Abstract
Introduction
The impact of laparoscopic sleeve gastrectomy (LSG) on gastroesophageal reflux disease (GERD) has not been widely quantified, and the data in the literature remain controversial.
Materials and Methods
Candidates for LSG underwent barium swallow, esophageal manometry, ambulatory 24-h esophageal pH monitoring (APM), and gastric emptying scintigraphy before and after surgery (1 and 18 months). Symptoms were evaluated using a gastroesophageal reflux disease questionnaire (GERDq). Esophagogastroduodenoscopy was performed preoperatively in all patients and at 18 months postoperatively in patients who had suffered from preoperative esophagitis.
Results
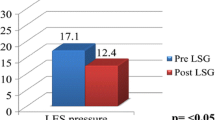
Fifty-two patients were included in the study (64.4% women and 34.6% men) with a median age of 46 years (25–63 years) and BMI of 45.0 ± 5.6 kg/m2. The follow-up rates at 1 and 18 months were 82.7% and 80.8%. At 18 months, the percentage of weight loss (%TWL) was 33.6 ± 10.4% and the percentage of excess BMI loss (%EBMIL) was 77.6 ± 25%. Postoperatively, a significant increase in accelerated gastric emptying and impaired esophageal body motility occurred at 1 and 18 months. A significant worsening of all the values obtained at both 1 and 18 months postoperatively becomes evident when comparing the results of the APM. After surgery, 76.4% of patients had developed “de novo” GERD at 1 month and 41% at 18 months. No improvement was found in patients with symptomatic GERD.
Conclusion
Based on the results of this study, LSG led to a considerable rate of postoperative “de novo” GERD. In addition, no improvement was found in patients with symptomatic GERD.
Graphical Abstract



Similar content being viewed by others
References
Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122(3):248–56. https://doi.org/10.1016/j.amjmed.2008.09.041.
Diamantis T, Apostolou KG, Alexandrou A, et al. Review of long-term weight loss results after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2014;10(1):177–83. https://doi.org/10.1016/j.soard.2013.11.007.
Pallati PK, Shaligram A, Shostrom VK, et al. Improvement in gastroesophageal reflux disease symptoms after various bariatric procedures: review of the Bariatric Outcomes Longitudinal Database. Surg Obes Relat Dis. 2014;10(3):502–7. https://doi.org/10.1016/j.soard.2013.07.018.
Dupree CE, Blair K, Steele SR, et al. Laparoscopic sleeve gastrectomy in patients with preexisting gastroesophageal reflux disease: a national analysis. JAMA Surg. 2014;149(4):328–34. https://doi.org/10.1001/jamasurg.2013.4323.
Oor JE, Roks DJ, Ünlü Ç, et al. Laparoscopic sleeve gastrectomy and gastroesophageal reflux disease: a systematic review and meta-analysis. Am J Surg. 2016;211(1):250–67. https://doi.org/10.1016/j.amjsurg.2015.05.031.
Lazoura O, Zacharoulis D, Triantafyllidis G, et al. Symptoms of gastroesophageal reflux following laparoscopic sleeve gastrectomy are related to the final shape of the sleeve as depicted by radiology. Obes Surg. 2011;21(3):295–9. https://doi.org/10.1007/s11695-010-0339-0.
Laffin M, Chau J, Gill RS, et al. Sleeve gastrectomy and gastroesophageal reflux disease. J Obes. 2013;2013: 741097. https://doi.org/10.1155/2013/741097.
Del Genio G, Tolone S, Limongelli P, et al. Sleeve gastrectomy and development of “de novo” gastroesophageal reflux. Obes Surg. 2014;24(1):71–7. https://doi.org/10.1007/s11695-013-1046-4.
Gorodner V, Buxhoeveden R, Clemente G, et al. Does laparoscopic sleeve gastrectomy have any influence on gastroesophageal reflux disease? Preliminary results. Surg Endosc. 2015;29(7):1760–8. https://doi.org/10.1007/s00464-014-3902-2.
Chiu S, Birch DW, Shi X, et al. Effect of sleeve gastrectomy on gastroesophageal reflux disease: a systematic review. Surg Obes Relat Dis. 2011;7(4):510–5. https://doi.org/10.1016/j.soard.2010.09.011.
Yehoshua RT, Eidelman LA, Stein M, et al. Laparoscopic sleeve gastrectomy—volume and pressure assessment. Obes Surg. 2008;18(9):1083–8. https://doi.org/10.1007/s11695-008-9576-x.
Braghetto I, Davanzo C, Korn O, et al. Scintigraphic evaluation of gastric emptying in obese patients submitted to sleeve gastrectomy compared to normal subjects. Obes Surg. 2009;19(11):1515–21. https://doi.org/10.1007/s11695-009-9954-z.
Gastrointestinal surgery for severe obesity. National Institutes of Health consensus development conference statement. Am J Clin Nutr. 1992;55(2 Suppl):615S-619S. https://doi.org/10.1093/ajcn/55.2.615s.
Jones R, Junghard O, Dent J, et al. Development of the GERDq, a tool for the diagnosis and management of gastro-oesophageal reflux disease in primary care. Aliment Pharmacol Ther. 2009;30(10):1030–8. https://doi.org/10.1111/j.1365-2036.2009.04142.x.
Hungin APS, Molloy-Bland M, Scarpignato C. Revisiting Montreal: new insights into symptoms and their causes, and implications for the future of GERD. Am J Gastroenterol. 2019;114(3):414–21. https://doi.org/10.1038/s41395-018-0287-1.
Gyawali CP, Kahrilas PJ, Savarino E, et al. Modern diagnosis of GERD: the Lyon Consensus. Gut. 2018;67(7):1351–62. https://doi.org/10.1136/gutjnl-2017-314722.
Schmulson MJ, Drossman DA. What is new in Rome IV. J Neurogastroenterol Motil. 2017;23(2):151–63. https://doi.org/10.5056/jnm16214.
Lundell LR, Dent J, Bennett JR, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999;45(2):172–80. https://doi.org/10.1136/gut.45.2.172.
Jonasson C, Wernersson B, Hoff DA, et al. Validation of the GERDq questionnaire for the diagnosis of gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2013;37(5):564–72. https://doi.org/10.1111/apt.12204.
Ruiz de León San Juan A, Ciriza de los Ríos C, Pérez de la Serna Bueno J, et al. Practical aspects of high resolution esophageal manometry. Rev Esp Enferm Dig. 2017;109(2):91–105. https://doi.org/10.17235/reed.2016.4441/2016.
Grupo español de motilidad digestiva. Asociación Española de Neurogastroenterología y motilidad. En: Manual Técnicas (antiguo tratado). [Internet]. Available form: https://asenem.org/index.php/recursos-bibliograficos/manual-tecnicas. [cited 2021 June 29].
Grifo I, Bruna M, Puche J, et al. Gastrectomia vertical: importancia del volumen gástrico resecado. BMI-J. 2017;7(1):1304–8.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13. https://doi.org/10.1097/01.sla.0000133083.54934.ae.
Brethauer SA, Kim J, el Chaar M, et al. ASMBS Clinical Issues Committee. Standardized outcomes reporting in metabolic and bariatric surgery. Surg Obes Relat Dis. 2015;11(3):489–506. https://doi.org/10.1016/j.soard.2015.02.003.
Herbella FA, Sweet MP, Tedesco P, et al. Gastroesophageal reflux disease and obesity. Pathophysiology and implications for treatment. J Gastrointest Surg. 2007;11(3):286–90. https://doi.org/10.1007/s11605-007-0097-z.
El-Serag HB, Graham DY, Satia JA, et al. Obesity is an independent risk factor for GERD symptoms and erosive esophagitis. Am J Gastroenterol. 2005;100(6):1243–50. https://doi.org/10.1111/j.1572-0241.2005.41703.x.
Hampel H, Abraham NS, El-Serag HB. Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann Intern Med. 2005;143(3):199–211. https://doi.org/10.7326/0003-4819-143-3-200508020-00006.
Borbély Y, Schaffner E, Zimmermann L, et al. De novo gastroesophageal reflux disease after sleeve gastrectomy: role of preoperative silent reflux. Surg Endosc. 2019;33(3):789–93. https://doi.org/10.1007/s00464-018-6344-4.
Yeung KTD, Penney N, Ashrafian L, et al. Does sleeve gastrectomy expose the distal esophagus to severe reflux?: a systematic review and meta-analysis. Ann Surg. 2020;271(2):257–65. https://doi.org/10.1097/SLA.0000000000003275.
Thereaux J, Barsamian C, Bretault M, et al. pH monitoring of gastro-oesophageal reflux before and after laparoscopic sleeve gastrectomy. Br J Surg. 2016;103(4):399–406. https://doi.org/10.1002/bjs.10089.
Genco A, Soricelli E, Casella G, et al. Gastroesophageal reflux disease and Barrett’s esophagus after laparoscopic sleeve gastrectomy: a possible, underestimated long-term complication. Surg Obes Relat Dis. 2017;13(4):568–74. https://doi.org/10.1016/j.soard.2016.11.029.
Himpens J, Dapri G, Cadière GB. A prospective randomized study between laparoscopic gastric banding and laparoscopic isolated sleeve gastrectomy: results after 1 and 3 years. Obes Surg. 2006;16(11):1450–6. https://doi.org/10.1381/096089206778869933.
Melissas J, Leventi A, Klinaki I, et al. Alterations of global gastrointestinal motility after sleeve gastrectomy: a prospective study. Ann Surg. 2013;258(6):976–82. https://doi.org/10.1097/SLA.0b013e3182774522.
Georgia D, Stamatina T, Maria N, et al. 24-h multichannel intraluminal impedance pH-metry 1 year after laparocopic sleeve gastrectomy: an objective assessment of gastroesophageal reflux disease. Obes Surg. 2017;27(3):749–53. https://doi.org/10.1007/s11695-016-2359-x.
Petersen WV, Meile T, Küper MA, et al. Functional importance of laparoscopic sleeve gastrectomy for the lower esophageal sphincter in patients with morbid obesity. Obes Surg. 2012;22(3):360–6. https://doi.org/10.1007/s11695-011-0536-5.
Braghetto I, Lanzarini E, Korn O, et al. Manometric changes of the lower esophageal sphincter after sleeve gastrectomy in obese patients. Obes Surg. 2010;20(3):357–62. https://doi.org/10.1007/s11695-009-0040-3.
Jobe BA, Kahrilas PJ, Vernon AH, et al. Endoscopic appraisal of the gastroesophageal valve after antireflux surgery. Am J Gastroenterol. 2004;99(2):233–43. https://doi.org/10.1111/j.1572-0241.2004.04042.x.
Zifan A, Kumar D, Cheng LK, et al. Three-dimensional myoarchitecture of the lower esophageal sphincter and esophageal hiatus using optical sectioning microscopy. Sci Rep. 2017;7(1):13188. https://doi.org/10.1038/s41598-017-13342-y.
Quero G, Fiorillo C, Dallemagne B, et al. The causes of gastroesophageal reflux after laparoscopic sleeve gastrectomy: quantitative assessment of the structure and function of the esophagogastric junction by magnetic resonance imaging and high-resolution manometry. Obes Surg. 2020;30(6):2108–17. https://doi.org/10.1007/s11695-020-04438-y.
Peterli R, Wölnerhanssen BK, Vetter D, et al. Laparoscopic sleeve gastrectomy versus roux-Y-gastric bypass for morbid obesity-3-year outcomes of the prospective randomized Swiss Multicenter Bypass Or Sleeve Study (SM-BOSS). Ann Surg. 2017;265(3):466–73. https://doi.org/10.1097/SLA.0000000000001929.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• LSG led to a considerable rate of postoperative “de novo” GERD.
• The clearance of acid in the distal esophagus is decreased after sleeve gastrectomy.
• Patients with symptomatic GERD do not experience an improvement after LSG.
• Preoperative study of GERD symptomatology and EGD seems appropriate.
Rights and permissions
About this article
Cite this article
Sancho Moya, C., Bruna Esteban, M., Sempere García-Argüelles, J. et al. The Impact of Sleeve Gastrectomy on Gastroesophageal Reflux Disease in Patients with Morbid Obesity. OBES SURG 32, 615–624 (2022). https://doi.org/10.1007/s11695-021-05808-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05808-w