Abstract
Introduction
Recently, burnout has amassed considerable attention because of deleterious effects on workers and the work environment. Frequently, EMS clinicians find themselves prone to experiencing burnout, yet little is known about etiologies in this population.
Objective
To estimate prevalence and predictors of burnout in EMS clinicians.
Methods
This was a cross-sectional survey study of nine EMS agencies from North Carolina selected based on geography and population. Emergency medical technicians (EMTs), advanced EMTs, and paramedics were included. Emergency medical responders and air medical personnel were excluded if those positions were a primary occupational function. The Professional Quality of Life (ProQOL) Scale was used to assess burnout. Parametric and nonparametric testing was used to assess factors potentially affecting burnout. Factors significant in univariate analyses were included in a hierarchical linear regression model to determine unique predictors of burnout while controlling for confounders. The area under the curve (AUC) of the receiver operating characteristic (ROC) was used to determine model predictability.
Results
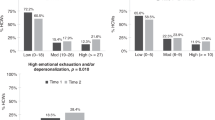
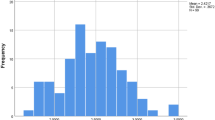
A total of 686 EMS clinicians completed the survey. Overall, 57.3% (n = 393) were likely to have burnout. Of the 328 respondents who were likely to have burnout, 254 (77.4%) and 211 (75.1%) also were identified as likely to suffer from compassion fatigue or vicarious trauma, respectively. Overall, 152 (22.2%) were likely to suffer from all three stress disorders, 118 (56.5%) of which scored high enough to potentially produce immune system dysregulation. Prior suicidal thoughts ((sr2 = 0.042, p < 0.001), attempts (sr2 = 0.025, p < 0.001) or the presence of vicarious trauma (sr2 = 0.040, p < 0.001) accounted for 4.2%, 2.5%, and 4.0% of model variance, respectively. Years of field experience (sr2 = 0.035, p < 0.001) and credential level (sr2 = 0.011, p = 0.005) accounted for 4.6% of model variance. Finally, a respondent’s experience or knowledge of debriefing (sr2 = 0.008, p = 0.023); experiencing adversity in childhood in the form of familial mental illness, depression, or suicide (sr2 = 0.009, p = 0.016); or the incarceration of a family member (sr2 = 0.010, p = 0.011) accounted for a combined 2.7% of model variance. Model predictability showed an AUCROC of 81.5%.
Conclusions
This study showed a nearly 60% prevalence of occupational burnout in the group of EMS clinicians surveyed, making burnout of considerable concern in this population. Further study is needed to address occupational factors that contribute to burnout in EMS clinicians.

Similar content being viewed by others
Data availability
Reprints are not available from the authors.
References
Shoman Y, El May E, Marca S et al (2021) Predictors of occupational burnout: a systematic review. Int J Environ Res Public Health18(17):9188. https://doi.org/10.3390/ijerph18179188
Shanafelt TD, West CP, Dyrbye LN et al (2022) Changes in burnout and satisfaction with work-life integration in physicians during the first 2 years of the COVID-19 pandemic. Mayo Clin Proc 97(12):2248–2258. https://doi.org/10.1016/j.mayocp.2022.09.002
Olff M, Langeland W, Gersons BPR (2005) The psychobiology og PTSD: coping with trauma. Psychoneuroendocrinology 30(10):974–982. https://doi.org/10.1016/j.psyneuen.2005.04.009
Stephens MA, Wand G (2012) Stress and the HPA axis: role of glucocorticoids in alcohol dependence. Alcohol Research 34(4):468–483
Schnurr PP, Green BL eds (2004) Trauma and health: physical health consequences of exposure to extreme stress. American Psychological Association. https://doi.org/10.1037/10723-000
Brewin CR, Holmes EA (2003) Psychological theories of posttraumatic stress disorder. Clin Psychol Rev 23(3):339–376. https://doi.org/10.1016/S0272-7358(03)00033-3
Occupational Safety and Health Administration (OSHA). Critical incident stress guide. Accessed 21 Jan 2020, from: https://www.osha.gov/SLTC/emergencypreparedness/guides/critical.html
Shelton R, Kelly J (1995) EMS stress: an emergency responder’s handbook for living well. JEMS Communications. Carlsbad, CA
Silverman MN, Pearce BD, Biron CA, Miller AH (2005) Immune modulation of the hypothalamic-pituitary-adrenal (HPA) axis during viral infection. Viral Immunol 18(1):41–78. https://doi.org/10.1089/vim.2005.18.41
Workplace stress (2023) The American Institute of Stress. Retrieved April 22, 2023, from https://www.stress.org/workplace-stress#:~:text=Research%20by%20Mental%20Health%20America,for%20mental%20and%20emotional%20exhaustion.
Marz JT, Petrie N, Boyes A (2021). Burnout is about your workplace, not your people. Harvard Business Review. Retrieved April 22, 2023, from https://hbr.org/2019/12/burnout-is-about-your-workplace-not-your-people
Crowe RP, Fernandez AR, Pepe PE et al (2020) The association of job demands and resources with burnout among emergency medical services professionals. J Am Coll Emerg Physicians Open 1(1):6–16. https://doi.org/10.1002/emp2.12014
United States Census Bureau (2010) 2010 Census Urban Area Delineation Program. https://www.census.gov/geo/reference/ua/urban-rural-2010.html. Accessed 5 Oct 2015
North Carolina Department of Commerce. Where the jobs are: supply and demand for labor in North Carolina’s regions. Accessed 14 Feb 2020. https://www.nccommerce.com/blog/2016/12/13/where-jobs-are-supply-and-demand-labor-north-carolina%E2%80%99s-regions
Beck JG, Grant DM, Read JP et al (2008) The impact of event scale-revised: psychometric properties in a sample of motor vehicle accident survivors. J Anxiety Disord 22(2):187–198. Epub 2007 Feb 24
Dube SR, Felitti VJ, Dong M et al (2003) Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the adverse childhood experiences study. Pediatrics 111(3):564–572
Murphy AP, Steele M, Dube SR et al (2014) Adverse childhood experiences (ACEs) questionnaire and adult attachment interview (AAI): implications for parent child relationships. Child Abuse and Neglect 38(2):224–233. https://doi.org/10.1016/j.chiabu.2013.09.004
McLennan JD, MacMillan HL, Afifi TO (2020) Questioning the use of adverse childhood experiences (ACEs) questionnaires. Child Abuse Negl 101:104331. https://doi.org/10.1016/j.chiabu.2019.104331
Anda RF, Porter LE, Brown DW (2020) Inside the adverse childhood experience score: strengths, limitations, and misapplications. Am J Prev Med 59(2):293–295. https://doi.org/10.1016/j.amepre.2020.01.009
Progovac AM, Mullin BO, Dunham E et al (2020) Disparities in suicidality by gender identity among medicare beneficiaries. Am J Prev Med 58(6):789–798. https://doi.org/10.1016/j.amepre.2020.01.004
Heritage B, Rees CS, Hegney DG (2018) The ProQOL-21: A revised version of the professional quality of life (ProQOL) scale based on Rasch analysis. PLoS ONE 13(2):e0193478. https://doi.org/10.1371/journal.pone.0193478
Renkiewicz GK, Hubble MW (2022) Secondary traumatic stress in emergency services systems project: quantifying the effect of personal trauma profiles on Lifetime prevalence of suicidality in emergency medical services personnel. Air Med J 41(5):463–472. https://doi.org/10.1016/j.amj.2022.04.002
Buchanan DB (2023). The professional quality of life scale – 5 (ProQOL). NovoPsych. Retrieved April 28, 2023, from https://novopsych.com.au/assessments/clinician-self-assessment/the-professional-quality-of-life-scale-5-proqol/
Weiss D, Marmar C (2018) Impact of event scale – revised (IES-R) for DSM-IV. Retrieved April 28, 2023, from https://www.ptsd.va.gov/professional/assessment/adult-sr/ies-r.asp#:~:text=The%20IES%2DR%20is%20a,distress%20caused%20by%20traumatic%20events
Stamm BH (2010) The concise ProQOL Manual, 2nd edn. ProQOL.org, Pocatello, ID
Petrino R, Riesgo LG, Yilmaz B (2022) Burnout in emergency medicine professionals after 2 years of the COVID-19 pandemic: a threat to the healthcare system? Eur J Emerg Med 29(4):279–284. https://doi.org/10.1097/MEJ.0000000000000952
Lawrence JA, Davis BA, Corbette T, Hill EV, Williams DR, Reede JY (2022) Racial/ethnic differences in burnout: a systematic review. J Racial Ethn Health Disparities 9(1):257–269. https://doi.org/10.1007/s40615-020-00950-0
Cantor JC, Mouzon DM (2020) Are Hispanic, Black, and Asian physicians truly less burned out than White physicians? Individual and Institutional Considerations. JAMA Netw Open 3(8):e2013099. https://doi.org/10.1001/jamanetworkopen.2020.13099
Garcia LC, Shanafelt TD, West CP et al (2020) Burnout, depression, career satisfaction, and work-life integration by physician race/ethnicity. JAMA Network Open 3(8):e2012762. Published 2020 Aug 3. https://doi.org/10.1001/jamanetworkopen.2020.1276
Maslach C, Leiter MP (2016) Understanding the burnout experience: recent research and - its implications for psychiatry. World Psychiatry: official journal of the World Psychiatric Association (WPA) 15(2):103–111. https://doi.org/10.1002/wps.20311
Almutairi MN, El Mahalli AA (2020) Burnout and coping methods among emergency medical services professionals. J Multidiscip Healthc 13:271–279. https://doi.org/10.2147/JMDH.S244303
Nikitha K, Menon BA (2020) Association of physician burnout with suicidal ideation and medical errors. JAMA Network Open. Retrieved April 9, 2023, from https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2773831
Bakusic J, Ghosh M, Polli A et al (2021) Role of NR3C1 and SLC6A4 methylation in the HPA axis regulation in burnout. J Affect Disord 295:505–512. https://doi.org/10.1016/j.jad.2021.08.081
Koutsimani P, Montgomery A, Georganta K (2019) The relationship between burnout, depression, and anxiety: a systematic review and meta-analysis. Front Psychol 10. https://doi.org/10.3389/fpsyg.2019.00284
Renkiewicz GK, Hubble MW (2021) Secondary traumatic stress in emergency services systems (STRESS) project: quantifying and predicting compassion fatigue in emergency medical services personnel. Prehosp Emerg Care 26(5):652–663. https://doi.org/10.1080/10903127.2021.1943578
Renkiewicz GK, Hubble MW (2021) Secondary traumatic stress in emergency services systems (STRESS) project: quantifying personal trauma profiles for secondary stress syndromes in emergency medical services personnel with prior military service. J Spec Oper Med 21(1):55. https://doi.org/10.55460/ao3y-hy3w
Renkiewicz GK, Hubble MW (2023) Secondary trauma response in emergency services systems (STRESS) project: quantifying and predicting vicarious trauma in emergency medical services personnel. Br Paramed J 7(4):23–34. https://doi.org/10.29045/14784726.2023.3.7.4.23
Nyklícek I, Pop VJ (2005) Past and familial depression predict current symptoms of professional burnout. J Affect Disord 88(1):63–68. https://doi.org/10.1016/j.jad.2005.06.007
Jackson DB, Testa A, Semenza DC, Vaughn MG (2021) Parental incarceration, child adversity, and child health: a strategic comparison approach. Int J Environ Res Public Health 18(7):3384. https://doi.org/10.3390/ijerph18073384
Murray J, Farrington D, Sekol I (2012) Children’s antisocial behavior, mental health, drug use, and educational performance after parental incarceration: a systematic review and meta-analysis. Psychol Bull 138(2):175–210
Bhutani J, Bhutani S, Balhara YP, Kalra S (2012) Compassion fatigue and burnout amongst clinicians: a medical exploratory study. Indian J Psychol Med 34(4):332–337. https://doi.org/10.4103/0253-7176.108206
American Ambulance Association. 2022 EMS employee turnover study. Accessed 5 May 2023: https://ambulance.org/2022/10/17/4th-annual-study-shows-worsening-ems-turnover/
Acknowledgements
The authors would like to acknowledge participating EMS agencies for their contribution to this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kaplan, G.R., Frith, T. & Hubble, M.W. Quantifying the prevalence and predictors of burnout in emergency medical services personnel. Ir J Med Sci (2023). https://doi.org/10.1007/s11845-023-03580-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11845-023-03580-7