Abstract
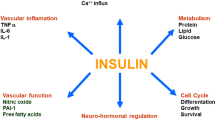
Experimental and clinical studies aimed at investigating the mechanism(s) underlying vascular complications of diabetes indicate that a great number of molecules are involved in the pathogenesis of these complications. Most of these molecules are inflammatory mediators or markers generated by immune or adipose tissue. Some of them, i.e. resistin and sortilin, have been shown to be involved in the cross talk between adipocytes and inflammatory cells. This interaction is an attractive area of research, particularly in type 2 diabetes and obesity. Other proteins, such as adiponectin and visfatin, appear to be more promising as possible vascular markers. In addition, some molecules involved in calcium/phosphorus metabolism, such as klotho and FGF23, have an involvement in the pathogenesis of diabetic vasculopathy, which appears to be dependent on the degree of vascular impairment. Inflammatory markers are a promising tool for treatment decisions while measuring plasma levels of adipokines, sortilin, Klotho and FGF23 in adequately sized longitudinal studies is expected to allow a more precise characterization of diabetic vascular disease and the optimal use of personalized treatment strategies.

Similar content being viewed by others
References
Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, Di Angelantonio E, Ingelsson E, Lawlor DA, Selvin E, Stampfer M, Stehouwer CD, Lewington S, Pennells L, Thompson A, Sattar N, White IR, Ray KK, Danesh J, Collaboration ERF (2010) Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 375(9733):2215–2222. https://doi.org/10.1016/S0140-6736(10)60484-9
Sasso FC, Chiodini P, Carbonara O, De Nicola L, Conte G, Salvatore T, Nasti R, Marfella R, Gallo C, Signoriello S, Torella R, Minutolo R, Group NITDS (2012) High cardiovascular risk in patients with Type 2 diabetic nephropathy: the predictive role of albuminuria and glomerular filtration rate. The NID-2 Prospective Cohort Study. Nephrol Dial Transplant 27(6):2269–2274. https://doi.org/10.1093/ndt/gfr644
Minutolo R, Sasso FC, Chiodini P, Cianciaruso B, Carbonara O, Zamboli P, Tirino G, Pota A, Torella R, Conte G, De Nicola L (2006) Management of cardiovascular risk factors in advanced type 2 diabetic nephropathy: a comparative analysis in nephrology, diabetology and primary care settings. J Hypertens 24(8):1655–1661. https://doi.org/10.1097/01.hjh.0000239303.93872.31
Norris KC, Smoyer KE, Rolland C, Van der Vaart J, Grubb EB (2018) Albuminuria, serum creatinine, and estimated glomerular filtration rate as predictors of cardio-renal outcomes in patients with type 2 diabetes mellitus and kidney disease: a systematic literature review. BMC Nephrol 19(1):36. https://doi.org/10.1186/s12882-018-0821-9
Selvin E, Erlinger TP (2004) Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999–2000. Circulation 110(6):738–743. https://doi.org/10.1161/01.CIR.0000137913.26087.F0
Selvin E, Marinopoulos S, Berkenblit G, Rami T, Brancati FL, Powe NR, Golden SH (2004) Meta-analysis: glycosylated hemoglobin and cardiovascular disease in diabetes mellitus. Ann Intern Med 141(6):421–431. https://doi.org/10.7326/0003-4819-141-6-200409210-00007
Hirsch IB (2015) Glycemic variability and diabetes complications: does it matter? Of course it does! Diabetes Care 38(8):1610–1614. https://doi.org/10.2337/dc14-2898
Lontchi-Yimagou E, Sobngwi E, Matsha TE, Kengne AP (2013) Diabetes mellitus and inflammation. Curr Diab Rep 13(3):435–444. https://doi.org/10.1007/s11892-013-0375-y
Lu J, Marnell LL, Marjon KD, Mold C, Du Clos TW, Sun PD (2008) Structural recognition and functional activation of FcgammaR by innate pentraxins. Nature 456(7224):989–992. https://doi.org/10.1038/nature07468
Biscetti F, Ferraro PM, Hiatt WR, Angelini F, Nardella E, Cecchini AL, Santoliquido A, Pitocco D, Landolfi R, Flex A (2019) Inflammatory cytokines associated with failure of lower extremity endovascular revascularization (LER): A Prospective Study of a Population with diabetes. Diabetes Care. https://doi.org/10.2337/dc19-0408
Libby P (2017) Interleukin-1 beta as a target for atherosclerosis therapy: biological basis of CANTOS and beyond. J Am Coll Cardiol 70(18):2278–2289. https://doi.org/10.1016/j.jacc.2017.09.028
Chen CH, Jiang T, Yang JH, Jiang W, Lu J, Marathe GK, Pownall HJ, Ballantyne CM, McIntyre TM, Henry PD, Yang CY (2003) Low-density lipoprotein in hypercholesterolemic human plasma induces vascular endothelial cell apoptosis by inhibiting fibroblast growth factor 2 transcription. Circulation 107(16):2102–2108. https://doi.org/10.1161/01.CIR.0000065220.70220.F7
Stancel N, Chen CC, Ke LY, Chu CS, Lu J, Sawamura T, Chen CH (2016) Interplay between CRP, atherogenic LDL, and LOX-1 and Its potential role in the pathogenesis of atherosclerosis. Clin Chem 62(2):320–327. https://doi.org/10.1373/clinchem.2015.243923
Balamir I, Ates I, Topcuoglu C, Turhan T (2018) Association of endocan, ischemia-modified albumin, and hscrp levels with endothelial dysfunction in type 2 diabetes mellitus. Angiology 69(7):609–616. https://doi.org/10.1177/0003319717740781
Soeki T, Sata M (2016) Inflammatory biomarkers and atherosclerosis. Int Heart J 57(2):134–139. https://doi.org/10.1536/ihj.15-346
Xu B, Yang CZ, Wu SB, Zhang D, Wang LN, Xiao L, Chen Y, Wang CR, Tong A, Zhou XF, Li XH, Guan XH (2017) Risk factors for lower extremity amputation in patients with diabetic foot. Zhonghua Nei Ke Za Zhi 56(1):24–28. https://doi.org/10.3760/cma.j.issn.0578-1426.2017.01.007
Inoue K, Sugiyama A, Reid PC, Ito Y, Miyauchi K, Mukai S, Sagara M, Miyamoto K, Satoh H, Kohno I, Kurata T, Ota H, Mantovani A, Hamakubo T, Daida H, Kodama T (2007) Establishment of a high sensitivity plasma assay for human pentraxin3 as a marker for unstable angina pectoris. Arterioscler Thromb Vasc Biol 27(1):161–167. https://doi.org/10.1161/01.ATV.0000252126.48375.d5
Mutlu M, Yuksel N, Takmaz T, Dincel AS, Bilgihan A, Altınkaynak H (2017) Aqueous humor pentraxin-3 levels in patients with diabetes mellitus. Eye (Lond) 31(10):1463–1467. https://doi.org/10.1038/eye.2017.87
Ahmad J, Zubair M, Malik A, Siddiqui MA, Wangnoo SK (2012) Cathepsin-D, adiponectin, TNF-α, IL-6 and hsCRP plasma levels in subjects with diabetic foot and possible correlation with clinical variables: a multicentric study. Foot (Edinb) 22(3):194–199. https://doi.org/10.1016/j.foot.2012.03.015
Silva LC, Ortigosa LC, Benard G (2010) Anti-TNF-α agents in the treatment of immune-mediated inflammatory diseases: mechanisms of action and pitfalls. Immunotherapy 2(6):817–833. https://doi.org/10.2217/imt.10.67
Nidorf SM, Eikelboom JW, Budgeon CA, Thompson PL (2013) Low-dose colchicine for secondary prevention of cardiovascular disease. J Am Coll Cardiol 61(4):404–410. https://doi.org/10.1016/j.jacc.2012.10.027
Banerjee M, Saxena M (2012) Interleukin-1 (IL-1) family of cytokines: role in type 2 diabetes. Clin Chim Acta 413(15–16):1163–1170. https://doi.org/10.1016/j.cca.2012.03.021
Herder C, Dalmas E, Böni-Schnetzler M, Donath MY (2015) The IL-1 pathway in type 2 diabetes and cardiovascular complications. Trends Endocrinol Metab 26(10):551–563. https://doi.org/10.1016/j.tem.2015.08.001
Dinarello CA, Ikejima T, Warner SJ, Orencole SF, Lonnemann G, Cannon JG, Libby P (1987) Interleukin 1 induces interleukin 1. I. Induction of circulating interleukin 1 in rabbits in vivo and in human mononuclear cells in vitro. J Immunol 139(6):1902–1910
Suzuki K, Murtuza B, Smolenski RT, Sammut IA, Suzuki N, Kaneda Y, Yacoub MH (2001) Overexpression of interleukin-1 receptor antagonist provides cardioprotection against ischemia-reperfusion injury associated with reduction in apoptosis. Circulation 104(12 Suppl 1):I303–I308. https://doi.org/10.1161/hc37t1.094871
Libby P, Warner SJ, Friedman GB (1988) Interleukin 1: a mitogen for human vascular smooth muscle cells that induces the release of growth-inhibitory prostanoids. J Clin Invest 81(2):487–498. https://doi.org/10.1172/JCI113346
Schlesinger N, Alten RE, Bardin T, Schumacher HR, Bloch M, Gimona A, Krammer G, Murphy V, Richard D, So AK (2012) Canakinumab for acute gouty arthritis in patients with limited treatment options: results from two randomised, multicentre, active-controlled, double-blind trials and their initial extensions. Ann Rheum Dis 71(11):1839–1848. https://doi.org/10.1136/annrheumdis-2011-200908
Zheng ZH, Zeng X, Nie XY, Cheng YJ, Liu J, Lin XX, Yao H, Ji CC, Chen XM, Jun F, Wu SH (2019) Interleukin-1 blockade treatment decreasing cardiovascular risk. Clin Cardiol. https://doi.org/10.1002/clc.23246
Gosling J, Slaymaker S, Gu L, Tseng S, Zlot CH, Young SG, Rollins BJ, Charo IF (1999) MCP-1 deficiency reduces susceptibility to atherosclerosis in mice that overexpress human apolipoprotein B. J Clin Invest 103(6):773–778. https://doi.org/10.1172/JCI5624
Panee J (2012) Monocyte chemoattractant protein 1 (MCP-1) in obesity and diabetes. Cytokine 60(1):1–12. https://doi.org/10.1016/j.cyto.2012.06.018
Arakelyan A, Petrkova J, Hermanova Z, Boyajyan A, Lukl J, Petrek M (2005) Serum levels of the MCP-1 chemokine in patients with ischemic stroke and myocardial infarction. Mediat Inflamm 3:175–179. https://doi.org/10.1155/MI.2005.175
Czemplik M, Kulma A, Wang YF, Szopa J (2017) Therapeutic strategies of plant-derived compounds for diabetes via regulation of monocyte chemoattractant protein-1. Curr Med Chem 24(14):1453–1468. https://doi.org/10.2174/0929867324666170303162935
Ismail NA, Abd El Baky AN, Ragab S, Hamed M, Hashish MA, Shehata A (2016) Monocyte chemoattractant protein 1 and macrophage migration inhibitory factor in children with type 1 diabetes. J Pediatr Endocrinol Metab 29(6):641–645. https://doi.org/10.1515/jpem-2015-0340
Hartman J, Frishman WH (2014) Inflammation and atherosclerosis: a review of the role of interleukin-6 in the development of atherosclerosis and the potential for targeted drug therapy. Cardiol Rev 22(3):147–151. https://doi.org/10.1097/CRD.0000000000000021
Mai J, Virtue A, Shen J, Wang H, Yang XF (2013) An evolving new paradigm: endothelial cells—conditional innate immune cells. J Hematol Oncol 6:61. https://doi.org/10.1186/1756-8722-6-61
Erlandsson Harris H, Andersson U (2004) Mini-review: the nuclear protein HMGB1 as a proinflammatory mediator. Eur J Immunol 34(6):1503–1512. https://doi.org/10.1002/eji.200424916
Kalinina N, Agrotis A, Antropova Y, DiVitto G, Kanellakis P, Kostolias G, Ilyinskaya O, Tararak E, Bobik A (2004) Increased expression of the DNA-binding cytokine HMGB1 in human atherosclerotic lesions: role of activated macrophages and cytokines. Arterioscler Thromb Vasc Biol 24(12):2320–2325. https://doi.org/10.1161/01.ATV.0000145573.36113.8a
Biscetti F, Straface G, De Cristofaro R, Lancellotti S, Rizzo P, Arena V, Stigliano E, Pecorini G, Egashira K, De Angelis G, Ghirlanda G, Flex A (2010) High-mobility group box-1 protein promotes angiogenesis after peripheral ischemia in diabetic mice through a VEGF-dependent mechanism. Diabetes 59(6):1496–1505. https://doi.org/10.2337/db09-1507
Oozawa S, Sano S, Nishibori M (2014) Usefulness of high mobility group box 1 protein as a plasma biomarker in patient with peripheral artery disease. Acta Med Okayama 68(3):157–162. https://doi.org/10.18926/AMO/52656
Biscetti F, Flex A, Alivernini S, Tolusso B, Gremese E, Ferraccioli G (2017) The role of high-mobility group box-1 and its crosstalk with microbiome in rheumatoid arthritis. Mediat Inflamm 2017:5230374. https://doi.org/10.1155/2017/5230374
Yang J, Shah R, Robling AG, Templeton E, Yang H, Tracey KJ, Bidwell JP (2008) HMGB1 is a bone-active cytokine. J Cell Physiol 214(3):730–739. https://doi.org/10.1002/jcp.21268
Hajer GR, van Haeften TW, Visseren FL (2008) Adipose tissue dysfunction in obesity, diabetes, and vascular diseases. Eur Heart J 29(24):2959–2971. https://doi.org/10.1093/eurheartj/ehn387
Vionnet N, Hani EH, Dupont S, Gallina S, Francke S, Dotte S, De Matos F, Durand E, Leprêtre F, Lecoeur C, Gallina P, Zekiri L, Dina C, Froguel P (2000) Genomewide search for type 2 diabetes-susceptibility genes in French whites: evidence for a novel susceptibility locus for early-onset diabetes on chromosome 3q27-qter and independent replication of a type 2-diabetes locus on chromosome 1q21-q24. Am J Hum Genet 67(6):1470–1480. https://doi.org/10.1086/316887
Pilz S, Horejsi R, Möller R, Almer G, Scharnagl H, Stojakovic T, Dimitrova R, Weihrauch G, Borkenstein M, Maerz W, Schauenstein K, Mangge H (2005) Early atherosclerosis in obese juveniles is associated with low serum levels of adiponectin. J Clin Endocrinol Metab 90(8):4792–4796. https://doi.org/10.1210/jc.2005-0167
Sasso FC, Pafundi PC, Marfella R, Calabrò P, Piscione F, Furbatto F, Esposito G, Galiero R, Gragnano F, Rinaldi L, Salvatore T, D'Amico M, Adinolfi LE, Sardu C (2019) Adiponectin and insulin resistance are related to restenosis and overall new PCI in subjects with normal glucose tolerance: the prospective AIRE Study. Cardiovasc Diabetol 18(1):24. https://doi.org/10.1186/s12933-019-0826-0
Ezenwaka CE, Kalloo R (2005) Caribbean female patients with type 2 diabetes mellitus have lower serum levels of adiponectin than nondiabetic subjects. Neth J Med 63(2):64–69
Al-Daghri NM, Al-Attas OS, Alokail MS, Alkharfy KM, Hussain T (2011) Adiponectin gene variants and the risk of coronary artery disease in patients with type 2 diabetes. Mol Biol Rep 38(6):3703–3708. https://doi.org/10.1007/s11033-010-0484-5
Hung WC, Wang CP, Lu LF, Yu TH, Chiu CA, Chung FM, Chen HJ, Houng JY, Shin SJ, Lee YJ (2010) Circulating adiponectin level is associated with major adverse cardiovascular events in type 2 diabetic patients with coronary artery disease. Endocr J 57(9):793–802
Xiang K, Wang Y, Zheng T, Jia W, Li J, Chen L, Shen K, Wu S, Lin X, Zhang G, Wang C, Wang S, Lu H, Fang Q, Shi Y, Zhang R, Xu J, Weng Q (2004) Genome-wide search for type 2 diabetes/impaired glucose homeostasis susceptibility genes in the Chinese: significant linkage to chromosome 6q21-q23 and chromosome 1q21-q24. Diabetes 53(1):228–234
Watanabe K, Watanabe R, Konii H, Shirai R, Sato K, Matsuyama TA, Ishibashi-Ueda H, Koba S, Kobayashi Y, Hirano T, Watanabe T (2016) Counteractive effects of omentin-1 against atherogenesis. Cardiovasc Res 110(1):118–128. https://doi.org/10.1093/cvr/cvw016
Yamawaki H (2011) Vascular effects of novel adipocytokines: focus on vascular contractility and inflammatory responses. Biol Pharm Bull 34(3):307–310
Biscetti F, Nardella E, Bonadia N, Angelini F, Pitocco D, Santoliquido A, Filipponi M, Landolfi R, Flex A (2019) Association between plasma omentin-1 levels in type 2 diabetic patients and peripheral artery disease. Cardiovasc Diabetol 18(1):74. https://doi.org/10.1186/s12933-019-0880-7
Menzel J, di Giuseppe R, Biemann R, Wittenbecher C, Aleksandrova K, Pischon T, Fritsche A, Schulze MB, Boeing H, Isermann B, Weikert C (2016) Omentin-1 and risk of myocardial infarction and stroke: Results from the EPIC-Potsdam cohort study. Atherosclerosis 251:415–421. https://doi.org/10.1016/j.atherosclerosis.2016.06.003
Verma S, Li SH, Wang CH, Fedak PW, Li RK, Weisel RD, Mickle DA (2003) Resistin promotes endothelial cell activation: further evidence of adipokine-endothelial interaction. Circulation 108(6):736–740. https://doi.org/10.1161/01.CIR.0000084503.91330.49
Degawa-Yamauchi M, Bovenkerk JE, Juliar BE, Watson W, Kerr K, Jones R, Zhu Q, Considine RV (2003) Serum resistin (FIZZ3) protein is increased in obese humans. J Clin Endocrinol Metab 88(11):5452–5455. https://doi.org/10.1210/jc.2002-021808
On YK, Park HK, Hyon MS, Jeon ES (2007) Serum resistin as a biological marker for coronary artery disease and restenosis in type 2 diabetic patients. Circ J 71(6):868–873. https://doi.org/10.1253/circj.71.868
Calabro P, Samudio I, Willerson JT, Yeh ET (2004) Resistin promotes smooth muscle cell proliferation through activation of extracellular signal-regulated kinase 1/2 and phosphatidylinositol 3-kinase pathways. Circulation 110(21):3335–3340. https://doi.org/10.1161/01.CIR.0000147825.97879.E7
Chen MP, Chung FM, Chang DM, Tsai JC, Huang HF, Shin SJ, Lee YJ (2006) Elevated plasma level of visfatin/pre-B cell colony-enhancing factor in patients with type 2 diabetes mellitus. J Clin Endocrinol Metab 91(1):295–299. https://doi.org/10.1210/jc.2005-1475
Adya R, Tan BK, Chen J, Randeva HS (2008) Nuclear factor-kappaB induction by visfatin in human vascular endothelial cells: its role in MMP-2/9 production and activation. Diabetes Care 31(4):758–760. https://doi.org/10.2337/dc07-1544
Mazaherioun M, Hosseinzadeh-Attar MJ, Janani L, Vasheghani Farahani A, Rezvan N, Karbaschian Z, Hossein-Nezhad A (2012) Elevated serum visfatin levels in patients with acute myocardial infarction. Arch Iran Med 15(11):688–692
Patel KM, Strong A, Tohyama J, Jin X, Morales CR, Billheimer J, Millar J, Kruth H, Rader DJ (2015) Macrophage sortilin promotes LDL uptake, foam cell formation, and atherosclerosis. Circ Res 116(5):789–796. https://doi.org/10.1161/CIRCRESAHA.116.305811
Ogawa K, Ueno T, Iwasaki T, Kujiraoka T, Ishihara M, Kunimoto S, Takayama T, Kanai T, Hirayama A, Hattori H (2016) Soluble sortilin is released by activated platelets and its circulating levels are associated with cardiovascular risk factors. Atherosclerosis 249:110–115. https://doi.org/10.1016/j.atherosclerosis.2016.03.041
Goettsch C, Kjolby M, Aikawa E (2018) Sortilin and its multiple roles in cardiovascular and metabolic diseases. Arterioscler Thromb Vasc Biol 38(1):19–25. https://doi.org/10.1161/ATVBAHA.117.310292
Oh TJ, Ahn CH, Kim BR, Kim KM, Moon JH, Lim S, Park KS, Lim C, Jang H, Choi SH (2017) Circulating sortilin level as a potential biomarker for coronary atherosclerosis and diabetes mellitus. Cardiovasc Diabetol 16(1):92. https://doi.org/10.1186/s12933-017-0568-9
Biscetti F, Bonadia N, Santini F, Angelini F, Nardella E, Pitocco D, Santoliquido A, Filipponi M, Landolfi R, Flex A (2019) Sortilin levels are associated with peripheral arterial disease in type 2 diabetic subjects. Cardiovasc Diabetol 18(1):5. https://doi.org/10.1186/s12933-019-0805-5
Biscetti F, Straface G, Pitocco D, Angelini F, Tinelli G, Landolfi R, Flex A (2016) Fibroblast growth factor 23 serum level in type 2 diabetic Italian subjects with peripheral arterial disease and critical limb ischemia. Eur Rev Med Pharmacol Sci 20(19):4048–4054
Kiechl S, Schett G, Wenning G, Redlich K, Oberhollenzer M, Mayr A, Santer P, Smolen J, Poewe W, Willeit J (2004) Osteoprotegerin is a risk factor for progressive atherosclerosis and cardiovascular disease. Circulation 109(18):2175–2180. https://doi.org/10.1161/01.CIR.0000127957.43874.BB
Fang L, Li X (2016) Level of serum phosphorus and adult type 2 diabetes mellitus. Zhong Nan Da Xue Xue Bao Yi Xue Ban 41(5):502–506. https://doi.org/10.11817/j.issn.1672-7347.2016.05.009
Razzaque MS (2009) The FGF23-Klotho axis: endocrine regulation of phosphate homeostasis. Nat Rev Endocrinol 5(11):611–619. https://doi.org/10.1038/nrendo.2009.196
Rennenberg RJ, Kessels AG, Schurgers LJ, van Engelshoven JM, de Leeuw PW, Kroon AA (2009) Vascular calcifications as a marker of increased cardiovascular risk: a meta-analysis. Vasc Health Risk Manag 5(1):185–197. https://doi.org/10.2147/vhrm.s4822
Starup-Linde J, Vestergaard P (2016) Biochemical bone turnover markers in diabetes mellitus—a systematic review. Bone 82:69–78. https://doi.org/10.1016/j.bone.2015.02.019
Mary A, Hartemann A, Brazier M, Aubert CE, Kemel S, Salem JE, Cluzel P, Liabeuf S, Massy Z, Mentaverri R, Bourron O, Kamel S (2018) Higher parathyroid hormone levels are associated with increased below-the-knee arterial calcification in type 2 diabetes. Diabetes Metab 44(3):305–308. https://doi.org/10.1016/j.diabet.2017.04.008
Freedman BI, Divers J, Russell GB, Palmer ND, Bowden DW, Carr JJ, Wagenknecht LE, Hightower RC, Xu J, Smith SC, Langefeld CD, Hruska KA, Register TC (2015) Plasma FGF23 and calcified atherosclerotic plaque in African Americans with type 2 diabetes mellitus. Am J Nephrol 42(6):391–401. https://doi.org/10.1159/000443241
Berezin AE, Berezin AA (2019) Impaired function of fibroblast growth factor 23/Klotho protein axis in prediabetes and diabetes mellitus: promising predictor of cardiovascular risk. Diabetes Metab Syndr 13(4):2549–2556. https://doi.org/10.1016/j.dsx.2019.07.018
Flotyńska J, Uruska A, Araszkiewicz A, Zozulińska-Ziółkiewicz D (2018) Klotho protein function among patients with type 1 diabetes. Endokrynol Pol 69(6):696–704. https://doi.org/10.5603/EP.a2018.0070
Pan HC, Chou KM, Lee CC, Yang NI, Sun CY (2018) Circulating Klotho levels can predict long-term macrovascular outcomes in type 2 diabetic patients. Atherosclerosis 276:83–90. https://doi.org/10.1016/j.atherosclerosis.2018.07.006
Martín-Núñez E, Donate-Correa J, López-Castillo Á, Delgado-Molinos A, Ferri C, Rodríguez-Ramos S, Cerro P, Pérez-Delgado N, Castro V, Hernández-Carballo C, Mora-Fernández C, Navarro-González JF (2017) Soluble levels and endogenous vascular gene expression of. Clin Sci (Lond) 131(21):2601–2609. https://doi.org/10.1042/CS20171242
Six I, Okazaki H, Gross P, Cagnard J, Boudot C, Maizel J, Drueke TB, Massy ZA (2014) Direct, acute effects of Klotho and FGF23 on vascular smooth muscle and endothelium. PLoS ONE 9(4):e93423. https://doi.org/10.1371/journal.pone.0093423
Olejnik A, Franczak A, Krzywonos-Zawadzka A, Kałużna-Oleksy M, Bil-Lula I (2018) The biological role of klotho protein in the development of cardiovascular diseases. Biomed Res Int 2018:5171945. https://doi.org/10.1155/2018/5171945
Semba RD, Cappola AR, Sun K, Bandinelli S, Dalal M, Crasto C, Guralnik JM, Ferrucci L (2011) Plasma klotho and cardiovascular disease in adults. J Am Geriatr Soc 59(9):1596–1601. https://doi.org/10.1111/j.1532-5415.2011.03558.x
Loyer X, Zlatanova I, Devue C, Yin M, Howangyin KY, Klaihmon P, Guerin CL, Kheloufi M, Vilar J, Zannis K, Fleischmann BK, Hwang DW, Park J, Lee H, Menasché P, Silvestre JS, Boulanger CM (2018) Intra-cardiac release of extracellular vesicles shapes inflammation following myocardial infarction. Circ Res 123(1):100–106. https://doi.org/10.1161/CIRCRESAHA.117.311326
Sluijter JPG, Davidson SM, Boulanger CM, Buzás EI, de Kleijn DPV, Engel FB, Giricz Z, Hausenloy DJ, Kishore R, Lecour S, Leor J, Madonna R, Perrino C, Prunier F, Sahoo S, Schiffelers RM, Schulz R, Van Laake LW, Ytrehus K, Ferdinandy P (2018) Extracellular vesicles in diagnostics and therapy of the ischaemic heart: Position Paper from the Working Group on Cellular Biology of the Heart of the European Society of Cardiology. Cardiovasc Res 114(1):19–34. https://doi.org/10.1093/cvr/cvx211
Boulanger CM, Loyer X, Rautou PE, Amabile N (2017) Extracellular vesicles in coronary artery disease. Nat Rev Cardiol 14(5):259–272. https://doi.org/10.1038/nrcardio.2017.7
Bellin G, Gardin C, Ferroni L, Chachques JC, Rogante M, Mitrečić D, Ferrari R, Zavan B (2019) Exosome in cardiovascular diseases: a complex world full of hope. Cells. https://doi.org/10.3390/cells8020166
Harris TA, Yamakuchi M, Ferlito M, Mendell JT, Lowenstein CJ (2008) MicroRNA-126 regulates endothelial expression of vascular cell adhesion molecule 1. Proc Natl Acad Sci USA 105(5):1516–1521. https://doi.org/10.1073/pnas.0707493105
Soeki T, Yamaguchi K, Niki T, Uematsu E, Bando S, Matsuura T, Ise T, Kusunose K, Hotchi J, Tobiume T, Yagi S, Fukuda D, Taketani Y, Iwase T, Yamada H, Wakatsuki T, Shimabukuro M, Sata M (2015) Plasma microRNA-100 is associated with coronary plaque vulnerability. Circ J 79(2):413–418. https://doi.org/10.1253/circj.CJ-14-0958
Witkowski M, Weithauser A, Tabaraie T, Steffens D, Kränkel N, Stratmann B, Tschoepe D, Landmesser U, Rauch-Kroehnert U (2016) Micro-RNA-126 reduces the blood thrombogenicity in diabetes mellitus via targeting of tissue factor. Arterioscler Thromb Vasc Biol 36(6):1263–1271. https://doi.org/10.1161/ATVBAHA.115.306094
Lalla E, Papapanou PN (2011) Diabetes mellitus and periodontitis: a tale of two common interrelated diseases. Nat Rev Endocrinol 7(12):738–748. https://doi.org/10.1038/nrendo.2011.106
Mascarenhas JV, Albayati MA, Shearman CP, Jude EB (2014) Peripheral arterial disease. Endocrinol Metab Clin North Am 43(1):149–166. https://doi.org/10.1016/j.ecl.2013.09.003
Silvestro A, Scopacasa F, Ruocco A, Oliva G, Schiano V, Zincarelli C, Brevetti G (2003) Inflammatory status and endothelial function in asymptomatic and symptomatic peripheral arterial disease. Vasc Med 8(4):225–232. https://doi.org/10.1191/1358863x03vm503oa
Hirabara SM, Gorjão R, Vinolo MA, Rodrigues AC, Nachbar RT, Curi R (2012) Molecular targets related to inflammation and insulin resistance and potential interventions. J Biomed Biotechnol 2012:379024. https://doi.org/10.1155/2012/379024
Rizza S, Cardellini M, Porzio O, Pecchioli C, Savo A, Cardolini I, Senese N, Lauro D, Sbraccia P, Lauro R, Federici M (2011) Pioglitazone improves endothelial and adipose tissue dysfunction in pre-diabetic CAD subjects. Atherosclerosis 215(1):180–183. https://doi.org/10.1016/j.atherosclerosis.2010.12.021
Dormandy JA, Charbonnel B, Eckland DJ, Erdmann E, Massi-Benedetti M, Moules IK, Skene AM, Tan MH, Lefèbvre PJ, Murray GD, Standl E, Wilcox RG, Wilhelmsen L, Betteridge J, Birkeland K, Golay A, Heine RJ, Korányi L, Laakso M, Mokán M, Norkus A, Pirags V, Podar T, Scheen A, Scherbaum W, Schernthaner G, Schmitz O, Skrha J, Smith U, Taton J, Investigators P (2005) Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet 366(9493):1279–1289. https://doi.org/10.1016/S0140-6736(05)67528-9
Rajamani K, Colman PG, Li LP, Best JD, Voysey M, D'Emden MC, Laakso M, Baker JR, Keech AC, Investigators Fs (2009) Effect of fenofibrate on amputation events in people with type 2 diabetes mellitus (FIELD study): a prespecified analysis of a randomised controlled trial. Lancet 373(9677):1780–1788. https://doi.org/10.1016/S0140-6736(09)60698-X
Bertrand MJ, Tardif JC (2017) Inflammation and beyond: new directions and emerging drugs for treating atherosclerosis. Expert Opin Emerg Drugs 22(1):1–26. https://doi.org/10.1080/14728214.2017.1269743
Bäck M, Hansson GK (2015) Anti-inflammatory therapies for atherosclerosis. Nat Rev Cardiol 12(4):199–211. https://doi.org/10.1038/nrcardio.2015.5
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
The procedures employed to draft this manuscript respect the ethical standards in the Helsinki Declaration of 1975, as revised in 2000, as well as the national law.
Informed consent
For this type of article, formal consent is not required.
Consent for publication
All authors have read the paper and agree that it can be published.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Biscetti, F., Nardella, E., Cecchini, A.L. et al. Biomarkers of vascular disease in diabetes: the adipose-immune system cross talk. Intern Emerg Med 15, 381–393 (2020). https://doi.org/10.1007/s11739-019-02270-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-019-02270-6