cardiol. 1997;29(7):1505–11.
Pitt B, et al. Aggressive lipid-lowering therapy compared with angioplasty in stable coronary artery disease. N Engl J Med. 1999;341:70–6.
Henderson RA, et al. Second Randomized Intervention Treatment of Angina (RITA-2) trial participants. Seven-year outcome in the RITA-2 trial: coronary angioplasty versus medical therapy. J Am Coll Cardiol. 2003;42(7):1161–70.
Hartigan PM, Giacomini JC, Folland ED, Parisi AF. Two to three year follow-up of patients with single-vessel coronary artery disease randomized to PTCA or medical therapy (results of a VA cooperative study). Am J Cardiol. 1998;82(12):1445–50.
Tonino PA, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360:213–24.
Pijls NH, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary disease; 2 year follow up of the FAME study. J Am Coll Cardiol. 2010;56:177–84.
De Bruyne B, Pijls NHJ, Kalesan B, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med 2012;367:991–1001.
Sedlis SP, et al. Percutaneous coronary intervention: FAME is lasting. Lancet. 2015;386(10006):1806–7.
Bangalore S, et al. Short and long term outcomes with drug-eluting and bare metal coronary stents: a mixed treatment comparison analysis of 117 762 patients years of follow up from randomized trials. Circulation. 2012;125(23):2873.
Applegate RJ, et al. Long term ( three year) safety and efficacy of everolimus-eluting stents compared to paclitaxel- eluting stents ( from the SPIRIT III Trial). Am J Cardiol. 2011;107(6):833–40.
• Windecker S, Stortecky S, Juni P. Revascularisation versus medical treatment in patients with stable coronary artery disease: network meta-analysis. BMJ. 2014;348:3859. Meta-analysis of 100 trials totaling 93,553 which compares whether revascularization improves prognosis compared to medical treatment among patients with stable coronary artery disease. Among the patients with stable CAD, it was found that CABG reduces the risk of death, MI and revascularization compared to medical treatment.
Bonaa KH, Mannsverk J, Wiseth, R. et al, Drug-eluting or bare-metal stents for coronary artery disease. N Engl J Med. 2016;375:1242–1252.
M Emond, M.B Mock, K.B Davis, et al. Long-term survival of medically treated patients in the Coronary Artery Surgery Study (CASS) Registry. Circulation. 1994;90:2645–2657
Takaro T, Peduzzi P, Detre KM, et al. Survival in subgroups of patients with left main coronary artery disease. Veterans Administration Cooperative Study of Surgery for Coronary Arterial Occlusive Disease. Circulation. 1982;66:14–22.
Chaitman BR, et al. Effect of coronary bypass surgery on survival patterns in subsets of patients with left main coronary artery disease. Report of the Collaborative Study in Coronary Artery Surgery (CASS). Am J Cardiol. 1981;48(4):765.
Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/ American Heart Association Task Force on Practice Guidelines, and the American Collegge of Physicians, American Association for Thoracic Surgery, Preventative Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2012; 126:e354–471.
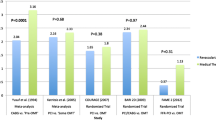
•• Gada H, et al. Meta-analysis of trials on mortality after percutaneous coronary intervention compared with medical therapy in patients with stable coronary heart disease and objective evidence of myocardial ischemia. Am J Cardiol. 2015;115(9):1194–9. Meta-analysis of 3 randomized clinical trials totaling 1,557 patients comparing PCI with OMT in patients with documented myocardial ischemia set out to find out if those with objective ischemia would benefit from PCI versus OMT alone. PCI with OMT compared to OMT alone was associated with a reduction in mortality in RCTs that enrolled patients with objective evidence of ischemia using noninvasive stress imaging or abnormal FFR. In PCI plus MT versus MT alone 3.0% versus 5.9% of the patients died. In the analysis of pooled HR, a significant reduction in all-cause mortality was 0.52.
Velazquez EJ, et al. Long-term survival of patients with ischemic cardiomyopathy treated by coronary artery bypass grafting versus medical therapy. Ann Thorac Surg. 2012;93:523–30.
O’Connor CM, et al. Comparison of coronary artery bypass grafting versus medical therapy on long-term outcome in patients with ischemic cardiomyopathy (a 25-year experience from the Duke Cardiovascular Disease Databank). Am J Cardiol. 2002;90:101–7.
Velazquez EJ, for the STICH Investigators, et al. Coronary-artery bypass surgery in patients with left ventricular dysfunction. N Engl J Med. 2011;364:1607–16.
Velasquez EJ, et al. Coronary-artery bypass surgery in patients with ischemic cardiomyopathy. N Engl J Med. 2016;374:1511–20.
Shaw LJ, et al. Baseline stress myocardial perfusion imaging results and outcomes in patients with stable ischemic heart disease randomized to optimal medical therapy with or without percutaneous coronary intervention. Am Heart J. 2012;164:243–50.
Moroi M, et al. Coronary revascularization does not decrease cardiac events in patients with stable ischemic heart disease but might do in those who showed moderate to severe ischemia. Int J Cardiol. 2012;158:246–52.
Acknowledgments
Binita Shah was supported in part by the Biomedical Laboratory Research & Development Service of the VA Office of Research and Development (I01BX007080).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Francisco Ujueta, Ephraim N. Weiss, Binita Shah, and Steven P. Sedlis declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Ischemic Heart Disease
Rights and permissions
About this article
Cite this article
Ujueta, F., Weiss, E.N., Shah, B. et al. Effect of Percutaneous Coronary Intervention on Survival in Patients with Stable Ischemic Heart Disease. Curr Cardiol Rep 19, 17 (2017). https://doi.org/10.1007/s11886-017-0821-6
Published:
DOI: https://doi.org/10.1007/s11886-017-0821-6