Abstract
Objective
The study was designed to examine changes of body fat distribution after laparoscopic sleeve gastrectomy (LSG) in obese male patients and to confirm whether these changes are correlated with increased testosterone.
Methods
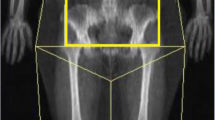
A total of 30 obese male patients with body mass index (BMI) 30–45 kg/m2 were enrolled in this study. Data on demographic characteristics, anthropometry, metabolic parameters, and body fat distribution were collected at baseline and 6 months after LSG. Body fat distribution was assessed by dual-energy X-ray absorptiometry (DXA).
Results
Six months after surgery, the BMI of participants (age 33.0 ± 9.5) decreased from 40.2 ± 5.2 to 30.8 ± 4.4 kg/m2, total testosterone increased from 2.4 ± 1.2 to 4.5 ± 1.8 ng/mL, and the percentage of testosterone deficiency in these patients decreased from 82.7 to 23.1%. Fat mass was significantly decreased in all regions, but the loss of fat mass in the android region was more than that in any other body region. After adjusting age and the BMI, the changes in android FM% and gynoid FM% were significantly correlated with an increase in total testosterone concentration (R2 = 0.187, R2 = 0.282, respectively).
Conclusion
In obese male patients with BMI 30–45 kg/m2, an increase of total testosterone correlated to the changes in android FM% and gynoid FM% at the sixth month after LSG surgery.

Similar content being viewed by others
References
Tajar A, Forti G, O'Neill TW, et al. Characteristics of secondary, primary, and compensated hypogonadism in aging men: evidence from the European male ageing study. J Clin Endocrinol Metab. 2010;95(4):1810–8. https://doi.org/10.1210/jc.2009-1796.
Kelly DM, Jones TH. Testosterone and obesity. Obes Rev. 2015;16(7):581–606. https://doi.org/10.1111/obr.12282.
Bann D, Wu FC, Keevil B, et al. Changes in testosterone related to body composition in late midlife: findings from the 1946 British birth cohort study. Obesity (Silver Spring). 2015;23(7):1486–92. https://doi.org/10.1002/oby.21092.
Couillard C, Gagnon J, Bergeron J, et al. Contribution of body fatness and adipose tissue distribution to the age variation in plasma steroid hormone concentrations in men: the HERITAGE Family Study. J Clin Endocrinol Metab. 2000;85(3):1026–31. https://doi.org/10.1210/jcem.85.3.6427.
Foulkes SJ, Daly RM, Fraser SF. The clinical importance of quantifying body fat distribution during androgen deprivation therapy for prostate cancer. Endocr Relat Cancer. 2017;24(3):R35–48. https://doi.org/10.1530/ERC-16-0505.
Frederiksen L, Hojlund K, Hougaard DM, et al. Testosterone therapy decreases subcutaneous fat and adiponectin in aging men. Eur J Endocrinol. 2012;166(3):469–76. https://doi.org/10.1530/EJE-11-0565.
Giannoulis MG, Martin FC, Nair KS, et al. Hormone replacement therapy and physical function in healthy older men. Time to talk hormones? Endocr Rev. 2012;33(3):314–77. https://doi.org/10.1210/er.2012-1002.
Botella-Carretero JI, Balsa JA, Gomez-Martin JM, et al. Circulating free testosterone in obese men after bariatric surgery increases in parallel with insulin sensitivity. J Endocrinol Investig. 2013;36(4):227–32. https://doi.org/10.3275/8469.
Calderon B, Galdon A, Calanas A, et al. Effects of bariatric surgery on male obesity-associated secondary hypogonadism: comparison of laparoscopic gastric bypass with restrictive procedures. Obes Surg. 2014;24(10):1686–92. https://doi.org/10.1007/s11695-014-1233-y.
Luconi M, Samavat J, Seghieri G, et al. Determinants of testosterone recovery after bariatric surgery: is it only a matter of reduction of body mass index? Fertil Steril. 2013;99(7):1872–9 e1871. https://doi.org/10.1016/j.fertnstert.2013.02.039.
O'Reilly MW, House PJ, Tomlinson JW. Understanding androgen action in adipose tissue. J Steroid Biochem Mol Biol. 2014;143:277–84. https://doi.org/10.1016/j.jsbmb.2014.04.008.
Navarro G, Allard C, Xu W, et al. The role of androgens in metabolism, obesity, and diabetes in males and females. Obesity (Silver Spring). 2015;23(4):713–9. https://doi.org/10.1002/oby.21033.
Mammi C, Calanchini M, Antelmi A, et al. Androgens and adipose tissue in males: a complex and reciprocal interplay. Int J Endocrinol. 2012;2012:789653.
Rosenthal RJ, International Sleeve Gastrectomy Expert P, Diaz AA, et al. International Sleeve Gastrectomy Expert Panel Consensus Statement: best practice guidelines based on experience of >12,000 cases. Surg Obes Relat Dis. 2012;8(1):8–19. https://doi.org/10.1016/j.soard.2011.10.019.
Li Y, Zhang M, Liu X, et al. Correlates and prevalence of hypogonadism in patients with early- and late-onset type 2 diabetes. Andrology. 2017;5(4):739–43. https://doi.org/10.1111/andr.12360.
Cooper LA, Page ST, Amory JK, et al. The association of obesity with sex hormone-binding globulin is stronger than the association with ageing—implications for the interpretation of total testosterone measurements. Clin Endocrinol. 2015;83(6):828–33. https://doi.org/10.1111/cen.12768.
Bhasin S, Cunningham GR, Hayes FJ, et al. Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95(6):2536–59. https://doi.org/10.1210/jc.2009-2354.
Sartorius G, Ly LP, Sikaris K, et al. Predictive accuracy and sources of variability in calculated free testosterone estimates. Ann Clin Biochem. 2009;46(Pt 2):137–43. https://doi.org/10.1258/acb.2008.008171.
Ly LP, Sartorius G, Hull L, et al. Accuracy of calculated free testosterone formulae in men. Clin Endocrinol. 2010;73(3):382–8. https://doi.org/10.1111/j.1365-2265.2010.03804.x.
Keelan JA, Mattes E, Tan H, et al. Androgen concentrations in umbilical cord blood and their association with maternal, fetal and obstetric factors. PLoS One. 2012;7(8):e42827. https://doi.org/10.1371/journal.pone.0042827.
Aarts E, van Wageningen B, Loves S, et al. Gonadal status and outcome of bariatric surgery in obese men. Clin Endocrinol. 2014;81(3):378–86. https://doi.org/10.1111/cen.12366.
Corona G, Rastrelli G, Monami M, et al. Body weight loss reverts obesity-associated hypogonadotropic hypogonadism: a systematic review and meta-analysis. Eur J Endocrinol. 2013;168(6):829–43. https://doi.org/10.1530/EJE-12-0955.
Mouser JG, Loprinzi PD, Loenneke JP. The association between physiologic testosterone levels, lean mass, and fat mass in a nationally representative sample of men in the United States. Steroids. 2016;115:62–6. https://doi.org/10.1016/j.steroids.2016.08.009.
Morrison SA, Goss AM, Azziz R, et al. Peri-muscular adipose tissue may play a unique role in determining insulin sensitivity/resistance in women with polycystic ovary syndrome. Hum Reprod. 2017;32(1):185–92. https://doi.org/10.1093/humrep/dew279.
Li W, Zhu L, Mo Z, et al. Effect of laparoscopic Roux-en-Y gastric bypass on body composition and insulin resistance in Chinese patients with type 2 diabetes mellitus. Obes Surg. 2014;24(4):578–83. https://doi.org/10.1007/s11695-013-1116-7.
Krotkiewski M, Bjorntorp P, Sjostrom L, et al. Impact of obesity on metabolism in men and women. Importance of regional adipose tissue distribution. J Clin Invest. 1983;72(3):1150–62. https://doi.org/10.1172/JCI111040.
Tchernof A, Despres JP. Pathophysiology of human visceral obesity: an update. Physiol Rev. 2013;93(1):359–404. https://doi.org/10.1152/physrev.00033.2011.
Kvist H, Chowdhury B, Grangard U, et al. Total and visceral adipose-tissue volumes derived from measurements with computed tomography in adult men and women: predictive equations. Am J Clin Nutr. 1988;48(6):1351–61. https://doi.org/10.1093/ajcn/48.6.1351.
Kuk JL, Lee S, Heymsfield SB, et al. Waist circumference and abdominal adipose tissue distribution: influence of age and sex. Am J Clin Nutr. 2005;81:1330–4.
Gruenewald DA, Matsumoto AM. Testosterone supplementation therapy for older men: potential benefits and risks. J Am Geriatr Soc. 2003;51(1):101–15; discussion 115. https://doi.org/10.1034/j.1601-5215.2002.51018.x.
Wittert GA, Chapman IM, Haren MT, et al. Oral testosterone supplementation increases muscle and decreases fat mass in healthy elderly males with low-normal gonadal status. J Gerontol A Biol Sci Med Sci. 2003;58:618–25.
Caprio M, Fabbrini E, Isidori AM, et al. Leptin in reproduction. Trends Endocrinol Metab. 2001;12(2):65–72. https://doi.org/10.1016/S1043-2760(00)00352-0.
Laughlin GA, Ix JH, Cummins K, et al. Extremes of an aromatase index predict increased 25-year risk of cardiovascular mortality in older women. Clin Endocrinol. 2012;77(3):391–8. https://doi.org/10.1111/j.1365-2265.2011.04287.x.
Blouin K, Boivin A, Tchernof A. Androgens and body fat distribution. J Steroid Biochem Mol Biol. 2008;108(3-5):272–80. https://doi.org/10.1016/j.jsbmb.2007.09.001.
Acknowledgments
The present study would not have been possible without the participation of these patients. This study is supported by grants from the Chinese National Natural Science Foundation (No. 81601269) and Shanghai Sailing Program (16YF1408900).
Author information
Authors and Affiliations
Contributions
JG and MZ analyzed the data and drafted the manuscript. JG, MZ, and SQ designed the study and directed implementation and data collection. JG, CZ, XW, and YZ collected the data. QL and LL provided necessary logistical support. DZ performed the surgery and participated in the discussion of this manuscript. MZ and SQ edited the manuscript for intellectual content and provided critical comments on the manuscript.
Corresponding author
Ethics declarations
Informed consent was obtained from all individual participants included in the study. The study was approved by the ethics committee of Shanghai Tenth People’s Hospital.
Conflict of Interest
The authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Gao, J., Zhang, M., Zhu, C. et al. The Change in the Percent of Android and Gynoid Fat Mass Correlated with Increased Testosterone After Laparoscopic Sleeve Gastrectomy in Chinese Obese Men: a 6-Month Follow-Up. OBES SURG 28, 1960–1965 (2018). https://doi.org/10.1007/s11695-018-3116-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3116-0