Abstract
Background
To the best of our knowledge, no other studies investigated acute myocardial infarction patients’ beliefs and knowledge level after the discharge education.
Aims
The aim of the study was to investigate the effectiveness of planned discharge education on the beliefs and knowledge levels of CVD risk factors, medication compliance, dietary compliance, and individual follow-up in patients with acute myocardial infarction (AMI).
Methods
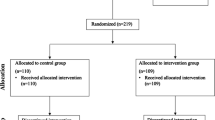
A double-blind randomized controlled study was carried out with 100 AMI patients. All participants were randomly assigned to the intervention (n = 50) and control groups (n = 50). The first evaluation of all participants in both groups was on the day of discharge. Both groups were re-evaluated after 4 weeks. Patients’ beliefs on medication, diet, and individual monitoring were assessed by the Beliefs about Medication Compliance Scale (BMCS), the Beliefs about Dietary Compliance Scale (BDCS), and the Beliefs about Individual Follow-up Scale (BIFS), respectively. The knowledge of CVD risk factors was questioned with the Cardiovascular Disease Risk Factors Knowledge Level (CARRF-KL) Scale.
Results
The mean age of the patients was 59.10 ± 9.38 years in the intervention group and 58.86 ± 9.19 in the control group. After the planned discharge education, beliefs and knowledge levels of CVD risk factors, medication compliance, dietary compliance, and individual follow-up were significantly increased compared with the control group.
Conclusion
Planned discharge education had a positive effect on the knowledge level of cardiovascular diseases risk factors, drug compliance, nutritional compliance, and individual follow-up in patients with acute myocardial infarction.

Similar content being viewed by others
Availability of data and material
All data generated or analyzed during this study are included in this published article.
References
Balakumar P, Maung-U K, Jagadeesh G (2016) Prevalence and prevention of cardiovascular disease and diabetes mellitus. Pharmacol Res 113:600–609
Roth GA, Johnson C, Abajobir A et al (2017) Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol 70(1):1–25
Souza PALd, Marcadenti A, Portal VL (2017) Effects of olive oil phenolic compounds on inflammation in the prevention and treatment of coronary artery disease. Nutrients 9(10):1087
Angell SY, McConnell MV, Anderson CAM et al (2020) The American Heart Association 2030 impact goal: a presidential advisory from the American Heart Association. Circulation 141(9):e120–e138
Nabel EG, Braunwald E (2012) A tale of coronary artery disease and myocardial infarction. N Engl J Med 366(1):54–63
Okrainec K, Banerjee DK, Eisenberg MJ (2004) Coronary artery disease in the developing world. Am Heart J 148(1):7–15
White HD, Chew DP (2008) Acute myocardial infarction. The Lancet 372(9638):570–584
Čulić V (2007) Acute risk factors for myocardial infarction. Int J Cardiol 117(2):260–269
Millett ERC, Peters SAE, Woodward M (2018) Sex differences in risk factors for myocardial infarction: cohort study of UK Biobank participants. bmj 363:k4247
Yandrapalli S, Nabors C, Goyal A et al (2019) Modifiable risk factors in young adults with first myocardial infarction. J Am Coll Cardiol 73(5):573–584
Bradley SM, Borgerding JA, Wood GB et al (2019) Incidence, risk factors, and outcomes associated with in-hospital acute myocardial infarction. JAMA network open 2(1):e187348–e187348
Sebregts E, Falger PRJ, Bär F (2000) Risk factor modification through nonpharmacological interventions in patients with coronary heart disease. J Psychosom Res 48(4–5):425–441
Hajar R (2017) Risk factors for coronary artery disease: historical perspectives. Heart views: the official journal of the Gulf Heart Association 18(3):109
Newby LK, Eisenstein EL, Califf RM et al (2000) Cost effectiveness of early discharge after uncomplicated acute myocardial infarction. N Engl J Med 342(11):749–755
Cao Y, Davidson PM, DiGiacomo M (2009) Cardiovascular disease in China: an urgent need to enhance the nursing role to improve health outcomes. J Clin Nurs 18(5):687–693
Camm AJ, Lüscher TF, Serruys PW (2009) The ESC textbook of cardiovascular medicine. OXFORD university press
Goddard L, Hill MC, Morton A (2015) Caring for patients after myocardial infarction. Practice nursing 26(6):288–294
Smith J, Liles C (2007) Information needs before hospital discharge of myocardial infarction patients: a comparative, descriptive study. J Clin Nurs 16(4):662–671
Froelicher ES, Kee LL, Newton KM et al (1994) Return to work, sexual activity, and other activities after acute myocardial infarction. Heart & lung: the journal of critical care 23(5):423–435
McMartin K (2013) Discharge planning in chronic conditions: an evidence-based analysis. Ontario health technology assessment series 13(4):1
Abbaszadeh A, Borhani F, Asadi N (2011) Effects of health belief model-based video training about risk factors on knowledge and attitude of myocardial infarction patients after discharge. Journal of research in medical sciences: the official journal of Isfahan University of Medical Sciences 16(2):195
Ebrahimi H, Abbasi A, Bagheri H et al (2020) The role of peer support education model on the quality of life and self-care behaviors of patients with myocardial infarction. Patient Education and Counseling
Faul F, Erdfelder E, Buchner A, Lang A-G (2009) Statistical power analyses using G* Power 3.1: tests for correlation and regression analyses. Behavior research methods 41 (4):1149–1160
Faul F, Erdfelder E, Lang A-G, Buchner A (2007) G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39(2):175–191
Bennett SJ, Milgrom LB, Champion V, Huster GA (1997) Beliefs about medication and dietary compliance in people with heart failure: an instrument development study. Heart Lung 26(4):273–279
Oðuz S, Enç N, Yiðit Z (2010) Adaptation of the compliance and belief scales to Turkish for patients with chronic heart failure. Archives of the Turkish Society of Cardiology 38(7):480–485
Arikan I, Metintaş S, Kalyoncu C, Yildiz Z (2009) The cardiovascular disease risk factors knowledge level (CARRF-KL) scale: a validity and reliability study. Turk Kardiyoloji Dernegi Arsivi: Turk Kardiyoloji Derneginin Yayin Organidir 37(1):35–40
Cafagna G, Seghieri C (2017) Educational level and 30-day outcomes after hospitalization for acute myocardial infarction in Italy. BMC Health Serv Res 17(1):18
Rajpura JR, Nayak R (2014) Role of illness perceptions and medication beliefs on medication compliance of elderly hypertensive cohorts. J Pharm Pract 27(1):19–24
Ayraler A, Akan H, Kaspar EÇ et al (2012) Compliance of patients admitted to the cardiology outpatient clinic with the recommendations regarding cardiac risk factors. Journal of Academic Research in Medicine 2:59–63
Köseoğlu N, Enç N (2016) Investigation of factors that prevent medication compliance in individuals with chronic heart failure
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study was carried out in accordance with the ethical principles, and the Helsinki Declaration. Informed consent of the patients was obtained. The study protocol was approved by the local ethics committee of Manisa Celal Bayar University Faculty of Medicine (No. 20.478.486-332). The study protocol was registered (ClinicalTrials.gov Identifier: NCT03985397).
Consent to participate
Informed consent of the patients was obtained.
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Tuna, S., Pakyüz, S.Ç. The effectiveness of planned discharge education on health knowledge and beliefs in patients with acute myocardial infarction: a randomized controlled trial. Ir J Med Sci 191, 691–698 (2022). https://doi.org/10.1007/s11845-021-02601-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-021-02601-7