Abstract
Objectives
We investigated current mechanisms causing low graft flow (LGF) following coronary artery bypass grafting, particularly for the right coronary artery (RCA).
Methods
We retrospectively assessed 230 individual bypass grafts as the sole bypass graft for the RCA using preoperative and postoperative quantitative angiography. Overall, 155 in-situ gastroepiploic arteries (GEAs) and 75 saphenous vein grafts (SVGs) were included. The size and status of the revascularised area were examined to determine whether these factors were associated with LGF (defined as ≤ 20 mL/min with intraoperative flowmetry). A distal lesion was defined as stenosis at segment #4, whereas a proximal lesion was stenosis at #1, #2 and #3.
Results
Graft flow in the SVG and the GEA for distal lesion was significantly less compared with that for proximal lesion (34 ± 26 vs. 60 ± 46, p < 0.0001 and 22 ± 12 vs. 43 ± 28, p = 0.0004, respectively). For proximal lesion, LGF was significantly more frequent when the minimal luminal diameter was over 1.27 compared with when it was less than 1.27 (p = 0.02). Prior myocardial infarction significantly correlated with LGF in the GEA (p = 0.007) and the SVG (p = 0.03). In 55 bypass grafts with LGF, the causes were competitive flow in 20.0%, small revascularised area in 38.1% and prior myocardial infarction in 32.7%.
Conclusions
Along with the current strategy based on the severity of native coronary stenosis, the incidence of competitive flow decreased remarkably. This resulted in flow demand, myocardial status and collateral vessels more influential on graft patency.
Similar content being viewed by others
Introduction
Intraoperative transit time flowmetry (TTFM) is useful not only for detecting technical errors but also for short and midterm patency [1, 2] following coronary artery bypass grafting (CABG). Competitive flow is caused by moderate stenosis of the native coronary artery and is most commonly found in the right coronary artery (RCA) region [3]; it was considered as the most important mechanism for arterial graft failure [4]. Recently, preoperative assessment of native coronary stenosis, such as fractional flow reserve (FFR) has been improving. FFR, calculated using intraluminal pressure, was considered reliable for the detection of functional ischaemia due to moderate stenosis before percutaneous coronary intervention and CABG.
In the present study, we examined the severity of target coronary artery stenosis and clinical history of the revascularised area to determine the underlying mechanisms for low graft flow (LGF) and the impact of flow demand or peripheral vasculature on graft flow and patency; we also assessed the causes of LGF in cases of bypass graft to the RCA in the present decade.
Subjects
We reviewed the clinical records and angiograms of 230 patients with 771 bypass grafts who underwent off-pump CABG and postoperative catheter coronary angiograms from July 2007 to December 2015. The study population comprised 175 men and 55 women with a mean age of 67 ± 10 years (Table 1). Patients who had a bypass graft that were individual and created as the sole bypass graft for the RCA region were selected for this study. The selected grafts comprised 155 in-situ gastroepiploic artery (GEA) grafts and 75 aorto-coronary saphenous vein grafts (SVG) to the RCA. To minimise bias, other graft materials, such as the radial artery, internal thoracic artery and composite or sequential grafts, were excluded. This retrospective observational study was approved by our institutional review board that waived the requirement for written informed consent of the patients.
Methods
Our standard procedure involving off-pump CABG and SVG or GEA was used for RCA revascularisation. At study initiation, we preferred to use arterial grafts, irrespective of the stenosis severity. In the later period, FFR was introduced in our institution. The use of aorto-coronary SVG has been on the rise in our institute, especially for RCA with moderate stenosis. Quantitative coronary angiography had been performed before CABG surgery for all patients of bypass grafts, measuring the minimal luminal diameter (MLD) at the narrowest stenotic lesion proximal to the anastomotic site, and its reference diameter. Stenosis at #1–3 was defined as a proximal lesion, while that at #4 was defined as a distal lesion. History of percutaneous coronary intervention (PCI) was defined as any catheter procedure for treating RCA stenosis or occlusion, even if the treatment was unsuccessful. Myocardial infarction (MI) was defined as the presence of Q-wave on electrocardiogram and asynergy on echocardiography in the inferior area or diagnosis by a cardiologist. Graft flow was measured after all the anastomotic manoeuvres were completed and the heart had returned to the normal position. The blood pressure was usually > 100 mmHg systolic arterial pressure with a minimal dose of inotropic agents. LGF was defined as mean flow ≤ 20 mL/min, as measured by intraoperative TTFM (Medi-stim, Oslo, Norway). When we identified a significant difference in the incidence of LGF between the higher and lower values, we defined the value with the lowest p value as the cuff-off MLD. As previously reported, LGF significantly correlates with future graft failure of the GEA and the SVG [5].
All these patients underwent postoperative coronary angiography. Cardiologists independently evaluated the severity of native coronary artery stenosis and anatomical and functional graft patency. Competitive flow was defined when a target coronary branch was slightly opacified by antegrade flow from graft injection, and the bypass graft was clearly opacified by retrograde flow from coronary injection. Graft failure was defined as occlusion or string sign by catheter selective angiography. String sign was defined as diffuse narrowing of the graft. The mean interval between CABG surgery and angiography was 1.5 ± 5.1 months, and less than 1 month in 93% of these patients.
Statistical analyses
We have expressed continuous variables as mean ± standard deviation values and compared them using unpaired Student’s t test. We compared the data of two independent groups with the χ2 test. The mean duration of follow-up was 11.4 ± 14.6 months. We considered the differences in the outcomes to be statistically significant when the p value was < 0.05.
Results
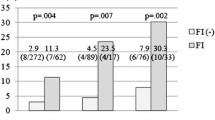
Graft flow in the SVG for the distal lesion was significantly less than that for the proximal lesion (34 ± 26 vs. 60 ± 46, p = 0.0004). Graft flow in the GEA for the distal lesion was significantly less than that for the proximal lesion (22 ± 12 vs. 43 ± 28, p < 0.0001). LGF developed in 55/230 (23.9%) bypass grafts, and there were 28/230 (12.2%) graft failures. With respect to the GEA, the incidence of LGF was 17.4% and that of graft failure was 13.5%. For the SVG, the incidence of LGF was 20.0% and that of graft failure was 9.3%. The incidence of LGF according to the characteristics of the target vessel, bypass graft, revascularised area and prior MI and PCI is shown in Table 2. For GEA to the RCA and SVG to the RCA, the incidence of LGF was significantly higher in patients with prior MI in the RCA region (p = 0.007 for GEA and p = 0.03 for SVG). The incidence of LGF was significantly higher for distal lesion as compared to that for the proximal lesion in the GEA (p = 0.001) and the SVG (p = 0.0004).
The reference diameters and cut-off MLD are shown in Table 3. For GEA to the RCA, the cut-off MLD was 1.27 for proximal stenosis, while no cut-off value was identified for distal stenosis. The incidence of LGF was 50.0% for distal stenosis, irrespective of the severity of stenosis. No cut-off value was identified in the SVG for proximal and distal lesions.
The hypothesised primary causes of LGF in bypass grafts to the RCA area are listed in Table 4. Competitive flow purely attributable to moderate stenosis was observed in 11 grafts (18.8%). Competitive flow was considered to be the primary cause of LGF in 9 of the 11 grafts until 2010. Prior MI in the RCA region with Q-wave and inferior asynergy were considered to be the causes of LGF in 18 cases. Extremely small revascularised areas, such as the stenosis located in the mid-portion of the posterior-descending branch, were considered to be the cause in 21 cases (Fig. 1, left). Abundant collaterals from an ectatic LCX were suspected in 4 (Fig. 1, right) patients, and a technical error was suspected in one patient. The cause of LGF was critical anastomotic stenosis for one bypass graft. This may be attributable to procedural failure of flow measurement.
Discussion
RCA dominant, indicating the posterior-descending branch from the RCA, is the most popular coronary anatomy [6, 7]. Coronary artery distribution was categorised as RCA dominant in 48–90% of the cases, left coronary artery dominant in 12.5–22% of the cases and balanced type (defined by the posterior-descending branch arising from both the right and left coronary artery) in 12–34% of the cases [7]. Dominance of the coronary artery significantly affects ventricular contraction and mortality following MI [8, 9]. Ortale and colleagues reported that even in a RCA dominant heart, 16% of the RCA did not have posterior left atrioventricular branch of the RCA [7]. In addition, there was no significant difference in the diameter of the posterior-descending branch between the RCA dominant and the balanced type [7]. The size of the area perfused by the RCA is quite individualised and can occasionally be small, even when the diameter is sufficient for anastomosis.
Collateral circulation is usually associated with a vessel with CTO or critical stenosis. It is widely believed that the development of collaterals mitigates MI and improves survival. Vessels with CTO are generally considered favourable targets for CABG. Caputo and colleagues have reported that patients with CTO usually have more advanced coronary vessel disease, history of MI and reduced left ventricular function, necessitating more targets for CABG [10]. However, these researchers also reported that in spite of differences in the severity and risks, midterm clinical results after off-pump CABG were similar in patients with and without collateral circulations [10]. Nathoe and colleagues have reported that the advantages of collateral circulation during off-pump CABG include myocardial protection and superior midterm results [11]. Few reports regarding fate and effect of collateral circulation after CABG exist. Kaku and co-researchers have shown that the presence of rich collateral circulation can reduce graft flow and increase the pulsatility index and that preoperative collateral vessels can disappear after ITA grafting [12]. Takami and colleagues reported that the disappearance of collateral vessels may depend on the anastomosis location of ITA to LAD [13]. Oshima and colleagues reported that Rentrop collateral classification is not associated with early graft failure, whereas akinetic or dyskinetic wall motion shows such an association [14].
Competitive flow usually results from native coronary flow due to moderate stenosis. Furthermore, competitive flow is considered the primary reason for graft failure associated with reduced graft flow. However, in current clinical practice, it can be avoided by reliable preoperative assessment of stenosis, appropriate selection of graft and creation of configuration [15, 16]. FFR was introduced, and it improved the accuracy of preoperative assessment. Honda and colleagues reported a decrease in the competitive flow using the strategy based on FFR [17]. Toth and colleagues reported better clinical outcomes with fewer distal anastomoses and probably fewer graft materials [18]. To achieve sufficient graft flow, not only avoidance of competitive flow, but also sufficient flow demand is necessary. Previously, we reported that more severe stenosis is necessary for distal stenosis compared to that for proximal stenosis [5].
In the present study, we assessed native coronary stenosis using the MLD, a simple structural and functional parameter of the native coronary artery. Moreover, TTFM is reliable in off-pump CABG [19] rather than in on-pump CABG because cardiopulmonary bypass can induce a hyperaemic state, creating a major bias in flow measurement [20]. Furthermore, to assess the impact of the size and status of the RCA area, only an individual bypass graft created as a sole bypass graft in the RCA area. The present study revealed that competitive flow simply attributable to moderately stenotic native targets was no longer the primary mechanism for LGF in the later period. Moreover, LGF was significantly associated with distal lesions and a history of MI in the RCA region. Previously, Borowski and colleagues reported that flow in the bypass grafts to totally occlude the RCA was significantly lower in the infarcted or the hypokinetic area [21]. However, as a secondary or underlying reason, the severity of native coronary stenosis might be associated with LGF occurrence. This study confirmed that graft flow and patency of the aorto-coronary SVG was influenced less by the stenosis severity, but significantly by the size of the revascularised area.
The present results suggest that the severity of the stenosis and the CABG strategy should be modified, depending on the stenosis location (distal or proximal) and the size of the revascularised area. In detail, GEA in an individual fashion should be preferably utilised for the RCA with proximal lesion and less than 1.27 mm of MLD to maintain long-term patency. When stenosis is located at the proximal portion and MLD is larger than the cut-off value, the aorto-coronary SVG is recommended. For distal lesion of the RCA, sequential grafting with the circumflex artery using either GEA or SVG would be a reasonable option, if there is a good target in the posterolateral area. For example, when the revascularised area of posterior-descending branch is small, sequential grafting to posterior-descending branch in a side-to-side fashion, and to circumflex branch with good run-off in an end-to-side fashion can be beneficial. Carrel and colleagues stated that the patency of the GEA was not always superior to that of the SVG for RCA; therefore, appropriate conduit selection would improve the overall graft patency [22].
This study had certain limitations. First, it was a retrospective observational study. Second, conditions for TTFM measurement, such as blood pressure and the dose of catecholamine were not strictly defined because flow measurement was performed in the clinical situation. Third, FFR may be a reliable modality of functional assessment for coronary artery stenosis. However, the data of FFR could not be considered for this study because it was not performed for all patients or introduced in all referral hospitals. In addition, FFR cannot be measured for the target with total occlusion, and is commonly biassed for the target as collateral source to the area of chronic total occlusion [23]. Fourth, we were unable to define clearly some factors as the causes of LGF, such as collateral circulation from the ectatic circumflex artery after bypass grafting. Collateral flow from the circumflex artery could not be reliably quantified and its postoperative fate would be unpredictable. Fifth, pulsatility index and diastolic filling were not taken into consideration because they did not significantly correlate with angiographic patency in our experience. Moreover, it is unclear whether parameters, such as pulsatility index or diastolic filling, have correlation with myocardial the size and status of revascularised area. Sixth, flow demand in the area with prior MI will correlate to the amount of remaining viability. Unfortunately, viability had not been preoperatively assessed by specific examinations. Seventh, technical failure or surgical skill might be the most significant bias, especially for CABG. In this study, most patients underwent postoperative angiography within a month to detect technical failure. However, such bias could not be completely eliminated. Finally, the complex mechanism of LGF might be suspected in some cases. However, the results confirmed that a decreasing trend in the competitive flow and increasing influence of flow demand is crucial.
To conclude, along with graft selection based on the severity of native coronary stenosis, the incidence of competitive flow decreased remarkably. This resulted in flow demand, myocardial status and collateral vessels more influential on graft flow and patency.
References
Lehnert P, Moller CH, Damgaard S, Gerds TA, Steinbruchel DA. Transit-time flow measurement as a predictor of coronary bypass graft failure at one year angiographic follow-up. J Card Surg. 2015;30:47–52.
Amin S, Pinho-Gomes AC, Taggart DP. Relationship of intraoperative transit time flowmetry findings to angiographic graft patency at follow-up. Ann Thorac Surg. 2016;101(5):1996–2006.
Nakajima H, Kobayashi J, Tagusari O, Bando K, Niwaya K, Kitamura S. Competitive flow in arterial composite grafts and effect of graft arrangement in off-pump coronary revascularization. Ann Thorac Surg. 2004;78:481–6.
Nakajima H, Kobayashi J, Toda K, Fujita T, Shimahara Y, Kasahara Y, Kitamura S. A 10-year angiographic follow-up of competitive flow in sequential and composite arterial grafts. Eur J Cardio-Thorac Surg. 2011;40:399–404.
Nakajima H, Iguchi A, Tabata M, Koike H, Morita K, Takahashi K, Asakura T, Nishimura S, Niinami H. Predictors and prevention of flow insufficiency due to limited flow demand. J Cardiothorac Surg. 2014;9:188.
Gupta T, Saini A, Sahni D. Terminal branching pattern of the right coronary artery in left-dominant hearts: a cadaveric study. Cardiovasc Pathol. 2013;22:179–82.
Ortale JR, Keiralla LCB, Sacilotto L. The posterior ventricular branches of the coronary arteries in the human heart. Arq Bras Cardiol. 2004;82:468–72.
Veltman CE, Hoogslag GE, Kharbanda RK, de Graaf MA, van Zwet EW, van der Hoeven BL, Delgado V, Bax JJ, Scholte A. Relation between coronary arterial dominance and left ventricular ejection fraction after ST-segment elevation acute myocardial infarction in patients having percutaneous coronary intervention. Am J Cardiol. 2014;114:1646e1650.
Goldberg A, Southern DA, Galbraith PD, Traboulsi M, Knudtson ML, Ghali WA. Coronary dominance and prognosis of patients with acute coronary syndrome. Am Heart J. 2007;154:1116–22.
Caputo M, Anis RR, Rogers CA, Ahmad N, Rizvi SIA, Baumbach A, Karsch KR, Angelini GD, Oberhoff M. Coronary collateral circulation: effect on early and midterm outcomes after off-pump coronary artery bypass surgery. Ann Thorac Surg. 2008;85:71–9.
Nathoe HM, Buskens E, Jansen EWL, Suyker WJL, Stella PR, Lahpor JR, van Boven WJ, van Dijk D, Diephuis JC, Borst C, Moons KGM, Grobbee DE, de Jaegere PPT. Role of coronary collaterals in off-pump and on-pump coronary bypass surgery. Circulation. 2004;110:1738–42.
Kaku D, Nakahira A, Hirai H, Sasaki Y, Hosono M, Bito Y, Suehiro Y, Suehiro S. Does rich coronary collateral circulation distal to chronically occluded left anterior descending artery compete with graft flow? Interact Cardiovasc Thorac Surg. 2013;17(6):944–9.
Takami Y, Masumoto H. Angiographic fate of collateral vessels after surgical revascularization of the totally occluded left anterior descending artery. Ann Thorac Surg. 2007;83:120–5.
Oshima H, Tokuda Y, Araki Y, Ishii H, Murohara T, Ozaki Y, Usui A. Predictors of early graft failure after coronary artery bypass grafting for chronic total occlusion. Interact Cardiovasc Thorac Surg. 2016;23:142–9.
Nakajima H, Kobayashi J, Toda K, Fujita T, Shimahara Y, Kasahara Y, Kitamura S. A 10-year angiographic follow-up of competitive flow in sequential and composite arterial grafts. Eur J Cardiothorac Surg. 2011;40(2):399–404.
Glineur D, Boodhwani M, Hanet C, de Kerchove L, Navarra E, Astarci P, Noirhomme P, El Khoury G. Bilateral internal thoracic artery configuration for coronary artery bypass surgery: a prospective randomized trial. Circ Cardiovasc Interv. 2016;9(7):e003518.
Honda K, Okamura Y, Nishimura Y, Uchita S, Yuzaki M, Kaneko M, Yamamoto N, Kubo T, Akasaka T. Graft flow assessment using a transit time flow meter in fractional flow reserve-guided coronary artery bypass surgery. J Thorac Cardiovasc Surg. 2015;149(6):1622–8.
Toth G, De Bruyne B, Casselman F, De Vroey F, Pyxaras S, Di Serafino L, Van Praet F, Van Mieghem C, Stockman B, Wijns W, Degrieck I, Barbato E. Fractional flow reserve-guided versus angiography-guided coronary artery bypass graft surgery. Circulation. 2013;128:1405–11.
Nakajima H, Iguchi A, Tabata M, Kambe M, Ikeda M, Uwabe K, Asakura T, Niinami H. Preserved autoregulation of coronary flow after off-pump coronary artery bypass grafting: retrospective assessment of intraoperative transit time flowmetry with and without intra-aortic balloon counterpulsation. J Cardiothorac Surg. 2016;11(1):156.
Balacumaraswami L, Abu-Omar Y, Selvanayagam J, Pigott D, Taggart DP. The effects of on-pump and off-pump coronary artery bypass grafting on intraoperative graft flow in arterial and venous conduits defined by a flow/pressure ratio. J Thorac Cardiovasc Surg. 2008;135(3):533–9.
Borowski A, Godehardt E, Dalyanoglu H. Surgical decision making for revascularization of chronically occluded right coronary artery. Gen Thorac Cardiovasc Surg. 2017;65:17–24.
Carrel T, Winkler B. Current trends in selection of conduits for coronary artery bypass grafting. Gen Thorac Cardiovasc Surg. 2017;65:549–56.
Iqbal MB, Shah N, Khan M, Wallis W. Reduction in myocardial perfusion territory and its effect on the physiological severity of a coronary stenosis. Circ Cardiovasc Interv. 2010;3:89–90.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Nakajima, H., Takazawa, A., Yoshitake, A. et al. Current mechanisms of low graft flow and conduit choice for the right coronary artery based on the severity of native coronary stenosis and myocardial flow demand. Gen Thorac Cardiovasc Surg 67, 655–660 (2019). https://doi.org/10.1007/s11748-019-01077-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-019-01077-8