Abstract
Risk factors for COVID-19-related outcomes have been variably reported. We used the standardised LACE index to examine admissions and in-hospital mortality associated with COVID-19. Data were collected in the pre-pandemic period (01-04-2019 to 29-02-2020) from 10,173 patients (47.7% men: mean age ± standard deviation = 68.3 years ± 20.0) and in the pandemic period (01-03-2019 to 31-03-2021) from 12,434 patients. With the latter, 10,982 were without COVID-19 (47.4% men: mean age = 68.3 years ± 19.6) and 1452 with COVID-19 (58.5% men: mean age = 67.0 years ± 18.4). Admissions and mortality were compared between pre-pandemic and pandemic patients, according to LACE index. Admission rates rose disproportionately with higher LACE indices amongst the COVID-19 group. Mortality rates amongst the pre-pandemic, pandemic non-COVID-19 and COVID-19 groups with LACE index scores < 4 were 0.7%, 0.5%, 0%; for scores 4–9 were 5.0%, 3.7%, 8.9%; and for scores ≥ 10 were: 24.2%, 20.4%, 43.4%, respectively. The area under the curve receiver operating characteristic for predicting mortality by LACE index was 76% for COVID-19 and 77% for all non-COVID-19 patients. The risk of age and sex-adjusted mortality did not differ from the pre-pandemic group for COVID-19 patients with LACE index scores < 4. However, risk increased drastically for scores from 4 to 9: odds ratio = 3.74 (95% confidence interval = 2.63–5.32), and for scores ≥ 10: odds ratio = 4.02 (95% confidence interval = 3.38–4.77). In conclusion, patients with LACE index scores ≥ 4 have disproportionally greater risk of COVID-19 hospital admissions and deaths, in support of previous studies in patients without COVID-19. However, of importance, our data also emphasise their increased risk in patients with COVID-19. Because the LACE index has a good predictive power of mortality, it should be considered for routine use to identify high-risk COVID-19 patients.
Similar content being viewed by others
Introduction
Coronavirus disease (COVID-19) has contributed to a high proportion of deaths in adults world-wide from the beginning of the pandemic in 2019 [1]. Since then, complications of COVID-19, including symptom severity, intensive care admission and mortality, have been associated with a wide range of risk factors. These include: male gender [2,3,4], obesity [4, 5], underlying chronic health conditions [3,4,5], learning difficulties [6], and older age [3, 4, 6, 7]. Also, included are deprivation [2, 4], unmarried status, as an immigrant from a low or middle-income country [2], people living in multi-occupancy dwellings [6] and ethnic minority groups [6, 8]. However, these individual risk factors have been variably reported between studies, so that currently there exists no consensus for the use of any standardised health index to predict the risk of complications and outcomes from COVID-19. Consequently, it is difficult, or impossible, to utilise existing data to compare clinical performances between studies.
The LACE index (Length of stay; Acuity of admission; Charlson co-morbidity index; Emergency department visits) scoring tool has been developed and validated to predict health outcomes, such as short-term mortality, readmission after a hospital discharge [9] and in-hospital mortality [10, 11]. This standardised index has been used widely in research and clinical practice for a number of years in different populations and conditions [10,11,12,13,14,15]. In this study, we hypothesised that patients with high LACE index scores might be at increased risk of death from COVID-19 infection. We have thus used the LACE index to examine in-hospital mortality during the COVID-19 pandemic, in both patients admitted with COVID-19 and those admitted with general medical conditions (non-COVID-19), and in comparison to a reference group, namely patients admitted with general medical conditions during the immediately preceding year.
Materials and methods
Study design, participants and setting
We analysed prospectively collected data of 22,644 consecutive unplanned admissions to a single NHS hospital (Ashford and St Peter’s NHS Foundation Trust, Surrey, UK). There were 37 cases (0.16%) for whom LACE index scores could not be calculated. This left 22,607 patients for analysis, comprising a group of 10,173 patients admitted before the COVID-19 pandemic (1 April 2019 to 29 February 2020), and 12,434 patients admitted during the pandemic (1 March 2020 to 31 March 2021). The pandemic group itself comprised 10,982 with general medical conditions (without COVID-19) and 1,452 with COVID-19 [16].
Measurements
Clinical data were recorded including age, sex and comorbidities (coded according to the international classification of diseases, ICD-11) [17] for calculation of the Charlson co-morbidity index [18]. The LACE index was calculated from Length of stay (score range 0–7), Acuity of admission (score range 0 or 3), Charlson co-morbidity index (score range 0–5), Emergency department visits (score range 0 or 4). The LACE index scale therefore ranges from 0 to 19 [19].
Categorisation of variables
The LACE index was categorised into two-point intervals, except for the lowest category (range 0–3) and highest category (range 14–19), for the initial exploration of the relationship between the LACE index and the distributions of admissions and mortality. This was followed by the creation of three LACE index categories based on the previous levels: scores < 4, 4–9, and ≥ 10 [10,11,12].
Statistical analysis
Chi-square tests were used to examine differences between categorical variables including rates of admission and in-hospital mortality. Analysis of variance (ANOVA) was used to assess differences between continuous variables, including age, amongst patients admitted before and during the pandemic. Receiver operating characteristic (ROC) curves were constructed to determine the area under the curve (AUC) for the LACE index, as a predictor of in-hospital mortality. Logistic regression was used to assess the risk of in-hospital mortality (dependent variables) in patients admitted during the COVID-19 pandemic compared to those admitted before the pandemic (reference group), according to different LACE index categories. Odds ratios (OR) and 95% confidence intervals (CI) are presented as two models; model 1: unadjusted, and model 2: adjusted for age and sex. Analyses were performed using IBM SPSS Statistics, v25.0 (IBM Corp., Armonk, NY).
Results
General description
Data were analysed from a total of 22,607 patients (48.3% men) admitted either before the COVID-19 pandemic (1 April 2019 to 29 February 2020), or during the pandemic (1 March 2020 to 31 March 2021). There were 10,173 patients admitted in the pre-pandemic period with a mean (SD) age of 68.3 years (20.0), 10,982 non-COVID-19 patients in the pandemic period with a mean age of 68.3 years (19.6), and 1452 with COVID-19, with a mean age of 67.0 years (18.4). There were 13.4, 46.5, and 39.9% of patients within the LACE index categories of < 4, 4–9 and ≥ 10 respectively. Overall, the proportion of deaths in hospital was 7.9% (Supplementary Table 1). In addition, there were no age differences between groups of patients admitted before the pandemic and those admitted during the pandemic without COVID-19 (P = 0.868). However, patients admitted with COVID-19 were younger than both the pre-pandemic (P = 0.014) and pandemic non-COVID-19 (P = 0.017) groups. Compared with patients admitted before the pandemic, patients with COVID-19 had a similar age in the lowest LACE index category, but were younger amongst the higher categories (Fig. 1),
Based on the LACE index categories at two-point intervals (but including the two extreme categories of 0–3 and ≥ 14), men and women had similar admission rates between the pre-pandemic and pandemic non-COVID-19 patients for any given LACE index score (Fig. 2A, B). By contrast, in both sexes, there were relatively smaller proportions of patients admitted with COVID-19 who had lower range of LACE index score (< 8). However, COVID-19 admissions began to exceed those of non-COVID-19 patients for those who had a LACE index score ≥ 8. An exception was for the highest category (LACE index score ≥ 14) where the rates of admission for COVID-19 were similar to those of the non-COVID-19 groups. Overall, the patterns of admissions for each of the three study groups within each LACE index category were almost identical for men and women (Fig. 2A, B). Based on the three LACE index categories (scores < 4, 4–9 and ≥ 10), compared to the pre-pandemic reference group, the pandemic non-COVID-19 group had similar distributions of gender and LACE index categories, and lower in-hospital mortality rates (7.6 versus 6.0%) (Table 1). The proportion of male admissions was significantly (χ2 = 65.8, P < 0.001) higher amongst those with COVID-19 (58.5% men), compared both to those admitted without COVID-19 during the pandemic (47.4% men), and those during the pre-pandemic period (47.7% men). Amongst patients admitted with COVID-19, there was a higher proportion with a LACE index ≥ 10 (53.0 versus 38.8%), and in-hospital deaths (24.5 versus 7.6%) in comparison to the pre-pandemic and non-COVID-19 pandemic groups (Table 1).
LACE index and mortality
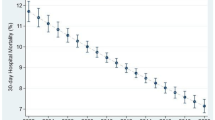
Based on the two-point intervals of the LACE index scores, there were similarities for in-hospital mortality between groups, rising progressively with increasing LACE index scores. Mortality rates were also similar amongst patients admitted before and during the pandemic without COVID-19 for any given LACE index score. By contrast, mortality rates for COVID-19 patients with low LACE index score (< 8) were slightly higher than those in non-COVID patients, but amongst those with LACE index scores ≥ 8, the mortality rates rose to a much greater extent, peaking at over 50% amongst those with LACE index scores of ≥ 14 in both sexes. The patterns of mortality for each study group within each LACE index category were similar for men and women (Fig. 2C, D). In-hospital mortality rates were similarly low for pre-pandemic, pandemic non-COVID-19 and COVID-19 groups: 0.7 vs 0.5 vs 0% amongst lowest (< 4) LACE index scores. However, these rose disproportionately amongst COVID-19 patients: 5.0 vs 3.7 vs 8.9% amongst intermediate (4–9) LACE index scores; and 24.2 vs 20.4 vs 43.4% amongst LACE index scores ≥ 10 (Fig. 3).
After adjustment for age and sex, compared to the pre-pandemic (reference) period, in-hospital mortality did not differ for those admitted during the pandemic without COVID-19 for those with a LACE index score < 10. However, mortality was significantly lower for those with a score ≥ 10: adjusted OR = 0.76 (95% CI 0.67–0.86). The risk of in-hospital mortality also did not differ from the reference group for patients with COVID-19 who had a LACE index score < 4. However, in-hospital death in patients admitted with COVID-19 was significantly greater amongst those with a LACE index score between 4 and 9: adjusted OR = 3.74 (95% CI 2.63–5.32) and rose further amongst those with a LACE index score ≥ 10: adjusted OR = 4.02 (95%CI 3.38–4.77) (Table 2).
Ability of the LACE index to predict mortality
ROC analysis showed comparable performance of LACE index scores in the prediction of in-hospital mortality amongst all three study groups. The AUC was 77.3% (95% CI 75.9–78.7%, P < 0.001) for the pre-pandemic group (Fig. 4A); 77.2% (95% CI 75.7–78.8%, P < 0.001) for the pandemic non-COVID-19 group (Fig. 4B) and 76.4% (95% CI 73.9–79.0%, P < 0.001) for the COVID-19 group (Fig. 4C).
Discussion
Key findings
The LACE index has become a universally accepted index for predicting early readmissions and mortality in patients without COVID-19, for which the majority of findings were published before the pandemic. As far as we are aware, however, this is the first large study to use the LACE index in the study of admission and mortality rates for patients with COVID-19. A number of important findings emerged from this study: (i) a high LACE index score is a risk factor for increased hospital admissions with or without COVID-19, (ii) amongst patients with high LACE index scores, COVID-19 is associated with disproportionately higher rates of in-hospital mortality, and (iii) the LACE index has a similar predictive power of in-hospital mortality in patients admitted with COVID-19 to patients admitted with a general medical condition (non-COVID-19). The standardised LACE index scoring tool, routinely used in clinical settings, should therefore be considered for future routine use to identify high-risk patients with COVID-19 and enable inter-study comparison of clinical research and practice.
Admission rates according to LACE index scores
The present study extended to COVID-19, showed evidence for a relationship between the LACE index and health outcomes. The observation that over half (53%) of patients admitted with COVID-19 had a LACE index score ≥ 10 suggest most of this group of patients had underlying poor health, although they were significantly younger than non-COVID patients. The rates of admission did not increase in the highest LACE index category (score ≥ 14) and suggest a survival bias, i.e. a proportion of those with poorest health or oldest age may have died before being admitted to hospital.
The LACE index has been shown extensively to relate to a number of outcomes including frequent early readmissions, and mortality whether in-hospital or after a discharge from hospital, in different study populations and admitted with a variety of non-COVID-19 medical conditions [10,11,12,13,14,15]. Unlike existing binary variables used to relate COVID-19 outcomes with variables, such as gender, ethnicity, obesity and learning difficulties, the LACE index has a wide range of scale (0–19 points). This allows more detailed analyses including the use of ROC curves to assess the power of prediction, and multiple thresholds to be examined in relation to COVID-19 outcomes. For example, the higher proportion of men admitted in the COVID-19 group is consistent with previous reports [2,3,4].
Mortality according to LACE index scores
The proportionately excessive risk of death from COVID-19 amongst patients with high LACE index scores has not been reported in the existing literature. Furthermore, there was a stepwise increment in the risk of death with increasing LACE index scores. Remarkably, there were no deaths amongst the 79 patients admitted with COVID-19 and who had a low LACE index score of < 4. However, compared to patients without COVID-19, the risk of death from COVID-19 rose disproportionately with increasing LACE index scores. This emphasises that the excess mortality associated with COVID-19 is accentuated by underlying poor health.
In addition, we have also shown a lower risk of mortality amongst non-COVID-19 patients admitted during the pandemic compared to those admitted before the pandemic, particularly if in the highest LACE index category. These findings are in consistent with our previous report [20] and suggest that the standard of care-quality of patients admitted with general medical conditions continued to be maintained, or even increased, during the pandemic.
Ability of the LACE index to predict mortality
The use of ROC curve analysis showed that the LACE index had a predictive power of in-hospital mortality amongst patients admitted with COVID-19 (AUC = 76%) similar to that amongst patients admitted with a general medical condition (AUC = 77%). These figures are also comparable to those reported previously (AUC = 66–83%) [10, 21,22,23]. This observation therefore supports the use of the LACE index scoring tool to identify high-risk patients admitted to hospital with COVID-19.
Strengths and limitations
The strengths of this study lie in the large number of patients with very few missing cases, and the use of a reference group admitted immediately prior to the pandemic, and in the same centre, for comparison. Thus, the methods of data collection were consistent, including construction of LACE index scores. Thus, analyses could be conducted more readily with robust statistical techniques including ROC curves and logistic regression, with appropriate adjustments. This study focussed on the COVID-19 pandemic wave 1 and wave 2, which included the delta and alpha variants. The recent omicron variant may pose a different outcome. Similarly, caution should be taken with other variants in other parts of the world.
In conclusion, we have demonstrated that patients with high LACE index scores have disproportionally greater risk of COVID-19 admissions to hospital and related deaths. This index should therefore be considered for routine use in the identification of high-risk patients with COVID-19.
Abbreviations
- ANOVA:
-
Analysis of variance
- AUC:
-
Area under the curve
- CI:
-
Confidence interval
- COVID-19:
-
Coronavirus disease
- ICD:
-
International classification of diseases
- OR:
-
Odds ratio
- LACE:
-
Length of stay; Acuity of admission; Charlson co-morbidity index; Emergency department visits
- ROC:
-
Receiver operating characteristic
References
World Health Organization. Coronavirus disease (COVID-19) pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed 04 Mar 2022
Drefahl S, Wallace M, Mussino E, Aradhya S, Kolk M, Brandén M (2020) A population-based cohort study of socio-demographic risk factors for COVID-19 deaths in Sweden. Nat Commun 11(1):1–7
Lippi G, Mattiuzzi C, Sanchis-Gomar F, Henry BM (2020) Clinical and demographic characteristics of patients dying from COVID-19 in Italy vs China. J Med Virol 92:1759–1760
Bhaskaran K, Bacon S, Evans SJ, Bates CJ, Rentsch CT, MacKenna B, Tomlinson L, Walker AJ, Schultze A, Morton CE, Grint D (2021) Factors associated with deaths due to COVID-19 versus other causes: population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform. Lancet Reg Health Eur 6:100109
Docherty AB, Harrison EM, Green CA, Hardwick HE, Pius R, Norman L, Holden KA, Read JM, Dondelinger F, Carson G, Merson L (2020) Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO clinical characterization protocol: prospective observational cohort study. BMJ 369:m1985
Joy M, Hobbs FR, Bernal JL, Sherlock J, Amirthalingam G, McGagh D, Akinyemi O, Byford R, Dabrera G, Dorward J, Ellis J (2020) Excess mortality in the first COVID pandemic peak: cross-sectional analyses of the impact of age, sex, ethnicity, household size, and long-term conditions in people of known SARS-CoV-2 status in England. Br J Gen Pract 70(701):e890–e898
Onder G, Rezza G, Brusaferro S (2020) Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA 323(18):1775–1776
Mathur R, Rentsch CT, Morton CE, Hulme WJ, Schultze A, MacKenna B, Eggo RM, Bhaskaran K, Wong AY, Williamson EJ, Forbes H (2021) Ethnic differences in SARS-CoV-2 infection and COVID-19-related hospitalisation, intensive care unit admission, and death in 17 million adults in England: an observational cohort study using the OpenSAFELY platform. Lancet 397(10286):1711–1724
Van Walraven C, Dhalla IA, Bell C, Etchells E, Stiell IG, Zarnke K, Austin PC, Forster AJ (2010) Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. CMAJ 182(6):551–557
Fry CH, Heppleston E, Fluck D, Han TS (2020) Derivation of age-adjusted LACE index thresholds in the prediction of mortality and frequent hospital readmissions in adults. Intern Emerg Med 15(7):1319–1325
Heppleston E, Fry CH, Kelly K, Shepherd B, Wright R, Jones G, Robin J, Murray P, Fluck D, Han TS (2021) LACE index predicts age-specific unplanned readmissions and mortality after hospital discharge. Aging Clin Exp Res 33(4):1041–1048
Linzey JR, Nadel JL, Wilkinson DA, Rajajee V, Daou BJ, Pandey AS (2020) Validation of the LACE index (Length of stay, Acuity of admission, Comorbidities, Emergency department use) in the adult neurosurgical patient population. Neurosurgery 86(1):E33–E37
Wang H, Robinson RD, Johnson C, Zenarosa NR, Jayswal RD (2014) Using the LACE index to predict hospital readmissions in congestive heart failure patients. BMC Cardiovasc Disord 14(1):1–8
Labrosciano C, Tavella R, Air T, Zeitz CJ, Worthley M, Beltrame JF (2021) The LACE index: a predictor of mortality and readmission in patients with acute myocardial infarction. J Healthc Qual 43(5):292–303
Cho E, Lee S, Bae WK, Lee JR, Lee H (2022) Prediction value of the LACE index to identify older adults at high risk for all-cause mortality in South Korea: a nationwide population-based study. BMC Geriatr 22(1):1–9
Fluck D, Rankin S, Lewis A, Robin J, Rees J, Finch J, Jones Y, Jones G, Kelly K, Murray P, Wood M, Fry CH, Han TS (2022) Comparison of characteristics and outcomes of patients admitted to hospital with COVID-19 during wave 1 and wave 2 of the current pandemic. Intern Emerg Med 17:675–684
World Health Organization. www.who.int/standards/classifications/classification-of-diseases/emergency-use-icd-codes-for-covid-19-disease-outbreak. Accessed 04 Mar 2022
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
MDCalc. https://www.mdcalc.com/lace-index-readmission. Accessed 04 Mar 2022
Fluck D, Fry CH, Rankin S, Lewis A, Robin J, Rees J, Finch J, Jones Y, Jones G, Tudose J, Taylor L, Han TS (2022) Does the length of stay in hospital affect healthcare outcomes of patients without COVID-19 who were admitted during the pandemic? A retrospective monocentric study. Intern Emerg Med 24:1–9. https://doi.org/10.1007/s11739-022-02945-7
Cotter PE, Bhalla VK, Wallis SJ, Biram RW (2012) Predicting readmissions: poor performance of the LACE index in an older UK population. Age Ageing 41(6):784–789
Fonseca J, Costa F, Mateus J, Ferreira D, Clemente H, Veríssimo M, Caravalho A (2017) Identification of high-risk patients for early death or unplanned readmission using the LACE index in an older Portuguese population. F1000Research 6(1798):1798
Shaffer BK, Cui Y, Wanderer JP (2019) Validation of the LACE readmission and mortality prediction model in a large surgical cohort: comparison of performance at preoperative assessment and discharge time points. J Clin Anesth 58:22–26
Author information
Authors and Affiliations
Contributions
TSH reviewed the topic-related literature and performed the study concept and analysis design. DF and JR performed the study coordination and management of patients. TSH wrote the first draft, analysed, interpreted the data and revised the manuscript. CHF and DF edited the manuscript. All authors checked, interpreted results and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This study does not require NHS Research Ethics Committee approval since it involves secondary analysis of anonymised data. This study was conducted in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Statement of human and animal rights: This article does not contain any studies with animals performed by any of the authors.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fluck, D., Fry, C.H., Robin, J. et al. High LACE index scores are associated with disproportionate excess deaths in hospital amongst patients with COVID-19. Intern Emerg Med 17, 1891–1897 (2022). https://doi.org/10.1007/s11739-022-03015-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-022-03015-8