Opinion statement
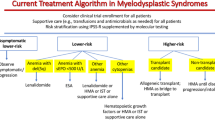
The treatment of myelodysplastic syndromes (MDS) begins with risk stratification using a validated tool such as the International Prognostic Scoring System (IPSS) or its revised version (IPSS-R). This divides patients into lower- and higher- risk categories. Although treatment objectives in lower-risk MDS (LR-MDS) have traditionally been directed at improving cytopenias (usually anemia) as well as quality of life, recent data supports a potential role for early intervention in delaying transfusion dependency. In addition, careful individualized risk stratification incorporating clinical, cytogenetic, and mutational data might help identify patients at higher-than-expected risk for progression. Given the need for supportive care with red blood cell (RBC) transfusions leading to iron overload, iron chelation should be considered for patients with heavy transfusion requirements at risk for end-organ complications. For patients with LR-MDS and isolated anemia, no high-risk features, and endogenous erythropoietin (EPO) levels below 500 U/L, erythropoiesis-stimulating agents (ESAs) can be attempted to improve anemia. Some LR-MDS patient subgroups may also benefit from specific therapies including luspatercept (MDS with ring sideroblasts), lenalidomide (MDS with deletion 5q), or immunosuppressive therapy (hypocellular MDS). LR-MDS patients failing the above options, or those with multiple cytopenias and/or higher-risk features, can be considered for oral low-dose hypomethylating agent (HMA) therapy. Alternatively, these patients may be enrolled on a clinical trial with promising agents targeting the transforming-growth factor beta (TGF-β) pathway, the hypoxia-inducible factor (HIF) pathway, telomerase activity, inflammatory signaling, or the splicing machinery. In higher-risk MDS (HR-MDS), therapy seeks to modify the natural history of the disease and prolong survival. Eligible patients should be considered for curative allogeneic hematopoietic stem cell transplantation (aHSCT). Despite promising novel combinations, the HMAs azacitidine (AZA) or decitabine (DAC) are still the standard of care for these patients, with intensive chemotherapy-based approaches being a potential option in a small subset of patients. Individuals who fail to respond or progress after HMA experience dismal outcomes and represent a major unmet clinical need. Such patients should be treated as part of a clinical trial if possible. Experimental agents to consider include venetoclax, myeloid cell leukemia 1 (MCL-1) inhibitors, eprenetapopt, CPX-351, immunotherapies (directed towards CD47, TIM3, or CD70), interleukin-1 receptor-associated kinase 4 (IRAK4) inhibitors, pevonedistat, seclidemstat, and eltanexor. In this review, we extensively discuss the current landscape of experimental therapies for both LR- and HR-MDS.
Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Cazzola M. Myelodysplastic Syndromes. N Engl J Med. 2020;383(14):1358–74. https://doi.org/10.1056/NEJMra1904794.
Zeidan AM, Shallis RM, Wang R, Davidoff A, Ma X. Epidemiology of myelodysplastic syndromes: Why characterizing the beast is a prerequisite to taming it. Blood Rev. 2019;34:1–15. https://doi.org/10.1016/j.blre.2018.09.001.
Swerdlow SH, Campo E, Lee Harris N, Jaffe ES, Pileri SA, Stein H, et al. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. Lyon (France): International Agency for Research on Cancer; 2017.
Ogawa S. Genetics of MDS. Blood. 2019;133(10):1049–59. https://doi.org/10.1182/blood-2018-10-844621.
Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G, et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997;89(6):2079–88.
Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Sole F, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120(12):2454–65. https://doi.org/10.1182/blood-2012-03-420489.
Bernard E, Tuechler H, Greenberg PL, Hasserjian RP, Ossa JA, Nannya Y, et al. Molecular International Prognosis Scoring System for Myelodysplastic Syndromes. Presented at ASH Annual Meeting 2021.
Meng F, Chen X, Yu S, Ren X, Liu Z, Fu R, et al. Safety and Efficacy of Eltrombopag and Romiplostim in Myelodysplastic Syndromes: A Systematic Review and Meta-Analysis. Front Oncol. 2020;10:582686. https://doi.org/10.3389/fonc.2020.582686.
Giagounidis A, Mufti GJ, Fenaux P, Sekeres MA, Szer J, Platzbecker U, et al. Results of a randomized, double-blind study of romiplostim versus placebo in patients with low/intermediate-1-risk myelodysplastic syndrome and thrombocytopenia. Cancer. 2014;120(12):1838–46. https://doi.org/10.1002/cncr.28663.
Dickinson M, Cherif H, Fenaux P, Mittelman M, Verma A, Portella MSO, et al. Azacitidine with or without eltrombopag for first-line treatment of intermediate- or high-risk MDS with thrombocytopenia. Blood. 2018;132(25):2629–38. https://doi.org/10.1182/blood-2018-06-855221.
Kantarjian HM, Fenaux P, Sekeres MA, Szer J, Platzbecker U, Kuendgen A, et al. Long-term follow-up for up to 5 years on the risk of leukaemic progression in thrombocytopenic patients with lower-risk myelodysplastic syndromes treated with romiplostim or placebo in a randomised double-blind trial. Lancet Haematol. 2018;5(3):e117–e26. https://doi.org/10.1016/S2352-3026(18)30016-4.
Comont T, Meunier M, Cherait A, Santana C, Cluzeau T, Slama B, et al. Eltrombopag for myelodysplastic syndromes or chronic myelomonocytic leukaemia with no excess blasts and thrombocytopenia: a French multicentre retrospective real-life study. Br J Haematol. 2021;194(2):336–43. https://doi.org/10.1111/bjh.17539.
Komrokji R, Garcia-Manero G, Ades L, Prebet T, Steensma DP, Jurcic JG, et al. Sotatercept with long-term extension for the treatment of anaemia in patients with lower-risk myelodysplastic syndromes: a phase 2, dose-ranging trial. Lancet Haematol. 2018;5(2):e63–72. https://doi.org/10.1016/S2352-3026(18)30002-4.
Ross DM, Arbelaez A, Chee LC, Fong CY, Hiwase D, Kannourakis G, et al. A Phase 2, Open-Label, Ascending Dose Study of Ker-050 for the Treatment of Anemia in Patients with Very Low, Low, or Intermediate Risk Myelodysplastic Syndromes. Blood. 2021;138:3675.
• Henry DH, Glaspy J, Harrup R, Mittelman M, Zhou A, Carraway HE, et al. Roxadustat for the treatment of anemia in patients with lower-risk myelodysplastic syndrome: Open-label, dose-selection, lead-in stage of a phase 3 study. Am J Hematol. 2022;97(2):174–84. https://doi.org/10.1002/ajh.26397This study reports the lead-in dose-finding portion of phase 3 trial evaluating the HIF-PH inhibitor roxadustat for LR-MDS. This agent was shown to lead to TI and a reduction in transfusion requirements in a significant proportion of patients. A major advantage of this drug is convenience from oral formulation.
• Steensma DP, Fenaux P, Van Eygen K, Raza A, Santini V, Germing U, et al. Imetelstat Achieves Meaningful and Durable Transfusion Independence in High Transfusion-Burden Patients With Lower-Risk Myelodysplastic Syndromes in a Phase II Study. J Clin Oncol. 2021;39(1):48–56. https://doi.org/10.1200/JCO.20.01895This phase 2 study demonstrated significant rates of erythroid responses and disease-modifying activity for imetelstat (a telomerase activity inhibitor) in transfusion-dependent LR-MDS patients.
Steensma DP, Wermke M, Klimek VM, Greenberg PL, Font P, Komrokji RS, et al. Phase I First-in-Human Dose Escalation Study of the oral SF3B1 modulator H3B-8800 in myeloid neoplasms. Leukemia. 2021;35(12):3542–50. https://doi.org/10.1038/s41375-021-01328-9.
Tobiasson M, Dybedahl I, Holm MS, Karimi M, Brandefors L, Garelius H, et al. Limited clinical efficacy of azacitidine in transfusion-dependent, growth factor-resistant, low- and Int-1-risk MDS: Results from the nordic NMDSG08A phase II trial. Blood Cancer J. 2014;4:e189. https://doi.org/10.1038/bcj.2014.8.
Thepot S, Ben Abdelali R, Chevret S, Renneville A, Beyne-Rauzy O, Prebet T, et al. A randomized phase II trial of azacitidine +/- epoetin-beta in lower-risk myelodysplastic syndromes resistant to erythropoietic stimulating agents. Haematologica. 2016;101(8):918–25. https://doi.org/10.3324/haematol.2015.140988.
Jabbour E, Short NJ, Montalban-Bravo G, Huang X, Bueso-Ramos C, Qiao W, et al. Randomized phase 2 study of low-dose decitabine vs low-dose azacitidine in lower-risk MDS and MDS/MPN. Blood. 2017;130(13):1514–22. https://doi.org/10.1182/blood-2017-06-788497.
Montalban-Bravo G, Jabbour E, Class C, Short NJ, Kanagal-Shamanna R, Kadia TM, et al. Long-Term Follow up of a Randomized Phase 2 Study of Low-Dose Decitabine Versus Low-Dose Azacitidine in Lower-Risk Myelodysplastic Syndromes. Blood. 2019;134(Supplement_1):1715. https://doi.org/10.1182/blood-2019-129141.
• Garcia-Manero G, Santini V, Almeida A, Platzbecker U, Jonasova A, Silverman LR, et al. Phase III, Randomized, Placebo-Controlled Trial of CC-486 (Oral Azacitidine) in Patients With Lower-Risk Myelodysplastic Syndromes. J Clin Oncol. 2021;39(13):1426–36. https://doi.org/10.1200/JCO.20.02619This study demonstrated that an oral HMA regimen is effective in improving cytopenia in LR-MDS and is well tolerated.
• Garcia-Manero G, McCloskey JK, Griffiths EA, Yee K, Zeidan AM, Al-Kali A, et al. Oral Decitabine/Cedazuridine in Patients with Lower Risk Myelodysplastic Syndrome: A Longer-Term Follow-up of from the Ascertain Study. Blood. 2021;138:66 This study demonstrated that an oral HMA regimen is effective in improving cytopenia in LR-MDS and is well tolerated.
•• Garcia JS, Wei AH, Borate U, Fong CY, Baer MR, Nolte F, et al. Safety, Efficacy, and Patient-Reported Outcomes of Venetoclax in Combination with Azacitidine for the Treatment of Patients with Higher-Risk Myelodysplastic Syndrome: A Phase 1b Study. Blood. 2020;136(Supplement 1):55–7. https://doi.org/10.1182/blood-2020-139492This abstract describes high response rates with azacitidine and venetoclax for the treatment of HR-MDS.
•• Bazinet A, Jabbour EJ, Kantarjian H, Chien KS, DiNardo CD, Ohanian M, et al. A Phase I/II Study of Venetoclax in Combination with 5-Azacytidine in Treatment-Naïve and Relapsed/Refractory High-Risk Myelodysplastic Syndrome (MDS) or Chronic Myelomonocytic Leukemia (CMML). Blood. 2021;138(Supplement 1):535. https://doi.org/10.1182/blood-2021-153086This abstract describes high response rates with azacitidine and venetoclax for the treatment of HR-MDS, including in the context of HMA failure.
•• Zeidan AM, Borate U, Pollyea DA, Brunner AM, Roncolato F, Garcia JS, et al. Venetoclax and Azacitidine in the Treatment of Patients with Relapsed/Refractory Myelodysplastic Syndrome. Blood. 2021;138(Supplement 1):537. https://doi.org/10.1182/blood-2021-145646This abstract demonstrated an encouraging OS (12.6 months) with azacitidine and venetoclax for the treatment of HR-MDS after HMA failure.
Peterlin P, Turlure P, Chevallier P, Gourin M-P, Dumas P-Y, Thepot S, et al. CPX 351 As First Line Treatment in Higher Risk MDS. a Phase II Trial By the GFM. Blood. 2021;138:243.
Montalban-Bravo G, Jabbour EJ, Estrov ZE, Kadia TM, Ravandi F, Chien KS, et al. Updated Results of a Phase 1/2 Study of Lower Dose CPX-351 for Patients with Int-2 or High Risk IPSS Myelodysplastic Syndromes and Chronic Myelomonocytic Leukemia after Failure to Hypomethylating Agents. Blood. 2021;138(Supplement 1):3674. https://doi.org/10.1182/blood-2021-151493.
• Sallman DA, Malki MA, Asch AS, Lee DJ, Kambhampati S, Donnellan WB, et al. Tolerability and efficacy of the first-in-class anti-CD47 antibody magrolimab combined with azacitidine in MDS and AML patients: Phase Ib results. J Clin Oncol. 2020;38(15_suppl):7507. https://doi.org/10.1200/JCO.2020.38.15_suppl.7507This study demonstrated an encouraging ORR (91%) for the combination of magrolimab and azacitidine in HR-MDS.
Garcia-Manero G, Erba HP, Sanikommu SR, Altman JK, Sayar H, Scott BL, et al. Evorpacept (ALX148), a CD47-Blocking Myeloid Checkpoint Inhibitor, in Combination with Azacitidine: A Phase 1/2 Study in Patients with Myelodysplastic Syndrome (ASPEN-02). Blood. 2021;138:2601.
Brunner AM, Esteve J, Porkka K, Knapper S, Traer E, Scholl S, et al. Efficacy and Safety of Sabatolimab (MBG453) in Combination with Hypomethylating Agents (HMAs) in Patients (Pts) with Very High/High-Risk Myelodysplastic Syndrome (vHR/HR-MDS) and Acute Myeloid Leukemia (AML): Final Analysis from a Phase Ib Study. Blood. 2021;138:244.
Sallman DA, DeZern AE, Garcia-Manero G, Steensma DP, Roboz GJ, Sekeres MA, et al. Eprenetapopt (APR-246) and Azacitidine in TP53-Mutant Myelodysplastic Syndromes. J Clin Oncol. 2021;39(14):1584–94. https://doi.org/10.1200/JCO.20.02341.
Cluzeau T, Sebert M, Rahme R, Cuzzubbo S, Lehmann-Che J, Madelaine I, et al. Eprenetapopt Plus Azacitidine in TP53-Mutated Myelodysplastic Syndromes and Acute Myeloid Leukemia: A Phase II Study by the Groupe Francophone des Myelodysplasies (GFM). J Clin Oncol. 2021;39(14):1575–83. https://doi.org/10.1200/JCO.20.02342.
Sebert M, Cluzeau T, Beyne Rauzy O, Stamatoulas Bastard A, Dimicoli-Salazar S, Thepot S, et al. Ivosidenib Monotherapy Is Effective in Patients with IDH1 Mutated Myelodysplastic Syndrome (MDS): The Idiome Phase 2 Study By the GFM Group. Blood. 2021;138(Supplement 1):62. https://doi.org/10.1182/blood-2021-146932.
Venugopal S, Dinardo CD, Takahashi K, Konopleva M, Loghavi S, Borthakur G, et al. Phase II study of the IDH2-inhibitor enasidenib in patients with high-risk IDH2-mutated myelodysplastic syndromes (MDS). J Clin Oncols. 2021;39(15_suppl):7010. https://doi.org/10.1200/JCO.2021.39.15_suppl.7010.
Abuasab T, Jabbour EJ, Short NJ, Konopleva M, Chien KS, Mohamed SF, et al. Initial Results of Phase I/II Study of Azacitidine in Combination with Quizartinib for Patients with Myelodysplastic Syndrome and Myelodysplastic/Myeloproliferative Neoplasm with FLT3 or CBL Mutations. Blood. 2021;138:1536.
Garcia-Manero G, Tarantolo S, Verma A, Dugan J, Winer ES, Giagounidis A, et al. A phase 1, dose escalation trial with novel oral IRAK4 inhibitor CA-4948 in patients with acute myelogenous leukemia or myelodysplastic syndrome - interim report. Presented at EHA Congress 2021.
Swords RT, Erba HP, DeAngelo DJ, Bixby DL, Altman JK, Maris M, et al. Pevonedistat (MLN4924), a First-in-Class NEDD8-activating enzyme inhibitor, in patients with acute myeloid leukaemia and myelodysplastic syndromes: a phase 1 study. Br J Haematol. 2015;169(4):534–43. https://doi.org/10.1111/bjh.13323.
Sekeres MA, Watts J, Radinoff A, Sangerman MA, Cerrano M, Lopez PF, et al. Randomized phase 2 trial of pevonedistat plus azacitidine versus azacitidine for higher-risk MDS/CMML or low-blast AML. Leukemia. 2021;35(7):2119–24. https://doi.org/10.1038/s41375-021-01125-4.
Lee S, Mohan S, Knupp J, Chamoun K, Bai X, Ma X, et al. Updated overall survival of eltanexor for the treatment of patients with hypomethylating agent refractory myelodysplastic syndrome. J Clin Oncol. 2021;39(15_suppl):e19037. https://doi.org/10.1200/JCO.2021.39.15_suppl.e19037.
Angelucci E, Li J, Greenberg P, Wu D, Hou M, Montano Figueroa EH, et al. Iron Chelation in Transfusion-Dependent Patients With Low- to Intermediate-1-Risk Myelodysplastic Syndromes: A Randomized Trial. Ann Intern Med. 2020;172(8):513–22. https://doi.org/10.7326/M19-0916.
Adrianzen Herrera D, Pradhan K, Snyder R, Karanth S, Janakiram M, Mantzaris I, et al. Myelodysplastic syndromes and the risk of cardiovascular disease in older adults: A SEER-medicare analysis. Leukemia. 2020;34(6):1689–93. https://doi.org/10.1038/s41375-019-0673-8.
Sano S, Wang Y, Walsh K. Clonal Hematopoiesis and Its Impact on Cardiovascular Disease. Circ J. 2018;83(1):2–11. https://doi.org/10.1253/circj.CJ-18-0871.
Fenaux P, Santini V, Spiriti MAA, Giagounidis A, Schlag R, Radinoff A, et al. A phase 3 randomized, placebo-controlled study assessing the efficacy and safety of epoetin-alpha in anemic patients with low-risk MDS. Leukemia. 2018;32(12):2648–58. https://doi.org/10.1038/s41375-018-0118-9.
Platzbecker U, Symeonidis A, Oliva EN, Goede JS, Delforge M, Mayer J, et al. A phase 3 randomized placebo-controlled trial of darbepoetin alfa in patients with anemia and lower-risk myelodysplastic syndromes. Leukemia. 2017;31(9):1944–50. https://doi.org/10.1038/leu.2017.192.
Jadersten M, Montgomery SM, Dybedal I, Porwit-MacDonald A, Hellstrom-Lindberg E. Long-term outcome of treatment of anemia in MDS with erythropoietin and G-CSF. Blood. 2005;106(3):803–11. https://doi.org/10.1182/blood-2004-10-3872.
Hellstrom-Lindberg E, Negrin R, Stein R, Krantz S, Lindberg G, Vardiman J, et al. Erythroid response to treatment with G-CSF plus erythropoietin for the anaemia of patients with myelodysplastic syndromes: proposal for a predictive model. Br J Haematol. 1997;99(2):344–51. https://doi.org/10.1046/j.1365-2141.1997.4013211.x.
•• Fenaux P, Platzbecker U, Mufti GJ, Garcia-Manero G, Buckstein R, Santini V, et al. Luspatercept in Patients with Lower-Risk Myelodysplastic Syndromes. N Engl J Med. 2020;382(2):140–51. https://doi.org/10.1056/NEJMoa1908892This landmark phase 3 study (MEDALIST trial) established luspatercept as an effective treatment option for transfusion-dependent patients with MDS-RS. This led to the FDA approval of the first TGF-β ligand trap for MDS.
Della Porta M, Platzbecker U, Santini V, Garcia-Manero G, Komrokji RS, Ito R, et al. The Commands Trial: A Phase 3 Study of the Efficacy and Safety of Luspatercept Versus Epoetin Alfa for the Treatment of Anemia Due to IPSS-R Very Low-, Low-, or Intermediate-Risk MDS in Erythropoiesis Stimulating Agent-Naive Patients Who Require RBC Transfusions. Blood. 2020;136(Supplement 1):1–2. https://doi.org/10.1182/blood-2020-140284.
Fenaux P, Giagounidis A, Selleslag D, Beyne-Rauzy O, Mufti G, Mittelman M, et al. A randomized phase 3 study of lenalidomide versus placebo in RBC transfusion-dependent patients with Low-/Intermediate-1-risk myelodysplastic syndromes with del5q. Blood. 2011;118(14):3765–76. https://doi.org/10.1182/blood-2011-01-330126.
Durrani J, Maciejewski JP. Idiopathic aplastic anemia vs hypocellular myelodysplastic syndrome. Hematology. 2019;2019(1):97–104. https://doi.org/10.1182/hematology.2019000019.
Stahl M, DeVeaux M, De Witte T, Neukirchen J, Sekeres MA, Brunner AM, et al. The use of immunosuppressive therapy in MDS: clinical outcomes and their predictors in a large international patient cohort. Blood Adv. 2018;2(14):1765–72.
Gonzalez-Lugo JD, Kambhampati S, Yacoub A, Donnellan W, Bhagat P, Fehn K, et al. Lenalidomide and Eltrombopag for Treatment in Low or Intermediate Risk Myelodysplastic Syndrome: Result of a Phase 2 Study Combination Clinical Trial. Blood. 2021;138(Supplement 1):65. https://doi.org/10.1182/blood-2021-146597.
Komrokji RS. Activin Receptor II Ligand Traps: New Treatment Paradigm for Low-Risk MDS. Curr Hematol Malig Rep. 2019;14(4):346–51. https://doi.org/10.1007/s11899-019-00517-9.
Verma A, Brunner AM, Pennock G, McMullen D, Wade M, Yang H, et al. Phase 1/2 Study of Oral TP-0184 for the Treatment of Anemia in Adults with Low-or Intermediate-Risk Myelodysplastic Syndromes. Blood. 2021;138:1534.
Gupta N, Wish JB. Hypoxia-Inducible Factor Prolyl Hydroxylase Inhibitors: A Potential New Treatment for Anemia in Patients With CKD. Am J Kidney Dis. 2017;69(6):815–26. https://doi.org/10.1053/j.ajkd.2016.12.011.
Park HS, Choi J, See CJ, Kim JA, Park SN, Im K, et al. Dysregulation of Telomere Lengths and Telomerase Activity in Myelodysplastic Syndrome. Ann Lab Med. 2017;37(3):195–203. https://doi.org/10.3343/alm.2017.37.3.195.
Briatore F, Barrera G, Pizzimenti S, Toaldo C, Casa CD, Laurora S, et al. Increase of telomerase activity and hTERT expression in myelodysplastic syndromes. Cancer Biol Ther. 2009;8(10):883–9. https://doi.org/10.4161/cbt.8.10.8130.
Harley CB. Telomerase and cancer therapeutics. Nat Rev Cancer. 2008;8(3):167–79. https://doi.org/10.1038/nrc2275.
Brunner AM, Steensma DP. Targeting Aberrant Splicing in Myelodysplastic Syndromes: Biologic Rationale and Clinical Opportunity. Hematol Oncol Clin North Am. 2020;34(2):379–91. https://doi.org/10.1016/j.hoc.2019.10.003.
Kim E, Ilagan JO, Liang Y, Daubner GM, Lee SC, Ramakrishnan A, et al. SRSF2 Mutations Contribute to Myelodysplasia by Mutant-Specific Effects on Exon Recognition. Cancer Cell. 2015;27(5):617–30. https://doi.org/10.1016/j.ccell.2015.04.006.
Ilagan JO, Ramakrishnan A, Hayes B, Murphy ME, Zebari AS, Bradley P, et al. U2AF1 mutations alter splice site recognition in hematological malignancies. Genome Res. 2015;25(1):14–26. https://doi.org/10.1101/gr.181016.114.
Malcovati L, Stevenson K, Papaemmanuil E, Neuberg D, Bejar R, Boultwood J, et al. SF3B1-mutant MDS as a distinct disease subtype: a proposal from the International Working Group for the Prognosis of MDS. Blood. 2020;136(2):157–70. https://doi.org/10.1182/blood.2020004850.
Seiler M, Yoshimi A, Darman R, Chan B, Keaney G, Thomas M, et al. H3B-8800, an orally available small-molecule splicing modulator, induces lethality in spliceosome-mutant cancers. Nat Med. 2018;24(4):497–504. https://doi.org/10.1038/nm.4493.
Fong JY, Pignata L, Goy PA, Kawabata KC, Lee SC, Koh CM, et al. Therapeutic Targeting of RNA Splicing Catalysis through Inhibition of Protein Arginine Methylation. Cancer Cell. 2019;36(2):194–209 e9. https://doi.org/10.1016/j.ccell.2019.07.003.
de Mooij CEM, Netea MG, van der Velden W, Blijlevens NMA. Targeting the interleukin-1 pathway in patients with hematological disorders. Blood. 2017;129(24):3155–64. https://doi.org/10.1182/blood-2016-12-754994.
Korn C, Mendez-Ferrer S. Myeloid malignancies and the microenvironment. Blood. 2017;129(7):811–22. https://doi.org/10.1182/blood-2016-09-670224.
Mocsai A, Ruland J, Tybulewicz VL. The SYK tyrosine kinase: a crucial player in diverse biological functions. Nat Rev Immunol. 2010;10(6):387–402. https://doi.org/10.1038/nri2765.
Carnevale J, Ross L, Puissant A, Banerji V, Stone RM, DeAngelo DJ, et al. SYK regulates mTOR signaling in AML. Leukemia. 2013;27(11):2118–28. https://doi.org/10.1038/leu.2013.89.
Garcia-Manero G, Shan J, Faderl S, Cortes J, Ravandi F, Borthakur G, et al. A prognostic score for patients with lower risk myelodysplastic syndrome. Leukemia. 2008;22(3):538–43. https://doi.org/10.1038/sj.leu.2405070.
Fenaux P, Mufti GJ, Hellstrom-Lindberg E, Santini V, Finelli C, Giagounidis A, et al. Efficacy of azacitidine compared with that of conventional care regimens in the treatment of higher-risk myelodysplastic syndromes: a randomised, open-label, phase III study. Lancet Oncol. 2009;10(3):223–32. https://doi.org/10.1016/S1470-2045(09)70003-8.
Lubbert M, Suciu S, Baila L, Ruter BH, Platzbecker U, Giagounidis A, et al. Low-dose decitabine versus best supportive care in elderly patients with intermediate- or high-risk myelodysplastic syndrome (MDS) ineligible for intensive chemotherapy: final results of the randomized phase III study of the European Organisation for Research and Treatment of Cancer Leukemia Group and the German MDS Study Group. J Clin Oncol. 2011;29(15):1987–96. https://doi.org/10.1200/JCO.2010.30.9245.
Garcia JS, Swords RT, Roboz GJ, Jacoby MA, Garcia-Manero G, Hong WJ, et al. A systematic review of higher-risk myelodysplastic syndromes clinical trials to determine the benchmark of azacitidine and explore alternative endpoints for overall survival. Leuk Res. 2021;104:106555. https://doi.org/10.1016/j.leukres.2021.106555.
Silverman LR, Fenaux P, Mufti GJ, Santini V, Hellstrom-Lindberg E, Gattermann N, et al. Continued azacitidine therapy beyond time of first response improves quality of response in patients with higher-risk myelodysplastic syndromes. Cancer. 2011;117(12):2697–702. https://doi.org/10.1002/cncr.25774.
Garcia-Manero G, Griffiths EA, Steensma DP, Roboz GJ, Wells R, McCloskey J, et al. Oral cedazuridine/decitabine for MDS and CMML: a phase 2 pharmacokinetic/pharmacodynamic randomized crossover study. Blood. 2020;136(6):674–83. https://doi.org/10.1182/blood.2019004143.
Cutler CS, Lee SJ, Greenberg P, Deeg HJ, Perez WS, Anasetti C, et al. A decision analysis of allogeneic bone marrow transplantation for the myelodysplastic syndromes: delayed transplantation for low-risk myelodysplasia is associated with improved outcome. Blood. 2004;104(2):579–85. https://doi.org/10.1182/blood-2004-01-0338.
Yahng SA, Kim M, Kim TM, Jeon YW, Yoon JH, Shin SH, et al. Better transplant outcome with pre-transplant marrow response after hypomethylating treatment in higher-risk MDS with excess blasts. Oncotarget. 2017;8(7):12342–54. https://doi.org/10.18632/oncotarget.12511.
Zeidan AM, Kharfan-Dabaja MA, Komrokji RS. Beyond hypomethylating agents failure in patients with myelodysplastic syndromes. Curr Opin Hematol. 2014;21(2):123–30. https://doi.org/10.1097/MOH.0000000000000016.
Jilg S, Reidel V, Muller-Thomas C, Konig J, Schauwecker J, Hockendorf U, et al. Blockade of BCL-2 proteins efficiently induces apoptosis in progenitor cells of high-risk myelodysplastic syndromes patients. Leukemia. 2016;30(1):112–23. https://doi.org/10.1038/leu.2015.179.
DiNardo CD, Jonas BA, Pullarkat V, Thirman MJ, Garcia JS, Wei AH, et al. Azacitidine and Venetoclax in Previously Untreated Acute Myeloid Leukemia. N Engl J Med. 2020;383(7):617–29. https://doi.org/10.1056/NEJMoa2012971.
Tsao T, Shi Y, Kornblau S, Lu H, Konoplev S, Antony A, et al. Concomitant inhibition of DNA methyltransferase and BCL-2 protein function synergistically induce mitochondrial apoptosis in acute myelogenous leukemia cells. Ann Hematol. 2012;91(12):1861–70. https://doi.org/10.1007/s00277-012-1537-8.
Zeidan AM, Garcia JS, Fenaux P, Platzbecker U, Miyazaki Y, Xiao Z-J, et al. Phase 3 VERONA study of venetoclax with azacitidine to assess change in complete remission and overall survival in treatment-naïve higher-risk myelodysplastic syndromes. J Clin Oncol. 2021;39(15_suppl):TPS7054. https://doi.org/10.1200/JCO.2021.39.15_suppl.TPS7054.
Wei AH, Roberts AW, Spencer A, Rosenberg AS, Siegel D, Walter RB, et al. Targeting MCL-1 in hematologic malignancies: Rationale and progress. Blood Rev. 2020;44:100672. https://doi.org/10.1016/j.blre.2020.100672.
Lancet JE, Uy GL, Cortes JE, Newell LF, Lin TL, Ritchie EK, et al. CPX-351 (cytarabine and daunorubicin) Liposome for Injection Versus Conventional Cytarabine Plus Daunorubicin in Older Patients With Newly Diagnosed Secondary Acute Myeloid Leukemia. J Clin Oncol. 2018;36(26):2684–92. https://doi.org/10.1200/JCO.2017.77.6112.
Chao MP, Takimoto CH, Feng DD, McKenna K, Gip P, Liu J, et al. Therapeutic Targeting of the Macrophage Immune Checkpoint CD47 in Myeloid Malignancies. Front Oncol. 2019;9:1380. https://doi.org/10.3389/fonc.2019.01380.
Pang WW, Pluvinage JV, Price EA, Sridhar K, Arber DA, Greenberg PL, et al. Hematopoietic stem cell and progenitor cell mechanisms in myelodysplastic syndromes. Proc Natl Acad Sci U S A. 2013;110(8):3011–6. https://doi.org/10.1073/pnas.1222861110.
Vyas P, Knapper S, Kelly R, Salim R, Lubowiecki M, Royston D. Initial phase 1 results of the first-in-class anti-CD47 antibody Hu5F9-G4 in relapsed/refractory acute myeloid leukemia patients. Presented at EHA Congress 2018.
Boasman K, Bridle C, Simmonds M, Rinaldi C. Role of pro-phagocytic calreticulin and anti-phagocytic CD47 in MDS and MPN models treated with azacytidine or ruxolitinib. Presented at EHA Congress 2017.
Garcia-Manero G, Daver NG, Xu J, Chao M, Chung T, Tan A, et al. Magrolimab + azacitidine versus azacitidine + placebo in untreated higher risk (HR) myelodysplastic syndrome (MDS): The phase 3, randomized, ENHANCE study. J Clin Oncol. 2021;39(15_suppl):TPS7055. https://doi.org/10.1200/JCO.2021.39.15_suppl.TPS7055.
Rezaei M, Tan J, Zeng C, Li Y, Ganjalikhani-Hakemi M. TIM-3 in Leukemia; Immune Response and Beyond. Front Oncol. 2021;11:753677. https://doi.org/10.3389/fonc.2021.753677.
Zeidan AM, Komrokji RS, Brunner AM. TIM-3 pathway dysregulation and targeting in cancer. Expert Rev Anticancer Ther. 2021;21(5):523–34. https://doi.org/10.1080/14737140.2021.1865814.
Asayama T, Tamura H, Ishibashi M, Kuribayashi-Hamada Y, Onodera-Kondo A, Okuyama N, et al. Functional expression of Tim-3 on blasts and clinical impact of its ligand galectin-9 in myelodysplastic syndromes. Oncotarget. 2017;8(51):88904–17. https://doi.org/10.18632/oncotarget.21492.
Kikushige Y, Miyamoto T, Yuda J, Jabbarzadeh-Tabrizi S, Shima T, Takayanagi S, et al. A TIM-3/Gal-9 Autocrine Stimulatory Loop Drives Self-Renewal of Human Myeloid Leukemia Stem Cells and Leukemic Progression. Cell Stem Cell. 2015;17(3):341–52. https://doi.org/10.1016/j.stem.2015.07.011.
Zeidan AM, Esteve J, Giagounidis A, Kim H-J, Miyazaki Y, Platzbecker U, et al. The STIMULUS Program: Clinical Trials Evaluating Sabatolimab (MBG453) Combination Therapy in Patients (Pts) with Higher-Risk Myelodysplastic Syndromes (HR-MDS) or Acute Myeloid Leukemia (AML). Blood. 2020;136:45–6.
Riether C, Schurch CM, Buhrer ED, Hinterbrandner M, Huguenin AL, Hoepner S, et al. CD70/CD27 signaling promotes blast stemness and is a viable therapeutic target in acute myeloid leukemia. J Exp Med. 2017;214(2):359–80. https://doi.org/10.1084/jem.20152008.
Riether C, Pabst T, Hopner S, Bacher U, Hinterbrandner M, Banz Y, et al. Targeting CD70 with cusatuzumab eliminates acute myeloid leukemia stem cells in patients treated with hypomethylating agents. Nat Med. 2020;26(9):1459–67. https://doi.org/10.1038/s41591-020-0910-8.
Argenx. Argenx Announces 2021 Corporate Priorities and Highlights Recent Achievements Across Immunology Pipeline. 2021. https://www.argenx.com/news/argenx-announces-2021-corporate-priorities-and-highlights-recent-achievements-across. Accessed 6 Jan 2022.
Roboz GJ, Pabst T, Aribi A, Brandwein JM, Döhner H, Fiedler W, et al. Safety and Efficacy of Cusatuzumab in Combination with Venetoclax and Azacitidine (CVA) in Patients with Previously Untreated Acute Myeloid Leukemia (AML) Who Are Not Eligible for Intensive Chemotherapy; An Open-Label, Multicenter, Phase 1b Study. Blood. 2021;138(Supplement 1):369. https://doi.org/10.1182/blood-2021-150371.
Aribi A, Advani AS, Donnellan W, Fathi AT, Rotta M, Tomlinson BK, et al. A Phase 1 Study of Sea-CD70 in Myeloid Malignancies. Blood. 2020;136(Supplement 1):23–4. https://doi.org/10.1182/blood-2020-136203.
Bernard E, Nannya Y, Hasserjian RP, Devlin SM, Tuechler H, Medina-Martinez JS, et al. Implications of TP53 allelic state for genome stability, clinical presentation and outcomes in myelodysplastic syndromes. Nat Med. 2020;26(10):1549–56. https://doi.org/10.1038/s41591-020-1008-z.
Peng X, Zhang MQ, Conserva F, Hosny G, Selivanova G, Bykov VJ, et al. APR-246/PRIMA-1MET inhibits thioredoxin reductase 1 and converts the enzyme to a dedicated NADPH oxidase. Cell Death Dis. 2013;4:e881. https://doi.org/10.1038/cddis.2013.417.
Aprea Therapeutics. Aprea Therapeutics Announces Results of Primary Endpoint from Phase 3 Trial of Eprenetapopt in TP53 Mutant Myelodysplastic Syndromes (MDS). 2020. https://ir.aprea.com/news-releases/news-release-details/aprea-therapeutics-announces-results-primary-endpoint-phase-3. Accessed 28 Dec 2021.
Haferlach T, Nagata Y, Grossmann V, Okuno Y, Bacher U, Nagae G, et al. Landscape of genetic lesions in 944 patients with myelodysplastic syndromes. Leukemia. 2014;28(2):241–7. https://doi.org/10.1038/leu.2013.336.
Daver N, Strati P, Jabbour E, Kadia T, Luthra R, Wang S, et al. FLT3 mutations in myelodysplastic syndrome and chronic myelomonocytic leukemia. Am J Hematol. 2013;88(1):56–9. https://doi.org/10.1002/ajh.23345.
Smith MA, Choudhary GS, Pellagatti A, Choi K, Bolanos LC, Bhagat TD, et al. U2AF1 mutations induce oncogenic IRAK4 isoforms and activate innate immune pathways in myeloid malignancies. Nat Cell Biol. 2019;21(5):640–50. https://doi.org/10.1038/s41556-019-0314-5.
Choudhary GS, Smith MA, Pellagatti A, Bhagat TD, Gordon S, Pandey S, et al. SF3B1 Mutations Induce Oncogenic IRAK4 Isoforms and Activate Targetable Innate Immune Pathways in MDS and AML. Blood. 2019;134(Supplement_1):4224. https://doi.org/10.1182/blood-2019-124458.
Takeda Pharmaceutical. Takeda Provides Update on Phase 3 PANTHER (Pevonedistat-3001) Trial. 2021 https://www.takeda.com/newsroom/newsreleases/2021/takeda-provides-update-on-phase-3-panther-pevonedistat-3001-trial/. Accessed 8 Jan 2022.
Sacilotto N, Dessanti P, Lufino MMP, Ortega A, Rodriguez-Gimeno A, Salas J, et al. Comprehensive in Vitro Characterization of the LSD1 Small Molecule Inhibitor Class in Oncology. ACS Pharmacol Transl Sci. 2021;4(6):1818–34. https://doi.org/10.1021/acsptsci.1c00223.
Buscarlet M, Krasteva V, Ho L, Simon C, Hebert J, Wilhelm B, et al. Essential role of BRG, the ATPase subunit of BAF chromatin remodeling complexes, in leukemia maintenance. Blood. 2014;123(11):1720–8. https://doi.org/10.1182/blood-2013-02-483495.
Etchin J, Berezovskaya A, Conway AS, Galinsky IA, Stone RM, Baloglu E, et al. KPT-8602, a second-generation inhibitor of XPO1-mediated nuclear export, is well tolerated and highly active against AML blasts and leukemia-initiating cells. Leukemia. 2017;31(1):143–50. https://doi.org/10.1038/leu.2016.145.
Etchin J, Montero J, Berezovskaya A, Le BT, Kentsis A, Christie AL, et al. Activity of a selective inhibitor of nuclear export, selinexor (KPT-330), against AML-initiating cells engrafted into immunosuppressed NSG mice. Leukemia. 2016;30(1):190–9. https://doi.org/10.1038/leu.2015.194.
Hashmi MS, Sharif MA, Jaan A, Salman U, Aziz S, Shahab A, et al. Efficacy and Safety of Selinexor for Acute Myeloid Leukemia: A Systematic Review. Blood. 2020;136(Supplement 1):15–6. https://doi.org/10.1182/blood-2020-141050.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Alexandre Bazinet declares he has no conflict of interest. Guillermo Montalban-Bravo declares grants or contracts from IFM Therapeutics, Rigel Pharmaceuticals, Jazz Pharmaceuticals, Daichii Sankyo, Stemline Therapeutics, and Salarius Pharmaceuticals.
Human and Animal Rights and Informed Consent
The authors did not perform any studies with human or animal subjects as part of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Leukemia
Rights and permissions
About this article
Cite this article
Bazinet, A., Bravo, G.M. New Approaches to Myelodysplastic Syndrome Treatment. Curr. Treat. Options in Oncol. 23, 668–687 (2022). https://doi.org/10.1007/s11864-022-00965-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11864-022-00965-1