Abstract
Background
This meta-analysis was performed to investigate how cardiac structures and functions change in the very early stage after bariatric surgery.
Materials and Methods
We thoroughly searched the PubMed, Embase, Cochrane Library, and Web of Science databases for articles including patients who underwent bariatric surgery and examined the changes of their cardiac indices. Results were pooled by using Review Manager 5.1 and Stata 12.0. Weighted mean differences (WMDs) with 95% confidence intervals (CIs) were obtained. The I-squared (I2) test was used to determine the heterogeneity between studies. To identify publication bias, funnel plots and Egger’s test were utilized. The leave-one-out method was used to conduct sensitivity analysis.
Results
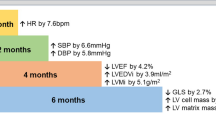
In this meta-analysis, 24 research including 942 patients were considered. According to our findings, most cardiac indices changed 3–6 months following bariatric surgery. An improvement in cardiac geometry was reflected by a reduction in left ventricular mass (LVM) (WMD = − 22.06, 95% CI = (− 27.97, − 16.16)). The left ventricular diastolic function improved, as reflected by the decrease in the E/e’ ratio (WMD = − 0.90, 95% CI = (− 1.83, − 0.16)). Left ventricular ejection fraction (LVEF) did not show an obvious change (WMD = 0.94, 95% CI = (− 0.19, 2.07)), while a more sensitive indicator of left ventricular systolic function, left ventricular longitudinal strain (LV LS), increased (WMD = − 2.43, 95% CI = (− 3.96, − 0.89)).
Conclusion
This meta-analysis includes the newest and most comprehensive cardiac indices to prove that cardiac structures and functions are improved early after bariatric surgery, which has not been reported by any other studies.
Graphical Abstract







Similar content being viewed by others
References
Zeng Q, Li N, Pan X-F, et al. Clinical management and treatment of obesity in China. Lancet Diabetes Endocrinol. 2021;9(6):393–405.
Powell-Wiley TM, Poirier P, Burke LE, et al. Obesity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2021;143(21):e984–1010.
Iwamoto SJ, Abushamat LA, Zaman A, et al. Obesity management in cardiometabolic disease: state of the art. Curr Atheroscler Rep. 2021;23(10):59.
Fisher DP, Johnson E, Haneuse S, et al. Association between bariatric surgery and macrovascular disease outcomes in patients with type 2 diabetes and severe obesity. JAMA. 2018;320(15):1570–82.
Aminian A, Zajichek A, Arterburn DE, et al. Association of metabolic surgery with major adverse cardiovascular outcomes in patients with type 2 diabetes and obesity. JAMA. 2019;322(13):1271–82.
Potter E, Marwick TH. Assessment of left ventricular function by echocardiography: the case for routinely adding global longitudinal strain to ejection fraction. JACC Cardiovasc Imaging. 2018;11(2 Pt 1):260–74.
Turkbey EB, McClelland RL, Kronmal RA, et al. The impact of obesity on the left ventricle. JACC: Cardiovasc Imaging. 2010;3(3):266–74.
Ng ACT, Prevedello F, Dolci G, et al. Impact of diabetes and increasing body mass index category on left ventricular systolic and diastolic function. J Am Soc Echocardiogr. 2018;31(8):916–25.
Holland DJ, Marwick TH, Haluska BA, Leano R, Hordern MD, Hare JL, et al. Subclinical LV dysfunction and 10-year outcomes in type 2 diabetes mellitus. Heart. 2015;101(13):1061–6.
Sterne JA, Hernan MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
Kanoupakis E, Michaloudis D, Fraidakis O, Parthenakis F, Vardas P, Melissas J. Left ventricular function and cardiopulmonary performance following surgical treatment of morbid obesity. Obes Surg. 2001;11(5):552–8.
Cunha Lde C, da Cunha CL, de Souza AM, et al. Evolutive echocardiographic study of the structural and functional heart alterations in obese individuals after bariatric surgery. Arquivos Brasileiros de Cardiologia. 2006;87(5):615–22.
Leichman JG, Aguilar D, King TM, et al. Improvements in systemic metabolism, anthropometrics, and left ventricular geometry 3 months after bariatric surgery. Surg Obes Relat Dis. 2006;2(6):592–9.
Jhaveri RR, Pond KK, Hauser TH, et al. Cardiac remodeling after substantial weight loss: a prospective cardiac magnetic resonance study after bariatric surgery. Surg Obes Relat Dis. 2009;5(6):648–52.
Hsuan C-F, Huang C-K, Lin J-W, et al. The effect of surgical weight reduction on left ventricular structure and function in severe obesity. Obesity. 2010;18(6):1193.
Gaborit B, Jacquier A, Kober F, et al. Effects of bariatric surgery on cardiac ectopic fat lesser decrease in epicardial fat compared to visceral fat loss and no change in myocardial triglyceride content. J Am Coll Cardiol. 2012;60(15):1381–9.
Kokkinos A, Alexiadou K, Liaskos C, et al. Improvement in cardiovascular indices after Roux-en-Y gastric bypass or sleeve gastrectomy for morbid obesity. Obes Surg. 2013;23(1):31–8.
Martin J, Bergeron S, Pibarot P, et al. Impact of bariatric surgery on N-terminal fragment of the prohormone brain natriuretic peptide and left ventricular diastolic function. Can J Cardiol. 2013;29(8):969–75.
Iancu ME, Copaescu C, Serban M, et al. Favorable changes in arterial elasticity, left ventricular mass, and diastolic function after significant weight loss following laparoscopic sleeve gastrectomy in obese individuals. Obes Surg. 2014;24(3):370.
Kaier TE, Morgan D, Grapsa J, et al. Ventricular remodelling post-bariatric surgery: is the type of surgery relevant? A prospective study with 3D speckle tracking. Eur Heart J Cardiovasc Imaging. 2014;15(11):1256–62.
Oz TK, Dayi SU, Seyit H, et al. The effects of weight loss after sleeve gastrectomy on left ventricular systolic function in men versus women. J Clin Ultrasound. 2016;44(8):499.
Tuluce K, Kara C, Tuluce SY, et al. Early reverse cardiac remodeling effect of laparoscopic sleeve gastrectomy. Obes Surg. 2017;27(2):364–75.
Kurnicka K, Domienik-Karlowicz J, Lichodziejewska B, et al. Improvement of left ventricular diastolic function and left heart morphology in young women with morbid obesity six months after bariatric surgery. Cardiol J. 2018;25(1):105.
Mikhalkova D, Holman SR, Jiang H, et al. Bariatric surgery–induced cardiac and lipidomic changes in obesity-related heart failure with preserved ejection fraction. Obesity. 2018;26(2):284–90.
Mostfa SA. Impact of obesity and surgical weight reduction on cardiac remodeling. Indian Heart J. 2018;70:S224–8.
Inci S, Gül M, Alsancak Y, et al. Short- and mid-term effects of sleeve gastrectomy on left ventricular functions with two-dimensional speckle tracking echocardiography in obese patients. Echocardiography. 2019;36:2019–25.
Simsek MA, Cabbar AT, Ozveren O, et al. Short-term effects of sleeve gastrectomy on weight loss and diastolic function in obese patients. Turk Kardiyoloji Dernegi arsivi : Turk Kardiyoloji Derneginin yayin organidir. 2019;47(3):167.
Ammar W, Basset HA, Al Faramawy A, et al. Bariatric surgery and cardiovascular outcome. Egyptian Heart J. 2020;72(1):67.
de Witte D, Wijngaarden LH, van Houten VAA, et al. Improvement of cardiac function after Roux-en-Y Gastric bypass in morbidly obese patients without cardiac history measured by cardiac MRI. Obes Surg. 2020;30(7):2481.
Kaya BC, Elkan H. Impact of weight loss with laparoscopic sleeve gastrectomy on left ventricular diastolic function: a prospective study. Obes Surg. 2020;30(9):3280–6.
Santos ECL, del Castillo JM, Parente GBO, et al. Changes in left ventricular mechanics after sleeve gastrectomy. Obes Surg. 2020;30(2):580–6.
Piche M-E, Clavel M-A, Auclair A, et al. Early benefits of bariatric surgery on subclinical cardiac function: contribution of visceral fat mobilization. Metabolism Clinical and Experimenta. 2021;119:154773.
Alqunai MS, Assakran BS, Widyan AM, Suresh A, Alharbi AA, Almosallam OI, et al. Effect of bariatric surgery on cardiac function in obese patients: an echocardiographic assessment. Saudi Med J. 2022;43(6):587–91.
Castagneto-Gissey L, Angelini G, Mingrone G, et al. The early reduction of left ventricular mass after sleeve gastrectomy depends on the fall of branched-chain amino acid circulating levels. EBioMedicine. 2022;76:103864.
Russo C, Jin Z, Homma S, et al. Effect of obesity and overweight on left ventricular diastolic function: a community-based study in an elderly cohort. J Am Coll Cardiol. 2011;57(12):1368–74.
Russo C, Jin Z, Homma S, et al. Effect of diabetes and hypertension on left ventricular diastolic function in a high-risk population without evidence of heart disease. Eur J Heart Fail. 2010;12(5):454–61.
Halliday BP, Senior R, Pennell DJ. Assessing left ventricular systolic function: from ejection fraction to strain analysis. Eur Heart J. 2021;42(7):789–97.
Lin CH, Kurup S, Herrero P, et al. Myocardial oxygen consumption change predicts left ventricular relaxation improvement in obese humans after weight loss. Obesity (Silver Spring). 2011;19(9):1804–12.
Kindel TL, Foster T, Goldspink P, et al. Early weight loss independent effects of sleeve gastrectomy on diet-induced cardiac dysfunction in obese. Wistar Rats Obes Surg. 2017;27(9):2370–7.
Mehmood K, Moin A, Hussain T, et al. Can manipulation of gut microbiota really be transformed into an intervention strategy for cardiovascular disease management? Folia Microbiol (Praha). 2021;66(6):897–916.
Ashrafian H, Li JV, Spagou K, et al. Bariatric surgery modulates circulating and cardiac metabolites. J Proteome Res. 2014;13(2):570–80.
Gutierrez-Repiso C, Moreno-Indias I, Tinahones FJ. Shifts in gut microbiota and their metabolites induced by bariatric surgery Impact of factors shaping gut microbiota on bariatric surgery outcomes. Rev Endocr Metab Disord. 2021;22(4):1137–56.
Hutch CR, Sandoval D. The role of GLP-1 in the metabolic success of bariatric surgery. Endocrinology. 2017;158(12):4139–51.
Hindso M, Svane MS, Hedback N, et al. The role of GLP-1 in postprandial glucose metabolism after bariatric surgery: a narrative review of human GLP-1 receptor antagonist studies. Surg Obes Relat Dis. 2021;17(7):1383–91.
Margulies KB, Anstrom KJ, Hernandez AF, et al. GLP-1 agonist therapy for advanced heart failure with reduced ejection fraction: design and rationale for the functional impact of GLP-1 for heart failure treatment study. Circ Heart Fail. 2014;7(4):673–9.
Funding
This work was supported by the National Natural Science Foundation of China [81820108007, 81800745].
Author information
Authors and Affiliations
Contributions
Conceptualization: S.H.. Methodology: S.H., Y.L., and J.Z.. Software: S.H.. Validation: S.H., Y.L., J.Z., and Z.Z.. Formal analysis: S.H.. Investigation: S.H.. Resources: S.H. and Y.L. Data curation: S.H.. Writing—original draft preparation: S.H.. Writing—review and editing: C.Z. Visualization: S.H.. Supervision: J.Z. and Z.Z.. Project administration: J.Z. and Z.Z.. Funding acquisition: Z.Z. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Informed consent does not apply.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
1. This is the first meta-analysis specifically focusing on the change in cardiac function and structure early (within 6 months) after bariatric surgery and including the most comprehensive cardiac indices.
2. We validated that cardiac structures and functions have improved early after bariatric surgery.
3. We found that LV LS, a new cardiac index using ultrasound speckle tracking technology, can detect subtle changes in cardiac systolic function before LVEF change, and after bariatric surgery, the LV LS improved.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, S., Lan, Y., Zhang, C. et al. The Early Effects of Bariatric Surgery on Cardiac Structure and Function: a Systematic Review and Meta-Analysis. OBES SURG 33, 453–468 (2023). https://doi.org/10.1007/s11695-022-06366-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06366-5