Abstract
Objective
To investigate whether Naoxueshu Oral Liquid (NXS) could promote hematoma absorption in post-craniotomy hematoma (PCH) patients.
Methods
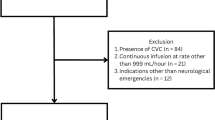
This is an open-label, multicenter, and randomized controlled trial conducted at 9 hospitals in China. Patients aged 18–80 years with post-craniotomy supratentorial hematoma volume ranging from 10 to 30 mL or post-craniotomy infratentorial hematoma volume less than 10 mL, or intraventricular hemorrhage following cranial surgery were enrolled. They were randomly assigned at a 1:1 ratio to the NXS (10 mL thrice daily for 15 days) or control groups using a randomization code table. Standard medical care was administered in both groups. The primary outcome was the percentage reduction in hematoma volume from day 1 to day 15. The secondary outcomes included the percentage reduction in hematoma volume from day 1 to day 7, the absolute reduction in hematoma volume from day 1 to day 7 and 15, and the change in neurological function from day 1 to day 7 and 15. The safety was closely monitored throughout the study. Moreover, subgroup analysis was performed based on age, gender, history of diabetes, and etiology of intracerebral hemorrhage (ICH).
Results
A total of 120 patients were enrolled and randomly assigned between March 30, 2018 and April 15, 2020. One patient was lost to follow-up in the control group. Finally, there were 119 patients (60 in the NXS group and 59 in the control group) included in the analysis. In the full analysis set (FAS) analysis, the NXS group had a greater percentage reduction in hematoma volume from day 1 to day 15 than the control group [median (Q1, Q3): 85% (71%, 97%) vs. 76% (53%, 93%), P<0.05]. The secondary outcomes showed no statistical significance between two groups, either in FAS or per-protocol set (P>0.05). Furthermore, no adverse events were reported during the study. In the FAS analysis, the NXS group exhibited a higher percentage reduction in hematoma volume on day 15 in the following subgroups: male patients, patients younger than 65 years, patients without diabetes, or those with initial cranial surgery due to ICH (all P<0.05).
Conclusions
The administration of NXS demonstrated the potential to promote the percentage reduction in hematoma volume from day 1 to day 15. This intervention was found to be safe and feasible. The response to NXS may be influenced by patient characteristics. (Registration No. ChiCTR1800017981)
Similar content being viewed by others
References
Lopez Ramos C, Brandel MG, Rennert RC, Wali AR, Steinberg JA, Santiago-Dieppa DR, et al. Clinical risk factors and postoperative complications associated with unplanned hospital readmissions after cranial neurosurgery. World Neurosurg 2018;119:e294–e300.
Wang C, Niu X, Ren Y, Lan Z, Zhang Y. Risk factors for postoperative intracranial hemorrhage after resection of intracranial tumor in 2259 consecutive patients. World Neurosurg 2019;129:e663–e668.
Dobran M, di Somma LGM, Paracino R. Haemostatic technique in malignant gliomas. Neurol Neurochir Pol 2022;56:499–502.
Chen R, Wang X, Anderson CS, Robinson T, Lavados PM, Lindley RI, et al. Infratentorial intracerebral hemorrhage: relation of location to outcome. Stroke 2019;50:1257–1259.
Dasenbrock HH, Yan SC, Chavakula V, Gormley WB, Smith TR, Claus EB, et al. Unplanned reoperation after craniotomy for tumor: a national surgical quality improvement program analysis. Neurosurgery 2017;81:761–771.
Lillemäe K, Järviö JA, Silvasti-Lundell MK, Antinheimo JJP, Hernesniemi JA, Niemi TT. Incidence of postoperative hematomas requiring surgical treatment in neurosurgery: a retrospective observational study. World Neurosurg 2017;108:491–497.
Kerezoudis P, Glasgow AE, Alvi MA, Spinner RJ, Meyer FB, Bydon M, et al. Returns to operating room after neurosurgical procedures in a tertiary care academic medical center: implications for health care policy and quality improvement. Neurosurgery 2019;84:E392–E401.
Kerezoudis P, Alvi MA, Spinner RJ, Meyer FB, Habermann EB, Bydon M. Predictors of unplanned returns to the operating room within 30 days in neurosurgery: insights from a national surgical registry. World Neurosurg 2019;123:e348–e370.
Song J, Nie Y, Wang P, Lu H, Gao L. Naoxueshu relieves hematoma after clot removal in acute spontaneous intracerebral hemorrhage. Brain Behav 2021;11:e01957.
Song J, Nie Y, Qin X, Wang P, Lu H, Gao L. Efficacy of Naoxueshu in acute spontaneous intracerebral hemorrhage: a multicenter observational study. Neurol Sci 2022;43:1885–1891.
Qiu J, Wang LN, Hu JH, Zhang YQ. Oral administration of leeches (Shuizhi): a review of the mechanisms of action on antiplatelet aggregation. J Ethnopharmacol 2019;232:103–109.
Chen JR, Xie XF, Zhang HQ, Li GM, Yin YP, Cao XY, et al. Pharmacological activities and mechanisms of hirudin and its derivatives—a review. Front Pharmacol 2021;12:660757.
Li Y, Tian C, Wei Y, Liu H, An N, Song K, et al. Exploring the pharmacological mechanism of Naoxueshu Oral Liquid in the treatment of intracerebral hemorrhage through weighted gene co-expression network analysis, network pharmacological and experimental validation. Phytomedicine 2023;108:154530.
Cao Y, Yu S, Zhang Q, Yu T, Liu Y, Sun Z, et al. Chinese Stroke Association guidelines for clinical management of cerebrovascular disorders: executive summary and 2019 update of clinical management of intracerebral haemorrhage. Stroke Vasc Neurol 2020;5:396–402.
Hemphill JC, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2015;46:2032–2060.
Ali M, Maragkos GA, Yaeger KA, Schupper AJ, Hardigan TA, Vasan V, et al. Initial experience with minimally invasive endoscopic evacuation of intracerebral hemorrhage in the setting of radiographic herniation. J Stroke Cerebrovasc Dis 2023;32:107309.
Eilertsen H, Menon CS, Law ZK, Chen C, Bath PM, Steiner T, et al. Haemostatic therapies for stroke due to acute, spontaneous intracerebral haemorrhage. Cochrane Database Syst Rev 2023;10:CD005951.
Wu L, Li Y, Wang X, Ren X, Zhu H, Sun Y, et al. A systematic review and meta-analysis on the treatment of cerebral hemorrhage with Naoxueshu Oral Liquid. BioMed Res Int 2017;2017:1–11.
Song J, Lyu Y, Wang P, Nie Y, Lu H, Gao L, et al. Treatment of Naoxueshu promotes improvement of hematoma absorption and neurological function in acute intracerebral hemorrhage patients. Front Physiol 2018;9:933.
Jiang H, Qin Y, Liu T, Zhang L, Wang M, Qin B, et al. Nao-Xue-Shu Oral Liquid protects and improves secondary brain insults of hypertensive cerebral hemorrhage. Evid Based Complement Altern Med 2016;2016:9121843.
Zheng Y, Ren W, Zhang L, Zhang Y, Liu D, Liu Y. A review of the pharmacological action of Astragalus polysaccharide. Front Pharmacol 2020;11:349.
Zhang CH, Yang X, Wei JR, Chen NMH, Xu JP, Bi YQ, et al. Ethnopharmacology, phytochemistry, pharmacology, toxicology and clinical applications of Radix Astragali. Chin J Integr Med 2021;27:229–240.
Li CX, Liu Y, Zhang YZ, Li JC, Lai J. Astragalus polysaccharide: a review of its immunomodulatory effect. Arch Pharm Res 2022;45:367–389.
Pan R, Zhou M, Zhong Y, Xie J, Ling S, Tang X, et al. The combination of Astragalus membranaceus extract and ligustrazine to improve the inflammation in rats with thrombolytic cerebral ischemia. Int J Immunopathol Pharmacol 2019;33:205873841986905.
Li X, Zhu Z, Gao S, Zhang L, Cheng X, Li S, et al. Inhibition of fibrin formation reduces neuroinflammation and improves long-term outcome after intracerebral hemorrhage. Int Immunopharmacol 2019;72:473–478.
Kaye AD, Manchikanti L, Novitch MB, Mungrue IN, Anwar M, Jones MR, et al. Responsible, safe, and effective use of antithrombotics and anticoagulants in patients undergoing interventional techniques: American Society of Interventional Pain Physicians (ASIPP) Guidelines. Pain Physician 2019;22(1S):S75–128.
Huang S, Xu F, Wang YY, Shang MY, Wang CQ, Wang X, et al. Improvement and application of acute blood stasis rat model aligned with the 3Rs (Reduction, Refinement and Replacement) of humane animal experimentation. Chin J Integr Med 2020;26:292–298.
Büyükkaragöz B, Bakkaloǧlu SA. Serum osmolality and hyperosmolar states. Pediatr Nephrol Berl Ger 2023;38:1013–1025.
Gong Y, Wang Y, Chen D, Teng Y, Xu F, Yang P. Predictive value of hyperglycemia on prognosis in spontaneous intracerebral hemorrhage patients. Heliyon 2023;9:e14290.
Tu WJ, Wang LD, Special Writing Group of China Stroke Surveillance Report. China stroke surveillance report 2021. Mil Med Res 2023;10:33.
Liu J, Zhu Z, Leung GKK. Erythrophagocytosis by microglia/macrophage in intracerebral hemorrhage: from mechanisms to translation. Front Cell Neurosci 2022;16:818602.
Vaibhav K, Braun M, Khan MB, Fatima S, Saad N, Shankar A, et al. Remote ischemic post-conditioning promotes hematoma resolution via AMPK-dependent immune regulation. J Exp Med 2018;215:2636–2654.
Nikolich-Žugich J. The twilight of immunity: emerging concepts in aging of the immune system. Nat Immunol 2018;19:10–19.
Huang Z, Chen B, Liu X, Li H, Xie L, Gao Y, et al. Effects of sex and aging on the immune cell landscape as assessed by single-cell transcriptomic analysis. Proc Natl Acad Sci 2021;118:e2023216118.
Shepherd R, Cheung AS, Pang K, Saffery R, Novakovic B. Sexual dimorphism in innate immunity: the role of sex hormones and epigenetics. Front Immunol 2021;11:604000.
Massicotte S, Lun R, Yogendrakumar V, Dewar B, Davies A, Fergusson DA, et al. Natural history of recovery after intracerebral haemorrhage: a scoping review protocol. BMJ Open 2020;10:e039460.
Acknowledgments
We would like to express our gratitude to the patients enrolled, as well as the nurses, clinical staff, and staff of the clinical research coordinator, clinical research associate for their valuable support and contributions to the study.
Author information
Authors and Affiliations
Contributions
Wang AX, Wang DL and Kang DZ contributed to conceptualizing and designing the trial; He Q, Lin FX, Su JY, and Zhuo LY cleaned, analyzed, and interpreted the data; Lin FX and He Q wrote the manuscript; Zhu Q, Sun XC, Jiang RC, Yao ZG, Wang L, Dang YW, Liu DZ, Liu Y, Fang WH, Wang FY, and Lin YX recruited the patients and collected data. All authors have approved the final manuscript as submitted and have agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
All authors have declared that they have no conflict of interest.
Additional information
Supported by the Technology Platform Construction Project of Fujian Province (No. 2021Y2001 and 2020Y2003)
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
He, Q., Lin, Fx., Su, Jy. et al. Naoxueshu Oral Liquid Accelerates Post-Craniotomy Hematoma Absorption in Patients: An Open-Label, Multicenter, and Randomized Controlled Trial. Chin. J. Integr. Med. (2024). https://doi.org/10.1007/s11655-024-3902-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s11655-024-3902-6