Abstract
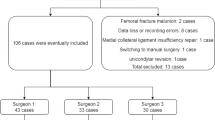
The main purpose of this study was to determine the learning curve of Robotic assisted Total Knee Arthroplasty surgery through assessment of operative time and comparison with that of conventional jig based Total Knee Arthroplasty. The study included our first 75 Robotic assisted Total Knee Arthroplasty and 25 randomly selected conventional jig-based Total knee arthroplasty from June 2017 to December 2017. The 75 cases were divided into 3 groups of 25 consecutive cases. The mean of operative time for each phase and total time was compared between the 3 groups and with the mean of total time for conventional jig based group. In our experience, Robotic assisted Total Knee arthroplasty was associated with a learning curve of approximately 25 cases. The mean for Registration phase of Group A (1st set of 25 cases) was 6.12 min (SD 1.8 min), group B (2nd set of 25 cases) was 4.46 min (SD 0.79 min) and group C (3rd set of 25 cases) was 4.17 min (SD 0.59 min). The mean for Planning phase of group A was 5.08 min (SD 1.01 min), group B was 4.04 min (SD 0.37 min) and group C was 4.01 min (SD 0.35 min). The mean for Cutting Phase of group A was 28.22 min (SD 6.24 min), group B was 22.49 min (SD 0.79 min) and group C was 22.36 min (SD 0.88 min). The mean for total time of group A was 39.42 min (SD 8.02), group B was 31 min (SD 1.22 min), group C was 30.53 min (SD 1.14 min) and conventional group was 30.54 min (SD 1.14 min). On comparing the Registration phase (Group A vs B, p < 0.001; Group B vs C, p 0.14; Group A vs C, p < 0.001), Planning phase (Group A vs B, p < 0.001; Group B vs C, p 0.75; Group A vs C, p < 0.001), Cutting phase (Group A vs B, p < 0.001; Group B vs C, p 0.58; Group A vs C, p < 0.001) and Total time (Group A vs B, p < 0.001; Group B vs C, p 0.74; Group A vs C, p < 0.001; Group A vs Conventional, p < 0.001; Group B vs Conventional, p 0.17, Group C vs Conventional, p 0.99), the results showed that the inflection point for learning curve in our hands was 25 cases. The learning curve and increased operation theatre time are likely to be major barrier in widespread acceptance of robotic technology amongst arthroplasty surgeons. We, in our experience can say that the learning curve was approximately 25 cases. The results of this study will help the arthroplasty surgeons in accepting this technology and achieve better outcomes.












Similar content being viewed by others
Abbreviations
- TKA:
-
Total knee arthroplasty
- RA-TKA:
-
Robotic assisted- total knee arthroplasty
- OR:
-
Operating room
- ROM:
-
Range of movement
- SD:
-
Standard deviation
- HS:
-
Highly significant
- NS:
-
Not significant
References
Baker PN, van der Meulen JH, Lewsey J, Gregg PJ, National Joint Registry for England and Wales (2007) The role of pain and function in determining patient satisfaction after total knee replacement. Data from the National Joint Registry for England and Wales. J Bone Joint Surg Br 89:893–900
Coon TM (2009) Integrating robotic technology into the operating room. Am J Orthop (Belle Mead NJ) 38:7–9
Feng JE, Novikov D, Anoushiravani AA, Schwarzkopf R (2018) Total knee arthroplasty: improving outcomes with a multidisciplinary approach. J Multidiscip Healthc 11:63–73
Gill GS, Joshi AB, Mills DM (1999) Total condylar knee arthroplasty 16- to 21-year results. Clin Orthop Relat Res Oct;(367):210–215
Grau L, Lingamfelter M, Ponzio D, Post Z, Ong A, Le D, Orozco F (2019) Robotic arm assisted total knee arthroplasty workflow optimization, operative times and learning curve. Arthroplast Today 5:465–470
Inacio MCS, Paxton EW, Graves SE, Namba RS, Nemes S (2017) Projected increase in total knee arthroplasty in the United States - an alternative projection model. Osteoarthritis Cartilage 25:1797–1803
Jeffery RS, Morris RW, Denham RA (1991) Coronal alignment after total knee replacement. J Bone Joint Surg Br 73:709–714
Kayani B, Konan S, Huq SS, Tahmassebi J, Haddad FS (2019) Robotic-arm assisted total knee arthroplasty has a learning curve of seven cases for integration into the surgical workflow but no learning curve effect for accuracy of implant positioning. Knee Surg Sports Traumatol Arthrosc 27:1132–1141
Kayani B, Konan S, Pietrzak JRT, Haddad FS (2018) Iatrogenic Bone and soft tissue trauma in robotic-arm assisted total knee arthroplasty compared with conventional jig-based total knee arthroplasty: a prospective cohort study and validation of a new classification system. J Arthroplasty 33:2496–2501
Kayani B, Konan S, Tahmassebi J, Pietrzak JRT, Haddad FS (2018) Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: a prospective cohort study. Bone Joint J 100-B:930–937
Koenig JA, Suero EM, Plaskos C (2012) Surgical accuracy and efficiency of computer-navigated tka with a robotic cutting guide – report on the first 100 cases. Orthopaed Proc British Editorial Soc Bone Joint Surg 94-B:103–103
Maheshwari AV, Blum YC, Shekhar L, Ranawat AS, Ranawat CS (2009) Multimodal pain management after total hip and knee arthroplasty at the Ranawat orthopaedic center. Clin Orthop Relat Res 467:1418–1423
Mannan A, Vun J, Lodge C, Eyre-Brook A, Jones S (2018) Increased precision of coronal plane outcomes in robotic-assisted total knee arthroplasty: A systematic review and meta-analysis. Surgeon 16:237–244
Parratte S, Pagnano MW, Trousdale RT, Berry DJ (2010) Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am 92:2143–2149
Rand JA, Trousdale RT, Ilstrup DM, Harmsen WS (2003) Factors affecting the durability of primary total knee prostheses. J Bone Joint Surg Am 85:259–265
Ritter MA, Faris PM, Keating EM, Meding JB (1994) Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res Feb;(299):153–156
Sodhi N, Khlopas A, Piuzzi NS, Sultan AA, Marchand RC, Malkani AL, Mont MA (2018) The learning curve associated with robotic total knee arthroplasty. J Knee Surg 31:17–21
Song E-K, Seon J-K, Yim J-H, Netravali NA, Bargar WL (2013) Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clin Orthop Relat Res 471:118–126
Vaidya N, Jaysingani TN, Panjwani T, Patil R, Deshpande A, Kesarkar A (2021) Assessment of accuracy of an imageless hand-held robotic-assisted system in component positioning in total knee replacement: a prospective study. J Robot Surg
Varacallo M, Luo TD, Johanson NA (2022) Total Knee Arthroplasty Techniques. StatPearls StatPearls Publishing, Treasure Island (FL)
Von Keudell A, Sodha S, Collins J, Minas T, Fitz W, Gomoll AH (2014) Patient satisfaction after primary total and unicompartmental knee arthroplasty: an age-dependent analysis. Knee 21:180–184
Funding
No external funding was provided for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors namely Dr. Narendra Vaidya, Dr. Anup Gadekar, Dr. Varun O Agrawal and Dr. Tanmay N. Jaysingani declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study including human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Ethical Committee and the Institutional Review Board.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vaidya, N., Gadekar, A., Agrawal, V.O. et al. Learning curve for robotic assisted total knee arthroplasty: our experience with imageless hand-held Navio system. J Robotic Surg 17, 393–403 (2023). https://doi.org/10.1007/s11701-022-01423-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-022-01423-8