Abstract
Background
Metabolic and bariatric surgery is an effective strategy to curb the natural history of obesity progression and improve psychosocial status in the short term for adolescents with severe obesity. The medium- and long-term psychosocial impact of bariatric surgery in this population is not established.
Methods
We searched MEDLINE (Ovid), EMBASE, Web of Science, PsycInfo, and the Cochrane Libraries through October 2017 for reports of weight loss surgery (roux-en-Y gastric bypass, sleeve gastrectomy, and adjustable gastric banding) on adolescents with severe obesity (age ≤ 21 years) having ≥ 6 months of follow-up. The primary outcome for inclusion in systematic review was use of a validated quality of life (QoL) or other psychosocial instrument at baseline and postoperatively. We used standardized mean difference (SMD) and random-effects modeling to provide summary estimates across different instruments.
Results
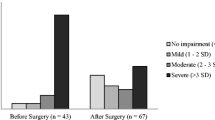
We reviewed 5155 studies, of which 20 studies met inclusion criteria for qualitative synthesis. There were 14 studies and 9 unique cohorts encompassing 573 patients which were eligible for meta-analysis regarding postoperative change in QoL. Across surgical procedures, there was significant improvement in QoL of 1.40 SMD (95% confidence interval 0.95 to 1.86; I2 = 89%; p < 0.001) at last follow-up (range 9–94 months). Trends in QoL improvement demonstrated the greatest improvement at 12 months; however, significant improvement was sustained at longest follow-up of 60+ months.
Conclusions
Weight loss surgery is associated with sustained improvement in QoL for adolescents with severe obesity across surgical procedures. Long-term data for psychosocial outcomes reflecting other mental health domains is lacking.





Similar content being viewed by others
References
Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2014;384(9945):766–81.
Ogden CL, Fryar CD, Hales CM, et al. Differences in obesity prevalence by demographics and urbanization in US children and adolescents, 2013-2016. JAMA. 2018;319(23):2410–8.
Pulgaron ER. Childhood obesity: a review of increased risk for physical and psychological comorbidities. Clin Thera. 2013;35(1):A18–32.
Kindel TL, Lomelin D, McBride C, et al. Plateaued national utilization of adolescent bariatric surgery despite increasing prevalence of obesity-associated co-morbidities. Surg Obes Relat Dis. 2016 May;12(4):868–73.
Wang Y, Beydoun MA, Liang L, et al. Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity (Silver Spring). 2008;16(10):2323–30.
Chung A, Backholer K, Wong E, et al. Trends in child and adolescent obesity prevalence in economically advanced countries according to socioeconomic position: a systematic review. Obes Rev. 2016;17(3):276–95.
Kelly AS, Barlow SE, Rao G, et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches. Circulation. 2013;128(15):1689–712.
Danielsson P, Kowalski J, Ekblom O, et al. Response of severely obese children and adolescents to behavioral treatment. Arch Pediatr Adolesc Med. 2012;166(12):1103–8.
Knop C, Singer V, Uysal Y, et al. Extremely obese children respond better than extremely obese adolescents to lifestyle interventions. Pediatr Obes. 2015;10(1):7–14.
Black JA, White B, Viner RM, et al. Bariatric surgery for obese children and adolescents: a systematic review and meta-analysis. Obes Rev. 2013;14(8):634–44.
Stefater MA, Inge TH. Bariatric surgery for adolescents with type 2 diabetes: an emerging therapeutic strategy. Current Diab Rep. 2017;17(8):62.
Olbers T, Beamish AJ, Gronowitz E, Flodmark CE, Dahlgren J, Bruze G, et al. Laparoscopic Roux-en-Y gastric bypass in adolescents with severe obesity (AMOS): a prospective, 5-year, Swedish nationwide study. Lancet Diabetes Endocrinol. 2017 2017-1-1;5(3):174–83.
Inge TH, Courcoulas AP, Jenkins TM, et al. Weight loss and health status 3 years after bariatric surgery in adolescents. N Engl J Med. 2016;374(2):113–23.
Schwimmer JB, Burwinkle TM, Varni JW. Health-related quality of life of severely obese children and adolescents. JAMA. 2003;289(14):1813–9.
Byrne ML, O’Brien-Simpson NM, Mitchell SA, et al. Adolescent-onset depression: are obesity and inflammation developmental mechanisms or outcomes? Child Psychiatry Hum Dev. 2015;46(6):839–50.
Herget S, Rudolph A, Hilbert A, et al. Psychosocial status and mental health in adolescents before and after bariatric surgery: a systematic literature review. Obes Facts. 2014;7(4):233–45.
Hillstrom KA, Graves JK. A review of depression and quality of life outcomes in adolescents post bariatric surgery. J Child Adolesc Psychiatr Nurs. 2015;28(1):50–9.
Paulus GF, de Vaan LE, Verdam FJ, et al. Bariatric surgery in morbidly obese adolescents: a systematic review and meta-analysis. Obes Surg. 2015;25(5):860–78.
White B, Doyle J, Colville S, et al. Systematic review of psychological and social outcomes of adolescents undergoing bariatric surgery, and predictors of success. Clin Obes. 2015;5(6):312–24.
Shoar S, Mahmoudzadeh H, Naderan M, et al. Long-term outcome of bariatric surgery in morbidly obese adolescents: a systematic review and meta-analysis of 950 patients with a minimum of 3 years follow-up. Obes Surg. 2017;2:02.
Trooboff S, Stucke R, Kulkarni A,et al. Psychosocial outcomes following adolescent bariatric surgery: a systematic review and meta-analysis. PROSPERO 2018 CRD42018089023 Available from: http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42018089023
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–34.
Higgins JPT GSe. Cochrane Handbook for Systematic Reviews of Interventions: the Cochrane Collaboration; 2011. Available from: www.cochrane-handbook.org.
McHorney CA, Ware JE, Raczek AE. The MOS 36-item short-form health survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care 1993;31(3):247–263.
Mourad Ouzzani HH, Zbys Fedorowicz, Ahmed Elmagarmid. Rayyan - a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210.
Noble M, Tregear SJ, Treadwell JR, et al. Long-term opioid therapy for chronic noncancer pain: a systematic review and meta-analysis of efficacy and safety. J Pain Symptom Manag. 2008;35(2):214–28.
Review Manager (RevMan) computer program, version 5.3. Copenhagen, Denmark: the Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Silberhumer GR, Miller K, Pump A, Kriwanek S, Widhalm K, Gyoeri G, Prager G Long-term results after laparoscopic adjustable gastric banding in adolescent patients: follow-up of the Austrian experience. Surg Endosc 2011;25(9):2993–9, 2999.
Sysko R, Devlin MJ, Hildebrandt TB, et al. Psychological outcomes and predictors of initial weight loss outcomes among severely obese adolescents receiving laparoscopic adjustable gastric banding. J Clin Psychol. 2012;73(10):1351–7.
Peña AS, Delko T, Couper R, et al. Laparoscopic adjustable gastric banding in Australian adolescents: should it be done? Obes Surg. 2017;27(7):1667–73.
Ratcliff MB, Eshleman KE, Reiter-Purtill J, et al. Prospective changes in body image dissatisfaction among adolescent bariatric patients: the importance of body size estimation. Surg Obes Relat Dis. 2012;8(4):470–5.
O'Brien P, Sawyer S, Laurie C, et al. Laparoscopic adjustable gastric banding in severely obese adolescents: a randomized trial. JAMA. 2010;303(6):519–26. Erratum in: JAMA. 2010 Jun;303(23):2357
Jarvholm K, Karlsson J, Olbers T, et al. Two-year trends in psychological outcomes after gastric bypass in adolescents with severe obesity. Obesity (Silver Spring). 2015;23(10):1966–72.
El-Matbouly MA, Khidir N, Touny HA, et al. A 5-year follow-up study of laparoscopic sleeve gastrectomy among morbidly obese adolescents: does it improve body image and prevent and treat diabetes? Obes Surg. 2018;28(2):513–9.
Hervieux E, Baud G, Dabbas M, et al. Comparative results of gastric banding in adolescents and young adults. J Pediatr Surg. 2016;51(7):1122–5.
Schmitt F, Riquin E, Beaumesnil M, et al. Laparoscopic adjustable gastric banding in adolescents: results at two years including psychosocial aspects. J Pediatr Surg. 2016 2016;51(3):403–8.
Aldaqal SM, Sehlo MG. Self-esteem and quality of life in adolescents with extreme obesity in Saudi Arabia: the effect of weight loss after laparoscopic sleeve gastrectomy. Gen Hosp Psychiatry. 2013;35(3):259–64.
Järvholm K, Olbers T, Flodmark CE, et al. Weight-related psychosocial problems in adolescents before and over 5 years after bariatric surgery-results from a Swedish nationwide study AMOS [abstract]. Obes Facts. 2016;9(suppl 1):295.
Zeller MH, Pendery EC, Reiter-Purtill J, et al. From adolescence to young adulthood: trajectories of psychosocial health following Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2017 2017-1-1;13(7):1196–203.
Holterman AX, Browne A, Tussing L, et al. A prospective trial for laparoscopic adjustable gastric banding in morbidly obese adolescents: an interim report of weight loss, metabolic and quality of life outcomes. J Pediatr Surg. 2010;45(1):74–8. discussion 78-9
Manco M, Mosca A, De Peppo F, et al. The benefit of sleeve gastrectomy in obese adolescents on nonalcoholic steatohepatitis and hepatic fibrosis. J Pediatr. 2017;180:31–37.e2.
Zeller MH, Reiter-Purtill J, Ratcliff MB, et al. Two-year trends in psychosocial functioning after adolescent roux-en-Y gastric bypass. Surg Obes Relat Dis. 2011;7(6):727–32.
Loux TJ, Haricharan RN, Clements RH, et al. Health-related quality of life before and after bariatric surgery in adolescents. J Pediatr Surg. 2008;43(7):1275–9.
Jong M, Hinnen C. Bariatric surgery in young adults: a multicenter study into weight loss, dietary adherence, and quality of life. Surg Obes Relat Dis. 2017;13(7):1204–10.
Ryder JR, Gross AC, Fox CK, et al. Factors associated with long-term weight-loss maintenance following bariatric surgery in adolescents with severe obesity. Int J Obes. 2018;42(1):102–7.
Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41(5):582–92.
Varni JW, Burwinkle TM, Seid M, et al. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr. 2003;3(6):329–41.
Pratt JSA, Browne A, Browne NT, et al. ASMBS pediatric metabolic and bariatric surgery guidelines, 2018. Surg Obes Relat Dis. 2018;14(7):882–901.
Hunsaker SL, Garland BH, Rofey D, et al. A multisite 2-year follow up of psychopathology prevalence, predictors, and correlates among adolescents who did or did not undergo weight loss surgery. J Adolesc Health. 2018;63(2):142–50.
Li L, Wu L-T. Substance use after bariatric surgery: a review. J Psychiatr Res. 2016;76:16–29.
Marino JM, Ertelt TW, Lancaster K, et al. The emergence of eating pathology after bariatric surgery: a rare outcome with important clinical implications. Int J Eat Disord. 2012;45(2):179–84.
Tindle HA, Omalu B, Courcoulas A, et al. Risk of suicide after long-term follow-up from bariatric surgery. Am J Med. 2010;123(11):1036–42.
Price KL, Lee ME, Washington GA, et al. The psychologist’s role in ethical decision making: adolescent bariatric surgery. Clin Pract Pediatr Psychol. 2015;3(4):359–64.51.
Hofmann B. Bariatric surgery for obese children and adolescents: a review of the moral challenges. BMC Med Ethics. 2013;14(1):18.
Göteborg University. Randomized Controlled Trial; Medical vs Bariatric Surgery for Adolescents (13–16 y) With Severe Obesity (AMOS-RCT). 2014 Aug 26 [cited 2018 Dec 1; updated 2018 Aug 8]. In: ClinicalTrials.gov [Internet]. Bethesda (MD): U.S. National Library of Medicine; 2000. Available from: https://clinicaltrials.gov/ct2/show/NCT02378259 Identifier: NCT02378259.
Acknowledgments
We are thankful for and gratefully acknowledge the guidance of Marc P. Michalsky, MD, and Meg H. Zeller, PhD, in helping to define the criteria for our search strategy as well as with the interpretation and framing of our results.
Funding
This material is based upon work supported by the Office of Academic Affiliations, Department of Veterans Affairs.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Statement of Human and Animal Rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
For this type of study, formal consent is not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary Appendix A
(DOCX 15 kb)
Supplementary Appendix B
Funnel plot of effect size versus standard error for studies included in meta-analysis of change in quality of life at last follow-up (PNG 402 kb)
Rights and permissions
About this article
Cite this article
Trooboff, S.W., Stucke, R.S., Riblet, N.B. et al. Psychosocial Outcomes Following Adolescent Metabolic and Bariatric Surgery: a Systematic Review and Meta-Analysis. OBES SURG 29, 3653–3664 (2019). https://doi.org/10.1007/s11695-019-04048-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-04048-3