Abstract
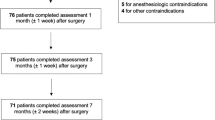
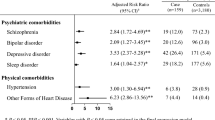
The objective our study was to carry out a systematic review and meta-analysis to examine the impact of attention-deficit and hyperactivity disorder (ADHD) on bariatric surgery outcomes. Despite the effectiveness of bariatric surgery, about 10 to 20% of patients continue to regain weight after the procedure. New evidence supports that ADHD may be directly associated with obesity and may affect outcomes following bariatric surgery. However, certain psychiatric illnesses, such as ADHD, are rarely screened for, leading to a continued lack of data on the interaction between ADHD and bariatric surgery. A comprehensive literature search for both published and unpublished studies of ADHD and bariatric surgery from 1946 to August 2018 was performed. The search was conducted using the Medline, EMBASE, Scopus, the Cochrane Library, and Web of Science databases as well as conference abstracts. Our search strategy terms included “(ADHD OR attention deficit hyperactivity disorder) AND (bariatrics OR obesity surgery OR gastric bypass OR gastric sleeve OR Roux-en-Y OR RYGB OR sleeve gastrectomy)” and was limited to human studies in the English language. Preliminary database search of the literature yielded 104 articles after 70 duplicates were removed. A total of five studies with 492 patients were included. The overall ADHD rate was 20.9% with reported rates ranging from 7 to 38%. The weighted mean age was 44.0 ± 10.2 years, the weighted sex was 83.6% female, and the weighted mean follow-up was 22.2 months. Preoperative weighted mean BMI was 43.7 versus a postoperative weighted mean BMI of 34.7. No statistical significance was observed for mean BMI difference between non-ADHD vs. ADHD patients undergoing bariatric surgery (three studies; MD − 2.66; CI − 7.54 to 2.13; p = 0.28). Statistical significance was, however, observed for postoperative follow-up between patients with ADHD vs. non-ADHD subjects (three studies; MD − 7.28; − 13.83 to −0.73; p = 0.03). Patients with ADHD do not have a statistically significant mean BMI difference following bariatric surgery but have a statistically significant reduction in postoperative follow-up versus non-ADHD patients. Targeted strategies aimed at improving clinic attendance for this at-risk ADHD population may improve bariatric outcomes and minimize recidivism rates.



Similar content being viewed by others
References
Morgan DJR, Ho KM, Armstrong J, et al. Long-term clinical outcomes and health care utilization after bariatric surgery: a population-based study. Ann Surg. 2015;262(1):86–92. https://doi.org/10.1097/SLA.0000000000000972.
Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366(17):1567–76. https://doi.org/10.1056/NEJMoa1200225.
Daigle CR, Corcelles R, Schauer PR. Primary silicone-banded laparoscopic sleeve gastrectomy: a pilot study. J Laparoendosc Adv Surg Tech A. 2015;25(2):94–7. https://doi.org/10.1089/lap.2014.0378.
Karmali S, Brar B, Shi X, et al. Weight recidivism post-bariatric surgery: a systematic review. Obes Surg. 2013;23:1922–33. https://doi.org/10.1007/s11695-013-1070-4.
Pedersen SD. The role of hormonal factors in weight loss and recidivism after bariatric surgery. Gastroenterol Res Pract. 2013;2013:1–9. https://doi.org/10.1155/2013/528450.
Tadross JA, le Roux CW. The mechanisms of weight loss after bariatric surgery. Int J Obes (Lond). 2009; https://doi.org/10.1038/ijo.2009.14.
Taymur I, Dilektas E, Budak E, et al. Relationship between symptoms of attention deficit hyperactivity disorder in childhood and mood in patients applying for bariatric surgery. Klin Psikofarmakol Bul. 2015;25:S89.
Alfonsson S, Sundbom M, Ghaderi A. Is age a better predictor of weight loss one year after gastric bypass than symptoms of disordered eating, depression, adult ADHD and alcohol consumption? Eat Behav. 2014;15(4):644–7. https://doi.org/10.1016/j.eatbeh.2014.08.024.
Nielsen F, Georgiadou E, Bartsch M, et al. Attention deficit hyperactivity disorder prevalence and correlates pre- and post-bariatric surgery: a comparative cross-sectional study. Obes Facts. 2017;10(1):1–11. https://doi.org/10.1159/000452999.
Taymur I, Budak E, Onen S, et al. The relationship between childhood and adult attention-deficit-hyperactivity disorder and general psychop athological features in individuals who apply for bariatric surgery. Bariatr Surg Pract Patient Care. 2016;11(3):116–22. https://doi.org/10.1089/bari.2016.0003.
Cortese S, Tessari L. Attention-deficit/hyperactivity disorder (ADHD) and obesity: update 2016. Curr Psychiatry Rep. 2017;19(1) https://doi.org/10.1007/s11920-017-0754-1.
Sandra Kooij JJ. ADHD and obesity. Am J Psychiatry. 2016;173(1):1–2. https://doi.org/10.1176/appi.ajp.2015.15101315.
Cortese S, Angriman M, Maffeis C, et al. Attention-deficit/hyperactivity disorder (ADHD) and obesity: a systematic review of the literature. Crit Rev Food Sci Nutr. 2008;48(6):524–37. https://doi.org/10.1080/10408390701540124.
Cortese S, Vincenzi B. Obesity and ADHD: clinical and neurobiological implications. Curr Top Behav Neurosci. 2012;9:199–218. https://doi.org/10.1007/7854_2011_154.
Williamson TM, Campbell TS, Telfer JA, et al. Emotion self-regulation moderates the association between symptoms of ADHD and weight loss after bariatric surgery. Obes Surg. 2018;28(6):1553–61. https://doi.org/10.1007/s11695-017-3037-3.
Marchesi DG, Ciriaco JGM, Miguel GPS, et al. Does the attention deficit hyperactivity disorder interfere with bariatric surgery results? TT - O Transtorno de Déficit de Atenção e Hiperatividade interfere nos resultados da cirurgia bariátrica? Rev Col Bras Cir. 2017;44(2):140–6. https://doi.org/10.1590/0100-69912017002006.
Nicolau J, Ayala L, Frances C, et al. Are subjects with criteria for adult attention-deficit/ hyperactivity disorder doing worse after bariatric surgery? A case-control study. Nutr Hosp. 2014;31(3):1052–8. https://doi.org/10.3305/nh.2015.31.3.8089.
Alfonsson S, Olsson E, Hursti T. The effects of therapist support and treatment presentation on the clinical outcomes of an Internet based applied relaxation program. Internet Interv. 2015;2(3):289–96. https://doi.org/10.1016/j.invent.2015.07.005.
Steinmann WC, Suttmoeller K, Chitima-Matsiga R, et al. Bariatric surgery: 1-year weight loss outcomes in patients with bipolar and other psychiatric disorders. Obes Surg. 2011;21(9):1323–9. https://doi.org/10.1007/s11695-011-0373-6.
Altfas JR. Prevalence of attention deficit/hyperactivity disorder among adults in obesity treatment. BMC Psychiatry. 2002;2:9. https://doi.org/10.1186/1471-244x-2-9. LB - Altfas2002
Altfas JR. Prevalence of attention deficit/hyperactivity disorder among adults in obesity treatment. BMC Psychiatry. 2002;2 https://doi.org/10.1186/1471-244X-2-9.
Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–6.
Higgins JPT GS. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. Cochrane Collab. 2011;Available.
Higgins JPT, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;3:557–60.
Marchesi DG, Ciriaco JGM, Miguel GPS, et al. Does the attention deficit hyperactivity disorder interfere with bariatric surgery results? Rev Col Bras Cir. 2017;44(2):140–6. https://doi.org/10.1590/0100-69912017002006.
Genro JP, Kieling C, Rohde LAHM. Attention-deficit/hyperactivity disorder and the dopaminergic hypotheses. Exper Rev Neurother. 2014;10(4)
Levy LD, Fleming JP, Klar D. Treatment of refractory obesity in severely obese adults following management of newly diagnosed attention deficit hyperactivity disorder. Int J Obes. 2009;33(3):326–34. https://doi.org/10.1038/ijo.2009.5.
Spitznagel MB, Alosco M, et al. Cognitive function predicts 24-month weight loss success after bariatric surgery. 2013;9 https://doi.org/10.1016/j.soard.2013.04.011.
Spitznagel MB, Alosco M, Galioto R, et al. The role of cognitive function in postoperative weight loss outcomes: 36-month follow-up. 2014:1078–84. https://doi.org/10.1007/s11695-014-1205-2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Authors 1, 2, 3, and 4: none to declare
Author 5 is a consultant and has received educational grants from Ethicon and Covidien, educational grants from Stryker, and teaching honoraria from Cook Surgery and Bard Davol.
Author 6 is a consultant for Gore Medical and Ethicon.
Ethical Approval and Consent
This article does not contain any studies with human participants or animals performed by any of the authors.
For this type of study, formal consent is not required. Informed consent does not apply.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mocanu, V., Tavakoli, I., MacDonald, A. et al. The Impact of ADHD on Outcomes Following Bariatric Surgery: a Systematic Review and Meta-analysis. OBES SURG 29, 1403–1409 (2019). https://doi.org/10.1007/s11695-019-03735-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03735-5