Abstract
Background
The (derived) neutrophil-to-lymphocyte ratio (dNLR) is a potential predictive biomarker in the era of checkpoint inhibitors (CPI). An elevated dNLR is associated with worse outcomes across several malignancies. However, there is no clearly defined cut-off in the clinical setting.
Aim
To compare outcomes in patients prescribed CPI with a baseline dNLR0 > 3 and dNLR0 ≤ 3. The dNLR6 was measured 6 weeks later to determine its impact on patient overall survival (OS).
Methods
Prospectively maintained pharmacy databases in a regional cancer centre were interrogated for patients who were prescribed CPI in the advanced setting between January 2017 and May 2020.
Results
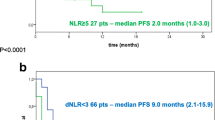
There were 121 patients with advanced cancer and a median age of 68 (range 30 to 88) years. Forty-four percent (n = 53) received prior systemic therapy. Patients with an initial dNLR0 > 3 when compared with a dNLR0 ≤ 3 had significantly shorter median progression-free survival (PFS), 3 vs. 14 months (p = 0.001) and median OS, 6.4 vs. 30.2 months (p = 0.001). Patients with an initial dNLR0 > 3 and increased dNLR at 6 weeks (dNLR6) had significantly reduced median PFS (3.5 vs. 14.7 months, p = 0.03) and OS (5.7 vs. 16.3, p = 0.03) when compared with those whose dNLR decreased. In the dNLR0 ≤ 3 cohort, any increased dNLR when compared with decreased dNLR after 6 weeks of CPI had significantly reduced PFS (8.4 months vs. NR, p = 0.01) and OS (24.2 months vs. NR, p = 0.02).
Conclusions
Lower pre-CPI treatment dNLR is associated with improved OS. A decrease in dNLR during treatment confers improved OS.


Similar content being viewed by others
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Herbst RS, Baas P, Kim DW et al (2016) Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet 387(10027):1540–1550
Reck M, Rodriguez-Abreu D, Robinson AG et al (2016) Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med 375(19):1823–1833
Rosenberg JE, Hoffman-Censits J, Powles T et al (2016) Atezolizumab in patients with locally advanced and metastatic urothelial carcinoma who have progressed following treatment with platinum-based chemotherapy: a single-arm, multicentre, phase 2 trial. Lancet 387(10031):1909–1920
Garon EB, Rizvi NA, Hui R et al (2015) Pembrolizumab for the treatment of non-small-cell lung cancer. N Engl J Med 372(21):2018–2028
Bellmunt J, de Wit R, Vaughn DJ et al (2017) Pembrolizumab as second-line therapy for advanced urothelial carcinoma. N Engl J Med 376(11):1015–1026
Schmid P, Adams S, Rugo HS et al (2018) Atezolizumab and nab-paclitaxel in advanced triple-negative breast cancer. N Engl J Med 379(22):2108–2121
Routy B, Le Chatelier E, Derosa L et al (2018) Gut microbiome influences efficacy of PD-1-based immunotherapy against epithelial tumors. Science 359(6371):91–97
Hellmann MD, Ciuleanu TE, Pluzanski A et al (2018) Nivolumab plus ipilimumab in lung cancer with a high tumor mutational burden. N Engl J Med 378(22):2093–2104
Capone M, Giannarelli D, Mallardo D et al (2018) Baseline neutrophil-to-lymphocyte ratio (NLR) and derived NLR could predict overall survival in patients with advanced melanoma treated with nivolumab. J Immunother Cancer 6(1):74
Templeton AJ, McNamara MG, Seruga B et al (2014) Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst 106(6):dju124
Petrova MP, Eneva MI, Arabadjiev JI et al (2020) Neutrophil to lymphocyte ratio as a potential predictive marker for treatment with pembrolizumab as a second line treatment in patients with non-small cell lung cancer. Biosci Trends 14(1):48–55
Rosner S, Kwong E, Shoushtari AN et al (2018) Peripheral blood clinical laboratory variables associated with outcomes following combination nivolumab and ipilimumab immunotherapy in melanoma. Cancer Med 7(3):690–697
Lalani AA, Xie W, Martini DJ et al (2018) Change in neutrophil-to-lymphocyte ratio (NLR) in response to immune checkpoint blockade for metastatic renal cell carcinoma. J Immunother Cancer 6(1):5
Kiriu T, Yamamoto M, Nagano T et al (2018) The time-series behavior of neutrophil-to-lymphocyte ratio is useful as a predictive marker in non-small cell lung cancer. PLoS One 13(2):e0193018
Cupp MA, Cariolou M, Tzoulaki I et al (2020) Neutrophil to lymphocyte ratio and cancer prognosis: an umbrella review of systematic reviews and meta-analyses of observational studies. BMC Med 18(1):360
Bigot F, Castanon E, Baldini C et al (2017) Prospective validation of a prognostic score for patients in immunotherapy phase I trials: the Gustave Roussy Immune Score (GRIm-Score). Eur J Cancer 84:212–218
Mezquita L, Auclin E, Ferrara R et al (2018) Association of the lung immune prognostic index with immune checkpoint inhibitor outcomes in patients with advanced non-small cell lung cancer. JAMA Oncol 4(3):351–357
Kazandjian D, Gong Y, Keegan P et al (2019) Prognostic value of the lung immune prognostic index for patients treated for metastatic non-small cell lung cancer. JAMA Oncol
Acknowledgements
Participating cancer patients and the UHW pharmacy department.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to this manuscript, read, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mullally, W.J., Greene, J., Jordan, E.J. et al. The prognostic value of the derived neutrophil-to-lymphocyte ratio (dNLR) in patients treated with immune checkpoint inhibitors. Ir J Med Sci 192, 83–87 (2023). https://doi.org/10.1007/s11845-022-02982-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-022-02982-3