Abstract
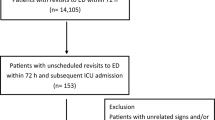
Once diagnostic work-up and first therapy are completed in patients visiting the emergency department (ED), boarding them within the ED until an in-hospital bed became available is a common practice in busy hospitals. Whether this practice may harm the patients remains a debate. We sought to determine whether an ED boarding time longer than 4 h places the patients at increased risk of in-hospital death. This retrospective, propensity score-matched analysis and propensity score-based inverse probability weighting analysis was conducted in an adult ED in a single, academic, 1136-bed hospital in France. All patients hospitalized via the adult ED from January 1, 2013 to March 31, 2018 were included. Hospital mortality (primary outcome) and hospital length of stay (LOS) were assessed in (1) a matched cohort (1:1 matching of ED visits with or without ED boarding time longer than 4 h but similar propensity score to experience an ED boarding time longer than 4 h); and (2) the whole study cohort. Sensitivity analysis to unmeasured confounding and analyses in pre-specified cohorts of patients were conducted. Among 68,632 included ED visits, 17,271 (25.2%) had an ED boarding time longer than 4 h. Conditional logistic regression performed on a 10,581 pair-matched cohort, and generalized estimating equations with adjustment on confounders and stabilized propensity score-based inverse probability weighting applied on the whole cohort showed a significantly increased risk of hospital death in patients experiencing an ED boarding time longer than 4 h: odds ratio (OR) of 1.13 (95% confidence interval [95% CI] 1.05–1.22), P = 0.001; and OR of 1.12 (95% CI 1.03–1.22), P = 0.007, respectively. Sensitivity analyses showed that these findings might be robust to unmeasured confounding. Hospital LOS was significantly longer in patients exposed to ED boarding time longer than 4 h: median difference 2 days (95% CI 1–2) (P < 0.001) in matched analysis and mean difference 1.15 days (95% CI 1.02–1.28) (P < 0.001) in multivariable unmatched analysis. In this single-center propensity score-based cohort analysis, patients experiencing an ED boarding time longer than 4 h before being transferred to an in-patient bed were at increased risk of hospital death.


Similar content being viewed by others
References
Kellermann AL, Martinez R (2011) The ER, 50 years on. N Engl J Med. 364(24):2278–2279
Mason S, Knowles E, Boyle A (2017) Exit block in emergency departments: a rapid evidence review. Emerg Med J. 34(1):46–51
Pines JM, Iyer S, Disbot M et al (2008) The effect of emergency department crowding on patient satisfaction for admitted patients. Acad Emerg Med. 15(9):825–831
McCarthy ML, Ding R, Zeger SL et al (2011) A randomized controlled trial of the effect of service delivery information on patient satisfaction in an emergency department fast track. Acad Emerg Med. 18(7):674–685
Vieth TL, Rhodes KV (2006) The effect of crowding on access and quality in an academic ED. Am J Emerg Med 24(7):787–794
Fee C, Weber EJ, Maak CA, Bacchetti P (2007) Effect of emergency department crowding on time to antibiotics in patients admitted with community-acquired pneumonia. Ann Emerg Med. 50(5):501–509
Pines JM, Localio AR, Hollander JE et al (2007) The impact of emergency department crowding measures on time to antibiotics for patients with community-acquired pneumonia. Ann Emerg Med. 50(5):510–516
Hwang U, Richardson L, Livote E et al (2008) Emergency department crowding and decreased quality of pain care. Acad Emerg Med. 15(12):1258–1265
Richardson D, McMahon KLH (2009) Emergency Department access block occupancy predicts delay to surgery in patients with fractured neck of femur. Emerg Med Aust 21(4):304–308
Gaieski DF, Agarwal AK, Mikkelsen ME et al (2017) The impact of ED crowding on early interventions and mortality in patients with severe sepsis. Am J Emerg Med 35(7):953–960
Bernstein SL, Aronsky D, Duseja R, Society for Academic Emergency Medicine, Emergency Department Crowding Task Force et al (2009) The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med 16(1):1–10
Shen YC, Hsia RY (2011) Association between ambulance diversion and survival among patients with acute myocardial infarction. JAMA 305(23):2440–2447
Sun BC, Hsia RY, Weiss RE et al (2013) Effect of emergency department crowding on outcomes of admitted patients. Ann Emerg Med. 61(6):605–611
Eriksson CO, Stoner RC, Eden KB, Newgard CD, Guise JM (2017) The Association between hospital capacity strain and inpatient outcomes in highly developed countries: a systematic review. J Gen Intern Med. 32(6):686–696
Schiff GD (2011) System dynamics and dysfunctionalities: levers for overcoming emergency department overcrowding. Acad Emerg Med. 18(12):1255–1261
Wiler JL, Welch S, Pines J, Schuur J, Jouriles N, Stone-Griffith S (2015) Emergency department performance measures updates: proceedings of the 2014 emergency department benchmarking alliance consensus summit. Acad Emerg Med 22(5):542–553
Singer AJ, Thode HC Jr, Viccellio P et al (2011) The association between length of emergency department boarding and mortality. Acad Emerg Med. 18(12):1324–1329
Derose SF, Gabayan GZ, Chiu VY et al (2014) Emergency department crowding predicts admission length-of-stay but not mortality in a large health system. Med Care 52(7):602–611
Lord K, Parwani V, Ulrich A et al (2018) Emergency department boarding and adverse hospitalization outcomes among patients admitted to a general medical service. Am J Emerg Med. 36(7):1246–1248
Reznek MA, Upatising B, Kennedy SJ, Durham NT, Forster RM, Michael SS (2018) Mortality associated with emergency department boarding exposure: are there differences between patients admitted to ICU and non-ICU settings? Med Care 56(5):436–440
Afilal M, Yalaoui F, Dugardin F, Amodeo L, Laplanche D, Blua P (2016) Forecasting the Emergency Department patients flow. J Med Syst. 40(7):175
Southern DA, Quan H, Ghali WA (2004) Comparison of the Elixhauser and Charlson/Deyo methods of comorbidity measurement in administrative data. Med Care. 42(4):355–360
Rubin DB (1997) Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 127(8 Pt 2):757–763
Austin PC (2011) Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 10(2):150–161
Austin PC (2009) Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 28(25):3083–3107
Xu S, Ross C, Raebel MA, Shetterly S, Blanchette CD (2010) Use of stabilized inverse propensity scores as weights to directly estimate relative risk and its confidence intervals. Value Health 13(2):273–277
Hanley JA, Negassa A, Edwardes MD, Forrester JE (2003) Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 157(4):364–375
Cole SR, Hernan MA (2008) Constructing inverse probability weights for marginal structural models. Am J Epidemiol. 168(6):6564
Austin PC, Stuart EA (2015) Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 34(28):3661–3679
VanderWeele TJ, Ding P (2017) Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 167(4):268–274
Ye LG, Zhou GJ, He XJ et al (2012) Prolonged length of stay in the emergency department in high-acuity patients at a Chinese tertiary hospital. Emerg Med Aust 24(6):634–640
Powell MP, Yu X, Isehunwa O, Chang CF (2018) National Trends in Hospital Emergency Department Visits among Those with and without multiple chronic conditions, 2007–2012. Hosp Top 96(1):1–8
Chalfin DB, Trzeciak S, Likourezos A et al (2007) Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 35(6):1477–1483
Cardoso LT, Grion CM, Matsuo T et al (2011) Impact of delayed admission to intensive care units on mortality of critically ill patients: a cohort study. Crit Care. 15:R28
Al-Qahtani S, Alsultan A, Haddad S et al (2017) The association of duration of boarding in the emergency room and the outcome of patients admitted to the intensive care unit. BMC Emerg Med. 17(1):34
Richardson DB (2002) The access block effect: relationship between delay to reaching an inpatient bed and inpatient length of stay. Med J Aust. 177(9):492–495
Liew D, Liew D, Kennedy MP (2003) Emergency department length of stay independently predicts excess inpatient length of stay. Med J Aust. 179(10):524–526
Sprivulis PC, Da Silva J-A, Jacobs IG et al (2006) The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust. 184(5):208–212
Källberg AS, Göransson KE, Florin J, Östergren J, Brixey JJ, Ehrenberg A (2015) Contributing factors to errors in Swedish emergency departments. Int Emerg Nurs. 23(2):156–161
Zhou JC, Pan KH, Zhou DY et al (2012) High hospital occupancy is associated with increased risk for patients boarding in the emergency department. Am J Med. 125(4):416.e1–7
Liu SW, Thomas SH, Gordon JA, Hamedani AG, Weissman JS (2009) A pilot study examining undesirable events among emergency department-boarded patients awaiting inpatient beds. Ann Emerg Med. 54(3):381–385
Sun BC, Laurie A, Prewitt L et al (2016) Risk-adjusted variation of Publicly Reported Emergency Department timeliness measures. Ann Emerg Med. 67(4):509–516
Commission Régionale d’Experts Urgences Île de France (2015) Activité des services d’urgence Île de France. Année. https://www.iledefrance.ars.sante.fr/sites/default/files/2017-02/Urgences-CREU-Rapport-IDF-2015.pdf. Accessed 17 July 2019
Welch SJ, Augustine JJ, Dong L, Savitz LA, Snow G, James BC (2012) Volume-related differences in emergency department performance. Jt Comm J Qual Patient Saf. 38(9):395–402
Henderson T, Shepheard J, Sundararajan V (2006) Quality of diagnosis and procedure coding in ICD-10 administrative data. Med Care. 44(11):1011–1019
Funding
This study was funded only by the Centre hospitalier régional d’Orléans. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
TB had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: TB, AM, OM. Acquisition, analysis, or interpretation of data: TB, AM, OM. Drafting of the manuscript: TB. Critical revision of the manuscript for important intellectual content: TB, AM, OM. Statistical analysis: TB. Obtained funding: TB. Administrative, technical, or material support: TB, AM, OM. Supervision: TB.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no financial or non-financial competing interests relative to this submission.
Ethical approval
The Ethical Committee of the French Society of Intensive Care approved the study protocol (#CE SRLF 18-31).
Informed consent
For this retrospective study that complied with French law requirements related to personal data protection, informed consent was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Boulain, T., Malet, A. & Maitre, O. Association between long boarding time in the emergency department and hospital mortality: a single-center propensity score-based analysis. Intern Emerg Med 15, 479–489 (2020). https://doi.org/10.1007/s11739-019-02231-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-019-02231-z