Abstract
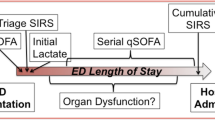
Using scoring systems in discreet microbiologic cohorts in a serial fashion to identify unique phenotypes of sepsis remains unknown. Single-center, retrospective study that screened adults who triggered the hospital’s SIRS (systemic inflammatory response syndrome) based sepsis alert into culture positive (Cx +) and culture negative (Cx−) groups. Subgroups were based on the location where the SIRS alert fired. SIRS scores and a novel score called SEP were calculated at t = 0 and at 3, 6, 12, and 24 h before and after t = 0. Primary outcome was a difference in SIRS/SEP scores in Cx + or Cx− groups over time. Secondary outcomes were differences in total SIRS/SEP scores and the components constituting SIRS/SEP scores at various locations over time. The study contained 7955 patients who met inclusion criteria. Cx + and Cx− groups had increases in SIRS/SEP scores and at similar rates starting 6 hours before t = 0. Both culture groups had decreasing SIRS/SEP scores, at varying gradients compared to the change in SIRS/SEP scores seen prior to t = 0. This pattern in SIRS/SEP scores before and after t = 0 was consistent in all location subgroups. Statistically significant differences were seen in the overall SIRS/SEP scores for Cx + and Cx− groups at hours 6, 12, and 24 after t = 0, in the ED group at t = 24 h after t = 0, the floor group at t = 0 h, and in the step-down group at t = 3 h after t = 0 h. Microbiological cohorting and serial assessments may be an effective tool to identify homogenous phenotypes of sepsis.





Similar content being viewed by others
References
Liu V, Escobar GJ, Greene JD et al (2014) Hospital deaths in patients with sepsis from 2 independent cohorts. JAMA 312(1):90–92
Rhee C, Dantes R, Epstein L, Murphy DJ, Seymour CW, Iwashyna TJ, Kadri SS, Angus DC, Danner RL, Fiore AE, Jernigan JA, Martin GS, Septimus E, Warren DK, Karcz A, Chan C, Menchaca JT, Wang R, Gruber S, Klompas M, CDC Prevention Epicenter Program (2017) Incidence and trends of sepsis in US hospitals using clinical vs claims data, 2009–2014. JAMA 318(13):1241–1249. https://doi.org/10.1001/jama.2017.13836
Annane D, Bellissant E, Cavaillon JM (2005) Septic shock. Lancet 365(9453):63–78. https://doi.org/10.1016/S0140-6736(04)17667-8
Shankar-Hari M, Phillips GS, Levy ML, Seymour CW, Liu VX, Deutschman CS, Angus DC, Rubenfeld GD, Singer M, Sepsis Definitions Task Force (2016) Developing a new definition and assessing new clinical criteria for septic shock: for the third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315(8):775–787. https://doi.org/10.1001/jama.2016.0289
Rhee C, Gohil S, Klompas M (2014) Regulatory mandates for sepsis care–reasons for caution. N Engl J Med 370(18):1673–1676. https://doi.org/10.1056/NEJMp1400276
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC (2016) The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315(8):801–810. https://doi.org/10.1001/jama.2016.0287
Kalantari A, Mallemat H, Weingart S (2017) Sepsis definitions: the search for gold and what CMS got wrong. West J Emerg Med 18(5):951–956
Seymour CW, Liu VX, Iwashyna TJ, Brunkhorst FM, Rea TD, Scherag A, Rubenfeld G, Kahn JM, Shankar-Hari M, Singer M, Deutschman CS, Escobar GJ, Angus DC (2016) Assessment of clinical criteria for sepsis: for the third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA 315(8):762–774. https://doi.org/10.1001/jama.2016.0288
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G (2003) SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Crit Care Med 31(4):1250–1256. https://doi.org/10.1097/01.CCM.0000050454.01978.3B
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 101(6):1644–1655. https://doi.org/10.1378/chest.101.6.1644
Brink A, Alsma J, Verdonschot RJCG, Rood PPM, Zietse R, Lingsma HF, Schuit SCE (2019) Predicting mortality in patients with suspected sepsis at the Emergency Department; a retrospective cohort study comparing qSOFA, SIRS and National Early Warning Score. PLoS ONE 14(1):e0211133. https://doi.org/10.1371/journal.pone.0211133.PMID:30682104;PMCID:PMC6347138
Seymour CW, Kennedy JN, Wang S et al (2019) Derivation, validation, and potential treatment implications of novel clinical phenotypes for sepsis. JAMA 321(20):2003–2017. https://doi.org/10.1001/jama.2019.5791
Quinten VM, van Meurs M, Olgers TJ, Vonk JM, Ligtenberg JJM, Ter Maaten JC (2018) Repeated vital sign measurements in the emergency department predict patient deterioration within 72 hours: a prospective observational study. Scand J Trauma Resusc Emerg Med 26(1):57. https://doi.org/10.1186/s13049-018-0525-y
Abdullah SMOB, Sørensen RH, Dessau RBC, Sattar SMRU, Wiese L, Nielsen FE (2019) Prognostic accuracy of qSOFA in predicting 28-day mortality among infected patients in an emergency department: a prospective validation study. Emerg Med J 36(12):722–728. https://doi.org/10.1136/emermed-2019-208456
Kilinc Toker A, Kose S, Turken M (2021) Comparison of SOFA Score, SIRS, qSOFA, and qSOFA + L criteria in the diagnosis and prognosis of sepsis. Eur J Med 53(1):40–47. https://doi.org/10.5152/eurasianjmed.2021.20081
Dykes LA, Heintz SJ, Heintz BH, Livorsi DJ, Egge JA, Lund BC (2019) Contrasting qSOFA and SIRS criteria for early sepsis identification in a veteran population. Fed Pract 36(2):S21–S24
Gando S, Shiraishi A, Abe T, Kushimoto S, Mayumi T, Fujishima S, Hagiwara A, Shiino Y, Shiraishi SI, Hifumi T, Otomo Y, Okamoto K, Sasaki J, Takuma K, Yamakawa K, Japanese Association for Acute Medicine (JAAM) Sepsis Prognostication in Intensive Care Unit and Emergency Room (SPICE) (JAAM SPICE) Study Group (2020) The SIRS criteria have better performance for predicting infection than qSOFA scores in the emergency department. Sci Rep 10(1):8095. https://doi.org/10.1038/s41598-020-64314-8
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare that they have no conflict of interest'.
Human and animal rights statement
This study was approved by the institutional IRB.
Informed consent
Informed consent was waived as the study was deemed minimal risk to human subjects.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nguyen, P.H., Fay, K.A., English, J.M. et al. Serial measurements of SIRS and SEP scores to identify unique phenotypes of sepsis. Intern Emerg Med (2024). https://doi.org/10.1007/s11739-023-03512-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11739-023-03512-4