Abstract
Purpose
Laparoscopic bariatric surgeries can cause intense postoperative pain. Opioid medication can alleviate the pain but can have harmful side effects especially in patients with obstructive sleep apnea. To promote early recovery, enhanced recovery after surgery guideline advises minimizing opioid use and opting for alternative analgesics. This paper aims to investigate the effect of regional anesthesia techniques through a systematic review and network meta-analysis. Primary outcome is postoperative morphine equivalent consumption at 24 h.
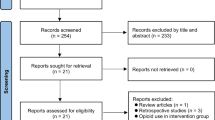
Methods
Search was conducted in the following databases: PubMed, CENTRAL, Scopus, and EMBASE, from the inception until 10 January 2023. The eligibility criteria were determined by PICOS, including postoperative opioid consumption, pain scores, time to ambulate, use of additional analgesics, and adverse events. The quality assessment was performed using the Risk of Bias 2 Tool, and the certainty of evidence was assessed using the GRADE approach. Funnel plots were used to evaluate publication bias.
Results
We included 22 studies in quantitative synthesis. A review of 12 studies found that all techniques had a lower mean consumption of opioids compared to placebo or no intervention, with TAP block having the greatest reduction. The quality of evidence for postoperative pain, PONV, time to deambulate, and use of rescue analgesics, was rated as moderate, with TAP block being the most effective intervention. There was no publication bias in any outcome.
Conclusions
TAP block is superior to other regional anesthesia techniques in reducing opioid consumption, pain, PONV, and use of rescue analgesics in bariatric surgery. However, further research is needed.
Graphical abstract






Similar content being viewed by others
References
Hartwig M, Allvin R, Bäckström R, et al. Factors associated with increased experience of postoperative pain after laparoscopic gastric bypass surgery. Obes Surg. 2017;27:1854–8.
Mason M, Cates CJ, Smith I. Effects of opioid, hypnotic and sedating medications on sleep-disordered breathing in adults with obstructive sleep apnoea. Cochrane Database Syst Rev. 2015;7:CD011090.
Oderda GM, Senagore AJ, Morland K, et al. Opioid-related respiratory and gastrointestinal adverse events in patients with acute postoperative pain: prevalence, predictors, and burden. J Pain Palliat Care Pharmacother. 2019;33:82–97.
Stenberg E, Dos Reis Falcão LF, O’Kane M, et al. Guidelines for perioperative care in bariatric surgery: enhanced recovery after surgery (ERAS) society recommendations: a 2021 update. World J Surg. 2022;46:729–51.
Grape S, Kirkham KR, Albrecht E. The analgesic efficacy of transversus abdominis plane block after bariatric surgery: a systematic review and meta-analysis with trial sequential analysis. Obes Surg. 2020;30:4061–70.
Chaw SH, Lo YL, Goh SL, et al. Transversus abdominis plane block versus intraperitoneal local anesthetics in bariatric surgery: a systematic review and network meta-analysis. Obes Surg. 2021;31:4305–15.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339: b2700.
El-Boghdadly K, Wolmarans M, Stengel AD, et al. Standardizing nomenclature in regional anesthesia: an ASRA-ESRA Delphi consensus study of abdominal wall, paraspinal, and chest wall blocks. Reg Anesth Pain Med. 2021;46:571–80.
Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366: l4898.
Puhan MA, Schünemann HJ, Murad MH, et al. A GRADE working group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ. 2014;349:g5630. Erratum in: BMJ. 2015;350:h3326.
Rücker G, Schwarzer G. Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med Res Methodol. 2015;15:58.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13.
Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Elshazly M, El-Halafawy YM, Mohamed DZ, et al. Feasibility and efficacy of erector spinae plane block versus transversus abdominis plane block in laparoscopic bariatric surgery: a randomized comparative trial. Korean J Anesthesiol. 2022;75:502–9.
Youwakiem PN, Reyad MK, Abo Zeid AEAA, et al. A comparative study between ultrasound guided trans-muscular quadratus lumborum block versus ultrasound guided transversus abdominis plane block as postoperative analgesia in laparoscopic bariatric surgery. QJM. 2021;114(86):hcab086.096.
Symons JL, Kemmeter PR, Davis AT, et al. A double-blinded, prospective randomized controlled trial of intraperitoneal bupivacaine in laparoscopic Roux-en-Y gastric bypass. J Am Coll Surg. 2007;204:392–8.
Alkhamesi NA, Kane JM, Guske PJ, et al. Intraperitoneal aerosolization of bupivacaine is a safe and effective method in controlling postoperative pain in laparoscopic Roux-en-Y gastric bypass. J Pain Res. 2008;1:9–13.
Saber AA, Lee YC, Chandrasekaran A, et al. Efficacy of transversus abdominis plane (TAP) block in pain management after laparoscopic sleeve gastrectomy (LSG): a double-blind randomized controlled trial. Am J Surg. 2019;217:126–32.
Okut G, Turgut E, Kaplan K, et al. Does laparoscopic-guided transversus abdominis plane block have an effect on postoperative pain and recovery after sleeve gastrectomy? Eur Rev Med Pharmacol Sci. 2022;26:5406–12.
Wassef M, Lee DY, Levine JL, et al. Feasibility and analgesic efficacy of the transversus abdominis plane block after single-port laparoscopy in patients having bariatric surgery. J Pain Res. 2013;27(6):837–41.
Ibrahim M, El SH. Efficacy of ultrasound-guided oblique subcostal transversus abdominis plane block after laparoscopic sleeve gastrectomy: a double blind, randomized, placebo controlled study. Egypt J Anaesth. 2014;30:285–92.
Tülübaş EK, Seyit H, Bostancı İ, et al. Laparoscopic transversus abdominal plane block is effective in multimodal analgesia for laparoscopic sleeve gastrectomy. Med J Bakirkoy. 2019;15:198–203.
Sun J, Wang S, Wang J, et al. Effect of intravenous infusion of lidocaine compared with ultrasound-guided transverse abdominal plane block on the quality of postoperative recovery in patients undergoing laparoscopic bariatric surgery. Drug Des Devel Ther. 2022;16:739.
Mittal T, Dey A, Siddhartha R, et al. Efficacy of ultrasound-guided transversus abdominis plane (TAP) block for postoperative analgesia in laparoscopic gastric sleeve resection: a randomized single blinded case control study. Surg Endosc. 2018;32:4985–9.
Sinha A, Jayaraman L, Punhani D. Efficacy of ultrasound-guided transversus abdominis plane block after laparoscopic bariatric surgery: a double blind, randomized, controlled study. Obes Surg. 2013;23:548–53.
Albrecht E, Kirkham KR, Endersby RV, et al. Ultrasound-guided transversus abdominis plane (TAP) block for laparoscopic gastric-bypass surgery: a prospective randomized controlled double-blinded trial. Obes Surg. 2013;23:1309–14.
Emile SH, Abdel-Razik MA, Elbahrawy K, et al. Impact of ultrasound-guided transversus abdominis plane block on postoperative pain and early outcome after laparoscopic bariatric surgery: a randomized double-blinded controlled trial. Obes Surg. 2019;29:1534–41.
Kaur R, Seal A, Lemech I, et al. Intraperitoneal instillation of local anesthetic (IPILA) in bariatric surgery and the effect on post-operative pain scores: a randomized control trial. Obes Surg. 2022;32:2349–56.
Koptan H, Soliman S, Sherif A. Feasibility and perioperative pain-relieving efficacy of ultrasound-guided transversus abdominis plane block in morbidly obese patients undergoing laparoscopic bariatric surgery. Res Opin Anesth Intensive Care. 2015;1:50.
Ruiz-Tovar J, Muñoz JL, Gonzalez J, et al. Postoperative pain after laparoscopic sleeve gastrectomy: comparison of three analgesic schemes (isolated intravenous analgesia, epidural analgesia associated with intravenous analgesia and port-sites infiltration with bupivacaine associated with intravenous analgesia). Surg Endosc. 2017;31:231–6.
Wong KA, Cabrera AG, Argiroff AL, et al. Transversus abdominis plane block with liposomal bupivacaine and its effect on opiate use after weight loss surgery: a randomized controlled trial. Surg Obes Relat Dis. 2020;16:886–93.
Arı DE, Ar AY, Karip CS, et al. Ultrasound-guided subcostal-posterior transversus abdominis plane block for pain control following laparoscopic sleeve gastrectomy. Saudi Med J. 2017;38:1224–9.
de Oliveira GS Jr. Transversus abdominis plane infiltration for laparoscopic gastric banding: a pilot study World. J Gastrointest Surg. 2014;6:27.
Alamdari NM, Bakhtiyari M, Gholizadeh B, et al. Analgesic effect of intraperitoneal bupivacaine hydrochloride after laparoscopic sleeve gastrectomy: a randomized clinical trial. J Gastrointest Surg. 2018;22:396–401.
Omar I, Abualsel A. Efficacy of intraperitoneal instillation of bupivacaine after bariatric surgery: randomized controlled trial. Obes Surg. 2019;29:1735–41.
Safari S, Rokhtabnak F, Djalali Motlagh S, et al. Effect of intraperitoneal bupivacaine on postoperative pain in laparoscopic bariatric surgeries. Surg Obes Relat Dis. 2020;16:299–305.
Schipper IE, Schouten M, Yalcin T, et al. The use of intraperitoneal bupivacaine in laparoscopic roux-en-y gastric bypass: a double-blind, randomized controlled trial. Obes Surg. 2019;29:3118–24.
Ruiz-Tovar J, Gonzalez J, Garcia A, et al. Intraperitoneal ropivacaine irrigation in patients undergoing bariatric surgery: a prospective randomized clinical trial. Obes Surg. 2016;26:2616–21.
Hegazy MA, Hamed H, Salim MS, et al. Effect of different concentrations of intraperitoneal bupivacaine on postoperative outcome in morbidly obese patients undergoing laparoscopic bariatric surgery. Int J Anesth Clin Med. 2020;8:68–73.
Sherif AA, Koptan HM, Soliman SM. Feasibility and perioperative pain-relieving efficacy of ultrasound-guided transversus abdominis plane block in morbidly obese patients undergoing laparoscopic bariatric surgery. Res Opin Anesth Intensive Care. 2015;2:50–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Informed consent does not apply.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
• Laparoscopic bariatric surgeries are considered minimally invasive; however, they could be associated with intense postoperative pain.
• Several regional anesthesia techniques have been proposed to reduce opioid consumption in laparoscopic bariatric surgeries.
• All regional anesthesia techniques were effective in reducing pain in patients undergoing laparoscopic bariatric surgeries.
• TAP block was the most effective technique in reducing opioid consumption, postoperative pain at 6 and 12 h, time to ambulate, and use of additional analgesics.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
De Cassai, A., Paganini, G., Pettenuzzo, T. et al. Single-Shot Regional Anesthesia for Bariatric Surgery: a Systematic Review and Network Meta-Analysis. OBES SURG 33, 2687–2694 (2023). https://doi.org/10.1007/s11695-023-06737-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-06737-6