Abstract
Purpose
Sexual health is important for quality of life among older (≥65 years) cancer survivors. Yet, little is known about the extent to which their sexual health has been studied.
Methods
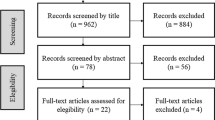
In this integrative review, PubMed, PsycINFO, CINAHL, and Web of Science were searched for data-based articles of sexual health among older cancer survivors. Using a matrix, study characteristics, including cancer types and areas of sexual health, were categorized.
Results
The sample included 82 articles (81 studies). The areas of sexual health were categorized into sexual function, body image, sexual function-related distress, sexual health-related quality of life, sexual activity, sexual enjoyment, and sexual desire. Most targeted prostate cancer (n = 56, 69.1%) and studied sexual function, e.g., erectile function (n = 53, 94.6%). Body image (n = 16, 19.8%) was next frequently studied, targeting women with breast cancer. Measures to assess areas of sexual health, largely unstandardized, varied widely. Generally, older cancer survivors reported negative changes in sexual function and other areas during and after cancer treatment.
Conclusions
Studies of sexual health among older cancer survivors have been focused primarily on prostate cancer, male, and sexual function. Together with the lack of standardized sexual health measures validated for older adults, this narrow research focus contributes to the limited body of knowledge regarding sexual health among older cancer survivors.
Implications for Cancer Survivors
Given that cancer and cancer treatment affect both men and women and many aspects of sexual health beyond functioning, broadening the scope of sexual health and cancer type is warranted for future research.

Similar content being viewed by others
Data availability
Because this review conducted a narrative synthesis of existing studies, no datasets were generated.
References
Gallicchio L, Tonorezos E, de Moor JS, Elena J, Farrell M, Green P, et al. Evidence gaps in cancer survivorship care: a report from the 2019 National Cancer Institute Cancer Survivorship Workshop. J Natl Cancer Inst. 2021;113(9):1136–42. https://doi.org/10.1093/jnci/djab049.
Miller KD, Nogueira L, Mariotto AB, Rowland JH, Yabroff KR, Alfano CM, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019;69(5):363–85. https://doi.org/10.3322/caac.21565.
Scotte F, Bossi P, Carola E, Cudennec T, Dielenseger P, Gomes F, et al. Addressing the quality of life needs of older patients with cancer: a SIOG consensus paper and practical guide. Ann Oncol. 2018;29(8):1718–26. https://doi.org/10.1093/annonc/mdy228.
Bober SL, Varela VS. Sexuality in adult cancer survivors: challenges and intervention. J Clin Oncol. 2012;30(30):3712–9. https://doi.org/10.1200/jco.2012.41.7915.
Carter J, Lacchetti C, Andersen BL, Barton DL, Bolte S, Damast S, et al. Interventions to address sexual problems in people with cancer: American Society of Clinical Oncology clinical practice guideline adaptation of Cancer Care Ontario Guideline. J Clin Oncol. 2018;36(5):492–511. https://doi.org/10.1200/jco.2017.75.8995.
Seguin L, Touzani R, Bouhnik AD, Charif AB, Marino P, Bendiane MK, et al. Deterioration of sexual health in cancer survivors five years after diagnosis: data from the French national prospective VICAN survey. Cancers. 2020;12(11) https://doi.org/10.3390/cancers12113453.
Falk SJ, Dizon DS. Sexual health issues in cancer survivors. Semin Oncol Nurs. 2020;36(1):150981. https://doi.org/10.1016/j.soncn.2019.150981.
World Health Organization. Measuring sexual health: conceptual and practical considerations and related indicators. Geneva, Switzerland: World Health Organization; 2010.
Kagan SH, Holland N, Chalian AA. Sexual issues in special populations: geriatric oncology - sexuality and older adults. Semin Oncol Nurs. 2008;24(2):120–6. https://doi.org/10.1016/j.soncn.2008.02.005.
Arthur EK, Worly B, Carpenter KM, Postl C, Rosko AE, Krok-Schoen JL, et al. Let’s get it on: addressing sex and intimacy in older cancer survivors. J Geriatr Oncol. 2021;12(2):312–5. https://doi.org/10.1016/j.jgo.2020.08.003.
Lindau ST, Schumm LP, Laumann EO, Levinson W, O’Muircheartaigh CA, Waite LJ. A study of sexuality and health among older adults in the United States. N Engl J Med. 2007;357(8):762–74. https://doi.org/10.1056/NEJMoa067423.
Kolodziejczak K, Rosada A, Drewelies J, Duzel S, Eibich P, Tegeler C, et al. Sexual activity, sexual thoughts, and intimacy among older adults: links with physical health and psychosocial resources for successful aging. Psychol Aging. 2019;34(3):389–404. https://doi.org/10.1037/pag0000347.
Sinković M, Towler L. Sexual aging: a systematic review of qualitative research on the sexuality and sexual health of older adults. Qual Health Res. 2019;29(9):1239–54. https://doi.org/10.1177/1049732318819834.
American Cancer Society. Cancer treatment & survivorship facts & figures 2019-2021. Atlanta: American Cancer Society; 2019.
Jackson SE, Firth J, Veronese N, Stubbs B, Koyanagi A, Yang L, et al. Decline in sexuality and wellbeing in older adults: a population-based study. J Affect Disord. 2019;245:912–7. https://doi.org/10.1016/j.jad.2018.11.091.
Ezhova I, Savidge L, Bonnett C, Cassidy J, Okwuokei A, Dickinson T. Barriers to older adults seeking sexual health advice and treatment: a scoping review. Int J Nurs Stud. 2020;107:103566. https://doi.org/10.1016/j.ijnurstu.2020.103566.
Haesler E, Bauer M, Fetherstonhaugh D. Sexuality, sexual health and older people: a systematic review of research on the knowledge and attitudes of health professionals. Nurse Educ Today. 2016;40:57–71. https://doi.org/10.1016/j.nedt.2016.02.012.
Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546–53. https://doi.org/10.1111/j.1365-2648.2005.03621.x.
Arraras JI, Manterola A, Illarramendi JJ, Asin G, de la Cruz S, Ibañez B, et al. Quality of life evolution in elderly survivors with localized breast cancer treated with radiotherapy over a three-year follow-up. Breast. 2018;41:74–81. https://doi.org/10.1016/j.breast.2018.06.010.
Arraras JI, Manterola A, Asin G, Illarramendi JJ, Cruz Sde L, Ibañez B, et al. Quality of life in elderly patients with localized breast cancer treated with radiotherapy. A prospective study. Breast. 2016;26:46–53. https://doi.org/10.1016/j.breast.2015.12.008.
Kikkawa K, Iba A, Kohjimoto Y, Noda Y, Sonomura T, Hara I. Impact of age on quality of life in patients with localized prostate cancer treated with high-dose rate brachytherapy combined with external beam radiotherapy. Int J Urol. 2018;25(4):366–71. https://doi.org/10.1111/iju.13530.
Wang E, Eriksson H. Quality of life and functional outcomes 10 years after laparoscopic radical prostatectomy. Upsala J Med Sci. 2014;119(1):32–7. https://doi.org/10.3109/03009734.2013.868560.
Ubrig B, Boy A, Heiland M, Roosen A. Outcome of robotic radical prostatectomy in men over 74. J Endourol. 2018;32(2):106–10. https://doi.org/10.1089/end.2017.0512.
Bhat SK, Moschovas M, Sandri M, Reddy S, Onol F, Noel J, et al. Stratification of potency outcomes following robot-assisted laparoscopic radical prostatectomy based on age, preoperative potency, and nerve sparing. J Endourol. 2021;35(11):1631–8. https://doi.org/10.1089/end.2021.0141.
Traboulsi S, Nguyen D, Zakaria A, Law K, Shahine H, Meskawi M, et al. Functional and perioperative outcomes in elderly men after robotic-assisted radical prostatectomy for prostate cancer. World J Urol. 2020;38(11):2791–8. https://doi.org/10.1007/s00345-020-03096-0.
Mandel P, Graefen M, Michl U, Huland H, Tilki D. The effect of age on functional outcomes after radical prostatectomy. Urol Oncol. 2015;33(5):203.e11–8. https://doi.org/10.1016/j.urolonc.2015.01.015.
Bhat SKR, Moschovas MC, Onol FF, Sandri M, Rogers T, Roof S, et al. Trends in clinical and oncological outcomes of robot-assisted radical prostatectomy before and after the 2012 US Preventive Services Task Force recommendation against PSA screening: a decade of experience. BJU Int. 2020;125(6):884–92. https://doi.org/10.1111/bju.15051.
Kumar A, Samavedi S, Bates A, Giedelman CC, Coelho R, Rocco B, et al. Age stratified comparative analysis of perioperative, functional and oncologic outcomes in patients after robot assisted radical prostatectomy--a propensity score matched study. Eur J Surg Oncol. 2015;41(7):837–43. https://doi.org/10.1016/j.ejso.2015.04.006.
Gurung PMS, Wang B, Hassig S, Wood J, Ellis E, Feng C, et al. Oncological and functional outcomes in patients over 70 years of age treated with robotic radical prostatectomy: a propensity-matched analysis. World J Urol. 2021;39(4):1131–40. https://doi.org/10.1007/s00345-020-03304-x.
Jayadevappa R, Chhatre S, Whittington R, Bloom B, Wein A, Malkowicz S. Health-related quality of life and satisfaction with care among older men treated for prostate cancer with either radical prostatectomy or external beam radiation therapy. BJU Int. 2006;97(5):955–62. https://doi.org/10.1111/j.1464-410X.2006.06128.x.
Litwin M, Melmed G, Nakazon T. Life after radical prostatectomy: a longitudinal study. J Urol. 2001;166(2):587–92.
Namiki S, Ishidoya S, Kawamura S, Tochigi T, Arai Y. Quality of life among elderly men treated for prostate cancer with either radical prostatectomy or external beam radiation therapy. J Cancer Res Clin Oncol. 2010;136(3):379–86. https://doi.org/10.1007/s00432-009-0665-6.
Namiki S, Ishidoya S, Tochigi T, Ito A, Arai Y. Quality of life after radical prostatectomy in elderly men. Int J Urol. 2009;16(10):813–9. https://doi.org/10.1111/j.1442-2042.2009.02371.x.
Sánchez-Ortiz R, Broderick G, Rovner E, Wein A, Whittington R, Malkowicz S. Erectile function and quality of life after interstitial radiation therapy for prostate cancer. Int J Impot Res. 2000;12:S18–24. https://doi.org/10.1038/sj.ijir.3900557.
Hampson LA, Cowan JE, Zhao S, Carroll PR, Cooperberg MR. Impact of age on quality-of-life outcomes after treatment for localized prostate cancer. Eur Urol. 2015;68(3):480–6. https://doi.org/10.1016/j.eururo.2015.01.008.
Namiki S, Tochigi T, Kuwahara M, Ioritani N, Yoshimura K, Terai A, et al. Recovery of health related quality of life after radical prostatectomy in Japanese men: a longitudinal study. Int J Urol. 2004;11(9):742–9. https://doi.org/10.1111/j.1442-2042.2004.00881.x.
Hu JC, Elkin EP, Pasta DJ, Lubeck DP, Kattan MW, Carroll PR, et al. Predicting quality of life after radical prostatectomy: results from CaPSURE. J Urol. 2004;171(2):703–8. https://doi.org/10.1097/01.ju.0000107964.61300.f6.
Kelović V, Buković D, Badzek S, Curić Z, Kelović Z, Persec Z, et al. Sex or surgery--erectile dysfunction after radical treatment of localized prostate cancer. Coll Antropol. 2009;33(2):529–32.
Merrick GS, Butler WM, Wallner KE, Galbreath RW, Anderson RL, Kurko BS, et al. Erectile function after prostate brachytherapy. Int J Radiat Oncol Biol Phys. 2005;62(2):437–47. https://doi.org/10.1016/j.ijrobp.2004.10.001.
Peters M, van Son M, Moerland M, Kerkmeijer L, Eppinga W, Meijer R, et al. MRI-guided ultrafocal HDR brachytherapy for localized prostate cancer: median 4-year results of a feasibility study. Int J Radiat Oncol Biol Phys. 2019;104(5):1045–53. https://doi.org/10.1016/j.ijrobp.2019.03.032.
Wortel R, Pos F, Heemsbergen W, Incrocci L. Sexual function after hypofractionated versus conventionally fractionated radiotherapy for prostate cancer: results from the randomized phase III HYPRO trial. J Sex Med. 2016;13(11):1695–703. https://doi.org/10.1016/j.jsxm.2016.08.012.
Shigeta K, Kikuchi E, Matsushima M, Ogihara K, Kosaka T, Mizuno R, et al. Relationship between radiation doses and erectile function deterioration in patients with localized prostate cancer treated with permanent prostate brachytherapy. Int J Urol. 2020;27(12):1087–93. https://doi.org/10.1111/iju.14358.
Adam S, Martin-Diener E, Camey B, Egger HC, Konzelmann I, Mohsen MS, et al. Health-related quality of life in long-term prostate cancer survivors after nerve-sparing and non-nerve-sparing radical prostatectomy-results from the multiregional PROCAS study. Cancer Med. 2020;9(15):5416–24. https://doi.org/10.1002/cam4.3197.
Lebret T, Culine S, Davin J, Hennequin C, Mignard J, Moreau J, et al. Quality of life of 1276 elderly patients with prostate cancer, starting treatment with a gonadotropin-releasing hormone agonist: results of a French observational study. Aging Male. 2014;17(2):87–93. https://doi.org/10.3109/13685538.2014.891013.
Maenhout M, Peters M, Moerland MA, Meijer RP, van den Bosch M, Frank SJ, et al. MRI guided focal HDR brachytherapy for localized prostate cancer: toxicity, biochemical outcome and quality of life. Radiother Oncol. 2018;129(3):554–60. https://doi.org/10.1016/j.radonc.2018.07.019.
Vernooij R, Cremers R, Jansen H, Somford D, Kiemeney L, van Andel G, et al. Urinary incontinence and erectile dysfunction in patients with localized or locally advanced prostate cancer: a nationwide observational study. Urologic Oncology. 2020;38(9):735.e17–25. https://doi.org/10.1016/j.urolonc.2020.05.022.
Shahait M, Dobbs R, Kim J, Eldred N, Liang K, Huynh L, et al. Perioperative and functional outcomes of robot-assisted radical prostatectomy in octogenarian men. J Endourol. 2021;35(7):1025–9. https://doi.org/10.1089/end.2020.0859.
Fowler F Jr, Barry M, Lu-Yao G, Wasson J, Roman A, Wennberg J. Effect of radical prostatectomy for prostate cancer on patient quality of life: results from a Medicare survey. Urology. 1995;45(6):1007–13. https://doi.org/10.1016/s0090-4295(99)80122-8.
Fowler F Jr, Barry M, Lu-Yao G, Wasson J, Bin L. Outcomes of external-beam radiation therapy for prostate cancer: a study of Medicare beneficiaries in three surveillance, epidemiology, and end results areas. J Clin Oncol. 1996;14(8):2258–65. https://doi.org/10.1200/JCO.1996.14.8.2258.
Fowler F Jr, McNaughton CM, Walker CE, Elliott D, Barry M. The impact of androgen deprivation on quality of life after radical prostatectomy for prostate carcinoma. Cancer. 2002;95(2):287–95. https://doi.org/10.1002/cncr.10656.
Stanford JL, Feng Z, Hamilton AS, Gillil FD, Stephenson RA, et al. Urinary and sexual function after radical prostatectomy for clinically localized prostate cancer The Prostate Cancer Outcomes Study. JAMA. 2000;283(3):354–60. https://doi.org/10.1001/jama.283.3.354.
Jønler M, Nielsen OS, Wolf H. Urinary symptoms, potency, and quality of life in patients with localized prostate cancer followed up with deferred treatment. Urology. 1998;52(6):1055–62. https://doi.org/10.1016/S0090-4295(98)00449-X.
Catalona WJ, Carvalhal GF, Mager DE, Smith DS. Potency, continence and complication rates in 1,870 consecutive radical retropubic prostatectomies. J Urology. 1999;162(2):433–8.
Kundu SD, Roehl KA, Eggener SE, Antenor JA, Han M, Catalona WJ. Potency, continence and complications in 3,477 consecutive radical retropubic prostatectomies. J Urology. 2004;172(6):2227–31. https://doi.org/10.1097/01.ju.0000145222.94455.73.
Potters L, Torre T, Fearn PA, Leibel SA, Kattan MW. Potency after permanent prostate brachytherapy for localized prostate cancer. Int J Radiat Oncol Biol Phys. 2001;50(5):1235–42. https://doi.org/10.1016/s0360-3016(01)01578-4.
Labanaris AP, Witt JH, Zugor V. Robotic-assisted radical prostatectomy in men ≥75 years of age. Surgical, oncological and functional outcomes. Anticancer Res. 2012;32(5):2085–9.
Rabbani F, Stapleton AM, Kattan MW, Wheeler TM, Scardino PT. Factors predicting recovery of erections after radical prostatectomy. J Urol. 2000;164(6):1929–34.
Hoffman R, Barry M, Stanford J, Hamilton A, Hunt W, Collins M. Health outcomes in older men with localized prostate cancer: results from the Prostate Cancer Outcomes Study. Am J Med. 2006;119(5):418–25. https://doi.org/10.1016/j.amjmed.2005.06.072.
Arraras JI, Illarramendi JJ, Manterola A, Asin G, Salgado E, Arrondo P, et al. Quality of life in elderly breast cancer patients with localized disease receiving endocrine treatment: a prospective study. Clin Transl Oncol. 2019;21(9):1231–9. https://doi.org/10.1007/s12094-019-02048-4.
Arraras JI, Manterola A, Domínguez MA, Arias F, Villafranca E, Romero P, et al. Impact of radiotherapy on the quality of life of elderly patients with localized breast cancer. A prospective study. Clin Transl Oncol. 2008;10(8):498–504. https://doi.org/10.1007/s12094-008-0239-0.
Bantema-Joppe EJ, de Bock GH, Woltman-van Iersel M, Busz DM, Ranchor AV, Langendijk JA, et al. The impact of age on changes in quality of life among breast cancer survivors treated with breast-conserving surgery and radiotherapy. Br J Cancer. 2015;112(4):636–43. https://doi.org/10.1038/bjc.2014.632.
Browall MM, Ahlberg KM, Persson LO, Karlsson PO, Danielson EB. The impact of age on health-related quality of life (HRQoL) and symptoms among postmenopausal women with breast cancer receiving adjuvant chemotherapy. Acta Oncol. 2008;47(2):207–15. https://doi.org/10.1080/02841860701621258.
Williams LJ, Kunkler IH, King CC, Jack W, van der Pol M. A randomised controlled trial of post-operative radiotherapy following breast-conserving surgery in a minimum-risk population. Quality of life at 5 years in the PRIME trial. Health Technol Assess. 2011;15(12):i–xi, 1-57. https://doi.org/10.3310/hta15120.
Perrone F, Nuzzo F, Di Rella F, Gravina A, Iodice G, Labonia V, et al. Weekly docetaxel versus CMF as adjuvant chemotherapy for older women with early breast cancer: final results of the randomized phase III ELDA trial. Ann Oncol. 2015;26(4):675–82. https://doi.org/10.1093/annonc/mdu564.
Mari G, Costanzi A, Galfrascoli E, Rosato A, Crippa J, Maggioni D. Prospective evaluation of genito-urinary function after laparoscopic rectal resection in the elderly. Chir Buchar. 2016;111(4):318–25.
Orsini R, Thong M, van de Poll-Franse L, Slooter G, Nieuwenhuijzen G, Rutten H, et al. Quality of life of older rectal cancer patients is not impaired by a permanent stoma. Eur J Surg Oncol. 2013;39(2):164–70. https://doi.org/10.1016/j.ejso.2012.10.005.
Schmidt CE, Bestmann B, Kuchler T, Longo WE, Kremer B. Impact of age on quality of life in patients with rectal cancer. World J Surg. 2005;29(2):190–7. https://doi.org/10.1007/s00268-004-7556-4.
Kamga AM, Bengrine-Lefevre L, Quipourt V, Favier L, Darut-Jouve A, Marilier S, et al. Long-term quality of life and sexual function of elderly people with endometrial or ovarian cancer. Health Qual Life Outcomes. 2021;19(1):56. https://doi.org/10.1186/s12955-021-01675-2.
Ganz P, Schag C, Heinrich R. The psychosocial impact of cancer on the elderly: a comparison with younger patients. J Am Geriatr Soc. 1985;33(6):429–35. https://doi.org/10.1111/j.1532-5415.1985.tb07154.x.
Figueiredo M, Cullen J, Hwang Y, Rowland J, Mandelblatt J. Breast cancer treatment in older women: does getting what you want improve your long-term body image and mental health? J Clin Oncol. 2004;22(19):4002–9. https://doi.org/10.1200/JCO.2004.07.030.
de Haes JC, Curran D, Aaronson NK, Fentiman IS. Quality of life in breast cancer patients aged over 70 years, participating in the EORTC 10850 randomised clinical trial. Eur J Cancer. 2003;39(7):945–51. https://doi.org/10.1016/s0959-8049(03)00149-7.
Zhang H, Hu H, Huang R, Guan Z, Zheng M, Xu C, et al. Natural orifice specimen extraction surgery versus conventional laparoscopic-assisted resection for colorectal cancer in elderly patients: a propensity-score matching study. Updates Surg. 2022;74(2):599–607. https://doi.org/10.1007/s13304-021-01143-y.
MacDonald L, Anderson H. Stigma in patients with rectal cancer: a community study. J Epidemiol Community Health. 1984;38(4):284–90. https://doi.org/10.1136/jech.38.4.284.
Nordin A, Dixon S, Chinn D, Moloney I, Naik R, De Barros LA, et al. Attitudes to radical gynecological oncology surgery in the elderly: a pilot study. Int J Gynecol Cancer. 2000;10(4):323–9. https://doi.org/10.1046/j.1525-1438.2000.010004323.x.
Nordin A, Chinn D, Moloney I, Naik R, Lopes A, Monaghan J, et al. Do elderly cancer patients care about cure? Attitudes to radical gynecologic oncology surgery in the elderly. Gynecol Oncol. 2001;81(3):447–55. https://doi.org/10.1006/gyno.2001.6178.
Zhang X, Pennell M, Bernardo B, Clark J, Krok-Schoen J, Focht B, et al. Body image, physical activity and psychological health in older female cancer survivors. J Geriatr Oncol. 2021;12(7):1059–67. https://doi.org/10.1016/j.jgo.2021.04.007.
Posielski N, Frankel J, Kuo H, Ho O, Elsamanoudi S, Nousome D, et al. Impact of age and race on health-related quality of life outcomes in patients undergoing radical prostatectomy for localized prostate cancer. Urology. 2022;163:99–106. https://doi.org/10.1016/j.urology.2021.07.034.
Barry MJ, Gallagher PM, Skinner JS, Fowler FJ Jr. Adverse effects of robotic-assisted laparoscopic versus open retropubic radical prostatectomy among a nationwide random sample of Medicare-age men. J Clin Oncol. 2012;30(5):513–8. https://doi.org/10.1200/jco.2011.36.8621.
Hollenbeck B, Dunn R, Wei J, McLaughlin P, Han M, Sanda M. Neoadjuvant hormonal therapy and older age are associated with adverse sexual health-related quality-of-life outcome after prostate brachytherapy. Urology. 2002;59(4):480–4. https://doi.org/10.1016/s0090-4295(01)01664-8.
Ramsey S, Hall I, Smith J, Ekwueme D, Fedorenko C, Kreizenbeck K, et al. A comparison of general, genitourinary, bowel, and sexual quality of life among long term survivors of prostate, bladder, colorectal, and lung cancer. J Geriatr Oncol. 2021;12(2):305–11. https://doi.org/10.1016/j.jgo.2020.07.014.
Muss HB, Tu D, Ingle JN, Martino S, Robert NJ, Pater JL, et al. Efficacy, toxicity, and quality of life in older women with early-stage breast cancer treated with letrozole or placebo after 5 years of tamoxifen: NCIC CTG intergroup trial MA.17. J Clin Oncol. 2008;26(12):1956–64. https://doi.org/10.1200/jco.2007.12.6334.
Kornblith AB, Powell M, Regan MM, Bennett S, Krasner C, Moy B, et al. Long-term psychosocial adjustment of older vs younger survivors of breast and endometrial cancer. Psycho-Oncology. 2007;16(10):895–903. https://doi.org/10.1002/pon.1146.
Paterson C, Kata S, Nandwani G, Chaudhury DD, Nabi G. Unmet supportive care needs of men with locally advanced and metastatic prostate cancer on hormonal treatment: a mixed methods study. Cancer Nurs. 2017;40(6):497–507. https://doi.org/10.1097/NCC.0000000000000482.
Mols F, Schoormans D, Smit J, Netea-Maier R, Links T, van der Graaf W, et al. Age-related differences in health-related quality of life among thyroid cancer survivors compared with a normative sample: Results from the PROFILES Registry. Head Neck. 2018;40(10):2235–45. https://doi.org/10.1002/hed.25325.
Fowler F Jr, Barry M, Lu-Yao G, Roman A, Wasson J, Wennberg J. Patient-reported complications and follow-up treatment after radical prostatectomy. The National Medicare Experience: 1988-1990 (updated June 1993). Urology. 1993;42(6):622–9. https://doi.org/10.1016/0090-4295(93)90524-e.
van Andel G, Bottomley A, Fosså SD, Efficace F, Coens C, Guerif S, et al. An international field study of the EORTC QLQ-PR25: a questionnaire for assessing the health-related quality of life of patients with prostate cancer. Eur J Cancer. 2008;44(16):2418–24. https://doi.org/10.1016/j.ejca.2008.07.030.
Sprangers M, Groenvold M, Arraras JI, Franklin J, te Velde A, Muller M, et al. The European Organization for Research and Treatment of Cancer breast cancer-specific quality-of-life questionnaire module: first results from a three-country field study. J Clin Oncol. 1996;14(10):2756–68.
Ganesh V, Agarwal A, Popovic M, Cella D, McDonald R, Vuong S, et al. Comparison of the FACT-C, EORTC QLQ-CR38, and QLQ-CR29 quality of life questionnaires for patients with colorectal cancer: a literature review. Support Care Cancer. 2016;24:3661–8. https://doi.org/10.1007/s00520-016-3270-7.
Litwin MS, Hays RD, Fink A, Ganz PA, Leake B, Brook RH. The UCLA prostate cancer index: development, reliability, and validity of a health-related quality of life measure. Med Care. 1998;36(7):1002–12.
Shen C, Jain K, Shah T, Schaefer E, Zhou S, Fried D, et al. Relationships between erectile dysfunction, prostate cancer treatment type and inflatable penile prosthesis implantation. Investig Clin Urol. 2022;63(3):316–24. https://doi.org/10.4111/icu.20210445.
Hu J, Gu X, Lipsitz S, Barry M, D’Amico A, Weinberg A, et al. Comparative effectiveness of minimally invasive vs open radical prostatectomy. J Am Med Assoc. 2009;302(14):1557–64. https://doi.org/10.1001/jama.2009.1451.
Sun M, Abdollah F, Hansen J, Trinh Q, Bianchi M, Tian Z, et al. Is a treatment delay in radical prostatectomy safe in individuals with low-risk prostate cancer? J Sex Med. 2012;9(11):2961–9. https://doi.org/10.1111/j.1743-6109.2012.02806.x.
Sussman R, Carvalho F, Harbin A, Zheng C, Lynch J, Stamatakis L, et al. Survival and secondary interventions following treatment for locally-advanced prostate cancer. Can J Urol. 2018;25(5):9516–24.
Hu JC, Gold KF, Pashos CL, Mehta SS, Litwin MS. Temporal trends in radical prostatectomy complications from 1991 to 1998. J Urol. 2003;169(4):1443–8. https://doi.org/10.1097/01.ju.0000056046.16588.e4.
Adejoro O, Gupta P, Ziegelmann M, Weight C, Konety B. Effect of minimally invasive radical prostatectomy in older men. Urol Oncol. 2016;34(5):234.e1–11. https://doi.org/10.1016/j.urolonc.2015.11.016.
Roberts C, Jang T, Shao Y, Kabadi S, Moore D, Lu-Yao G. Treatment profile and complications associated with cryotherapy for localized prostate cancer: a population-based study. Prostate Cancer Prostatic Dis. 2011;14(4):313–9. https://doi.org/10.1038/pcan.2011.17.
Anderson CB, Elkin EB, Atoria CL, Eastham JA, Scardino PT, Touijer K. The diffusion of minimally invasive radical prostatectomy in the United States: a case study of the introduction of new surgical devices. Prostate Cancer Prostatic Dis. 2015;18(1):75–80. https://doi.org/10.1038/pcan.2014.49.
Bekelman JE, Mitra N, Efstathiou J, Liao K, Sunderland R, Yeboa DN, et al. Outcomes after intensity-modulated versus conformal radiotherapy in older men with nonmetastatic prostate cancer. Int J Radiat Oncol Biol Phys. 2011;81(4):e325–34. https://doi.org/10.1016/j.ijrobp.2011.02.006.
Jiang R, Tomaszewski J, Ward K, Uzzo R, Canter D. The burden of overtreatment: comparison of toxicity between single and combined modality radiation therapy among low risk prostate cancer patients. Can J Urol. 2015;22(1):7648–55.
Muise A, Pan MM, Rose B, Buckley JC. Functional outcomes after prostate cancer treatment: a comparison between single and multiple modalities. Urol Oncol. 2023;41(2):104.e1–9. https://doi.org/10.1016/j.urolonc.2022.07.014.
Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Peña BM. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11(6):319–26. https://doi.org/10.1038/sj.ijir.3900472.
Wei JT, Dunn RL, Litwin MS, Sandler HM, Sanda MG. Development and validation of the expanded prostate cancer index composite (EPIC) for comprehensive assessment of health-related quality of life in men with prostate cancer. Urology. 2000;56(6):899–905. https://doi.org/10.1016/s0090-4295(00)00858-x.
Garcia-Rodelas L, Martinez-Bordajandi A, Puga-Mendoza A, Hernandez-Padilla J, Jimenez-Lasserrotte M, Fernandez-Sola C, et al. Quality of life in elderly men after a radical prostatectomy: a qualitative study. J Mens Health. 2023;19(1):7–14. https://doi.org/10.22514/jomh.2023.004.
Mortensen G, Jakobsen J. Patient perspectives on quality of life after penile cancer. Dan Med J. 2013;60(7):A4655.
Gupta N, Rasmussen S, Haney N, Smith A, Pierorazio P, Johnson M, et al. Understanding psychosocial and sexual health concerns among women with bladder cancer undergoing radical cystectomy. Urology. 2021;151:145–53. https://doi.org/10.1016/j.urology.2020.08.018.
Hilditch JR, Lewis J, Peter A, van Maris B, Ross A, Franssen E, et al. A menopause-specific quality of life questionnaire: development and psychometric properties. Maturitas. 1996;24(3):161–75. https://doi.org/10.1016/s0378-5122(96)82006-8.
U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute, 2023. https://www.cdc.gov/cancer/dataviz. Accessed July 12, 2023.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49. https://doi.org/10.3322/caac.21660.
Cherven B, Sampson A, Bober SL, Bingen K, Frederick N, Freyer DR, et al. Sexual health among adolescent and young adult cancer survivors: a scoping review from the Children’s Oncology Group Adolescent and Young Adult Oncology Discipline Committee. CA Cancer J Clin. 2021;71(3):250–63. https://doi.org/10.3322/caac.21655.
Lehmann V, Laan ETM, den Oudsten BL. Sexual health-related care needs among young adult cancer patients and survivors: a systematic literature review. J Cancer Surviv. 2022;16(4):913–24. https://doi.org/10.1007/s11764-021-01084-w.
Lundberg PC, Phoosuwan N. Life situations of Swedish women after mastectomy due to breast cancer: a qualitative study. Eur J Oncol Nurs. 2022;57:102116. https://doi.org/10.1016/j.ejon.2022.102116.
Rowland E, Metcalfe A. A systematic review of men’s experiences of their partner’s mastectomy: coping with altered bodies. Psycho-Oncology. 2014;23(9):963–74. https://doi.org/10.1002/pon.3556.
Almont T, Bouhnik A-D, Ben Charif A, Bendiane M-K, Couteau C, Manceau C, et al. Sexual health problems and discussion in colorectal cancer patients two years after diagnosis: a national cross-sectional study. J Sex Med. 2019;16(1):96–110. https://doi.org/10.1016/j.jsxm.2018.11.008.
Petersén C, Carlsson E. Life with a stoma-coping with daily life: experiences from focus group interviews. J Clin Nurs. 2021;30(15-16):2309–19. https://doi.org/10.1111/jocn.15769.
Günaydin Y, Kılıç Z, Zincir H, Tutar N. The effect of dyspnea and fatigue on sexual life and marital satisfaction individuals with chronic obstructive pulmonary disease. Sex Disabil. 2022;40(1):153–65. https://doi.org/10.1007/s11195-022-09725-3.
Stulz A, Lamore K, Montalescot L, Favez N, Flahault C. Sexual health in colon cancer patients: a systematic review. Psycho-Oncology. 2020;29(7):1095–104. https://doi.org/10.1002/pon.5391.
O’Brien R, Rose P, Campbell C, Weller D, Neal R, Wilkinson C, et al. “I wish I’d told them”: a qualitative study examining the unmet psychosexual needs of prostate cancer patients during follow-up after treatment. Patient Educ Couns. 2011;84(2):200–7. https://doi.org/10.1016/j.pec.2010.07.006.
Lindau S, Surawska H, Paice J, Baron S. Communication about sexuality and intimacy in couples affected by lung cancer and their clinical-care providers. Psycho-Oncology. 2011;20(2):179–85. https://doi.org/10.1002/pon.1787.
Grunfeld EA, Halliday A, Martin P, Drudge-Coates L. Andropause syndrome in men treated for metastatic prostate cancer: a qualitative study of the impact of symptoms. Cancer Nurs. 2012;35(1):63–9. https://doi.org/10.1097/NCC.0b013e318211fa92.
Brüggemann J. Redefining masculinity - men’s repair work in the aftermath of prostate cancer treatment. Health Sociol Rev. 2021;30(2):143–56. https://doi.org/10.1080/14461242.2020.1820367.
Kelemen A, Cagle J, Chung J, Groninger H. Assessing the impact of serious illness on patient intimacy and sexuality in palliative care. J Pain Symptom Manag. 2019;58(2):282–8. https://doi.org/10.1016/j.jpainsymman.2019.04.015.
Kelemen A, Van Gerven C, Mullins K, Groninger H. Sexuality and intimacy needs within a hospitalized palliative care population: results from a qualitative study. Am J Hosp Palliat Med. 2022;39(4):433–7. https://doi.org/10.1177/10499091211036928.
Alwaal A, Breyer BN, Lue TF. Normal male sexual function: emphasis on orgasm and ejaculation. Fertil Steril. 2015;104(5):1051–60. https://doi.org/10.1016/j.fertnstert.2015.08.033.
Freak-Poli R. It’s not age that prevents sexual activity later in life. Australas J Ageing. 2020;39 Suppl 1(Suppl 1):22–9. https://doi.org/10.1111/ajag.12774.
Walker LM, Wiebe E, Turner J, Driga A, Andrews-Lepine E, Ayume A, et al. The oncology and sexuality, intimacy, and survivorship program model: an integrated, multi-disciplinary model of sexual health care within oncology. J Cancer Educ. 2021;36(2):377–85. https://doi.org/10.1007/s13187-019-01641-z.
Acknowledgements
This study was supported by the Center for Nursing Excellence in Palliative Care at Emory University Nell Hodgson Woodruff School of Nursing, but the content is solely the responsibility of the authors. The authors would like to thank Ms. Sharon Leslie, a nursing informationist at Emory University Woodruff Health Sciences Center Library, for her assistance with the search string development.
Funding
The authors declare that no funds or grants were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. H.L. performed literature search and data analysis, wrote the first draft of the manuscript, and critically revised the work. M.K.S. supervised this study throughout the preparation of the manuscript. The authors reviewed and edited previous versions of the manuscript and read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
As this review did not involve human or animal subjects, ethics approval was not required.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, H., Song, MK. State of the science of sexual health among older cancer survivors: an integrative review. J Cancer Surviv (2024). https://doi.org/10.1007/s11764-024-01541-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11764-024-01541-2