Abstract
Background
There is contradictory evidence regarding the merits of restricted versus liberal perioperative intravenous (IV) fluid administration in bowel surgery. This study sought to audit perioperative fluid management in elective colectomy in Ireland and to analyse the impact of such on operative outcomes.
Methods
A national surgical trainee collaborative audit of perioperative fluid management was performed. Data from each site was collected prospectively over a selected 3-week period within a pre-defined 2-month block. Collected variables included demographics, type of operation/anaesthethic, volume/type of fluid administration pre-, intra- and post-operatively, 30-day morbidity and mortality. Primary outcome was fluid balance 24-h post-operatively with further analysis to identify the impact of this on 30-day morbidity. ROC curves were generated to identify the critical volume at which fluid balance was associated with 30-day morbidity.
Results
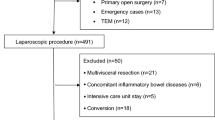
Ninety-four patients were enrolled from 17 hospitals. Mean age was 64 years. A total of 48.9% (N = 46) were managed by ERAS and 51.1% (N = 48) received bowel preparation. Almost 70% of cases (N = 63) were completed by minimally invasive techniques. Significant 30-day morbidity requiring hospital readmission was low [6.4% (n = 6)]. Median fluid balance at 24 h was + 715 ml (IQR 165–1486 ml). On multivariate analysis, high BMI (p = 0.02), indication for surgery (p = 0.02) and critical care admission (p = 0.008) were significantly predictive of 30-day morbidity. Twenty-four hour fluid balance >+ 665 ml was associated with increased risk of 30-day morbidity on univariate but not multivariate analysis, implying association but not causation.
Conclusion
Overall, perioperative fluid management was within an acceptable range with minimal impact on 30-day morbidity following elective colorectal surgery.


Similar content being viewed by others
Change history
03 July 2019
The above article originally published with Christina Fleming and Irish Surgical Research Collaborative listed in the authorship line.
References
https://www.ncri.ie/sites/ncri/files/factsheets/colorectal.pdf
Burke JP, Coffey JC, Boyle E, Keane F, McNamara DA (2013) Early outcomes for rectal cancer surgery in the republic of Ireland following a national centralization program. Ann Surg Oncol 20(11):3414–3421
Jones DW, Finlayson SR (2010) Trends in surgery for Crohn's disease in the era of infliximab. Ann Surg 252:307–312
Wind J, Polle SW, Fung Kon Jin PH, Dejong CH, von Meyenfeldt MF, Ubbink DT, Gouma DJ, Bemelman WA, Laparoscopy and/or Fast Track Multimodal Management Versus Standard Care (LAFA) Study Group, Enhanced Recovery after Surgery (ERAS) Group (2006) Systematic review of enhanced recovery programmes in colonic surgery. Br J Surg 93(7):800–809
The Impact of Enhanced Recovery Protocol Compliance on Elective Colorectal Cancer Resection 2015 Results from an international registry. Ann Surg.
Nisanevich V, Felsenstein I, Almogy G, Weissman C, Einav S, Matot I (2005) Effect of intraoperative fluid management on outcome after intraabdominal surgery. Anesthesiology. 103(1):25–32
Lobo DN, Bostock KA, Neal KR, Perkins AC, Rowlands BJ, Allison SP (2002) Effect of salt and water balance on recovery of gastrointestinal function after elective colonic resection: a randomised controlled trial. Lancet. 359(9320):1812–1818
Brandstrup B, Tonnesen H, Beier-Holgersen R, Hjortso E, Ording H, Lindorff-Larsen K et al (2003) Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: a randomized assessor-blinded multicenter trial. Ann Surg 238(5):641–648
Kalyan JP, Rosbergen M, Pal N, Sargen K, Fletcher SJ, Nunn DL et al (2013) Randomized clinical trial of fluid and salt restriction compared with a controlled liberal regimen in elective gastrointestinal surgery. Br J Surg 100(13):1746–1747
Bedi SS, Hetz R, Thomas C, Smith P, Olsen AB, Williams S, Xue H, Aroom K, Uray K, Hamilton J, Mays RW, Cox CS Jr (2013) Intravenous multipotent adult progenitor cell therapy attenuates activated microglial/macrophage response and improves spatial learning after traumatic brain injury. Stem Cells Transl Med 2:953–960
Boesen AK, Maeda Y, Rorbaek Madsen M. Perioperative fluid infusion and its influence on anastomotic leakage after rectal cancer surgery: implications for prevention strategies
Bundgaard-Nielsen M, Secher NH, Kehlet H (2009) 'Liberal' vs. 'restrictive' perioperative fluid therapy--a critical assessment of the evidence. Acta Anaesthesiol Scand 53:843–851
Boland MR, Noorani A, Varty K, Coffey JC, Agha R, Walsh SR (2013) Perioperative fluid restriction in major abdominal surgery: systematic review and meta-analysis of randomized, clinical trials. World J Surg 37(6):1193–1202
Myles PS, Bellomo R, Corcoran T, Forbes A, Peyton P, Story D, Christophi C, Leslie K, McGuinness S, Parke R, Serpell J, Chan MTV, Painter T, McCluskey S, Minto G, Wallace S (2018) Restrictive versus Liberal fluid therapy for major abdominal surgery. N Engl J Med 378:2263–2274. https://doi.org/10.1056/NEJMoa1801601. [Epub ahead of print]
Chong PC, Greco EF, Stothart D, Maziak DE, Sundaresan S, Shamji FM et al (2009) Substantial variation of both opinions and practice regarding perioperative fluid resuscitation. Can J Surg 52:207–214
G D, Bartlett DC, Futaba K, Whisker L, Pinkney TD, West Midlands Research Collaborative (2014) (WMRC), Birmingham, UK. BMC med Educ. How to set up and manage a trainee-led research collaborative. BMC Med Educ 14:94
CholeS study group, west midlands research Collaborative (2016) Population-based cohort study of outcomes following cholecystectomy for benign gallbladder diseases. Br J Surg 103(12):1704–1715
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 370:1453–1457
Lee SY, Kang SB, Kim DW, Oh HK, Ihn MH (2015) Risk factors and preventive measures for acute urinary retention after rectal cancer surgery. World J Surg 39(1):275–282
Boesen AK, Maeda Y, Rorbaek Madsen M (2013) Perioperative fluid infusion and its influence on anastomotic leakage after rectal cancer surgery: implications for prevention strategies. Color Dis 15(9):e522–e527
Lobo DN, Macafee DA, Allison SP (2006) How perioperative fluid balance influences postoperative outcomes. Best Pract Res Clin Anaesthesiol 20(3):439–455
Conway DH, Mayall R, Abdul-Latif MS, Gilligan S, Tackaberry C (2002) Randomised controlled trial investigating the influence of intravenous fluid titration using oesophageal Doppler monitoring during bowel surgery. Anaesthesia 57:845–849
Wakeling HG, McFall MR, Jenkins CS, Woods WG, Miles WF (2005) Barclay GR et al. intraoperative oesophageal Doppler guided fluid management shortens postoperative hospital stay after major bowel surgery. Br J Anaesth 95:634–642
Noblett SE, Snowden CP, Shenton BK, Horgan AF (2006) Randomized clinical trial assessing the effect of Doppler-optimized fluid management on outcome after elective colorectal resection. Br J Surg 93:1069–1076
Srinivasa S, Kahokehr A, Soop M, Taylor M, Hill AG (2013) Goal-directed fluid therapy- a survey of anaesthetists in the UK, USA, Australia and New Zealand. BMC anaesthesiology 13:5
Group TCOoSTS (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059
Kennedy GD, Heise C, Rajamanickam V, Harms B, Foley EF (2009) Laparoscopy decreases postoperative complication rates after abdominal colectomy: results from the national surgical quality improvement program. Ann Surg 249:596–601
Author information
Authors and Affiliations
Consortia
Ethics declarations
Ethical approval was sought prospectively from each regional clinical ethics committee prior to commencing data collection. Authorship was assigned in keeping with the Association of Surgeons in Training (ASiT)/National Research Collaborative (NRC) authorship model.
Conflict of interest
Nil
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: The above article originally published with Christina Fleming and Irish Surgical Research Collaborative listed in the authorship line. Christina Fleming’s name was included in error by the Publisher, and should have instead been included in the Collaborators section.
Appendix
Appendix
Pre-operative | |
|---|---|
MRN (for data collection only) | |
Age (years) | |
Gender | |
ASA | |
Indication | |
Admission date | |
Enhanced recovery (Y/N) | |
Pre-op weight (kg) | |
BMI | |
Diabetic (Y/N) | |
Baseline creatinine | |
Baseline haemoglobin | |
Baseline diuretic Type Dose | |
IV fluid preop Type Volume | |
Pre-op bowel prep (Y/N) Type | |
Intra-operative | |
Date of surgery | |
Time of induction | |
Time of skin closure | |
Lap/converted/open/robotic | |
Operation | |
Operation duration (min) | |
General anaesthesia (Y/N) | |
Spinal anaesthesia (Y/N) | |
Epidural (Y/N) | |
Cannula Size Number | |
Urinary catheter | |
Goal-directed fluid therapy (Y/N) Type | |
Oesophageal Doppler use (Y/N) | |
IV fluids Type Volume | |
Blood products Type Volume | |
Intra-op urinary output | |
Intra-op blood loss (ml) | |
Intra-op complications (Y/N) Type | |
Inotropes (Y/N) | |
Post-op day 1 | |
POD1 fluid balance (ml) | |
Total post op fluid input (ml) | |
Total post op fluid output (ml) | |
Weight (kg) | |
IV fluid post op to 24 h Type Volume | |
Blood products post op to 24 h Type Volume | |
Enteral fluid input post-op to 24 h Tpye Volume | |
Urinary output POD-24 h (ml) | |
GI output POD-24 h (ml) | |
Stoma (Y/N) Volume POD-24 h | |
Creatinine day 1 | |
Post-op diuretic Type Dose | |
Post-op day 30 | |
HDU (Y/N)–planned (Y/N) | |
ICU (Y/N)–planned (Y/N) | |
Total LOS (days) | |
High output stoma (Y/N) | |
Renal compromise from HOS (Y/N) | |
Return to theatre (Y/N) | |
Time to return to oral fluids (POD) | |
Time to return to oral diet (POD) | |
Time to passing flatus (POD) | |
Time to BO (POD) | |
30-day morbidity (Y/N) | |
Specific morbidity | |
Clavien-Dindo grade | |
Complication description | |
All cause 30-day ED attendance | |
All cause 30-day re-admission | |
All cause 30-day mortality | |
Cause of death |
Rights and permissions
About this article
Cite this article
Irish Surgical Research Collaborative. PERioperative Fluid Management in Elective ColecTomy (PERFECT)—a national prospective cohort study. Ir J Med Sci 188, 1363–1371 (2019). https://doi.org/10.1007/s11845-019-02003-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-019-02003-w