Abstract
Background
Difficulty performing basic daily activities such as bathing and dressing (“functional impairment”) affects more than 15% of middle-aged people, and this proportion is increasing. Little is known about the experiences and needs of individuals who develop functional impairment in middle age.
Objective
To examine the experiences and needs of adults who developed functional impairment in middle age.
Design
Qualitative study using semi-structured interviews.
Participants
Forty patients aged 50–64 years who developed functional impairment in middle age, recruited from four primary care clinics in San Francisco.
Approach
Interviews included open-ended questions about participants’ daily life, ability to perform activities of daily living (ADLs), and needs related to functional impairment. We analyzed interviews using qualitative thematic analysis.
Key Results
Interviews revealed several themes related to the psychosocial and physical impacts of developing functional impairment in middle age. Participants noted that losses associated with functional impairment, such as loss of independence, control, and social roles, caused conflict in their sense of identity. To cope with these losses, participants used strategies including acceptance, social comparison, adjusting standards, and engaging in valued life activities. Participants reflected on the intersection of their functional impairment with the aging process, noting that their impairments seemed premature compared to the more “natural” aging process in older adults. In terms of physical impacts, participants described how a lack of accommodations in the built environment exacerbated their impairments. While participants used behavioral strategies to overcome these challenges, unmet needs remained, resulting in downstream physical and psychological impacts including safety risks, falls, frustration, and fear.
Conclusions
Unmet psychosocial and physical needs were common among middle-aged adults with functional impairment and led to negative downstream effects. Eliciting and addressing unmet needs may help mitigate downstream health consequences for this growing population, optimizing function and quality of life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Difficulty performing basic activities of daily living (ADLs) such as bathing and dressing (“functional impairment”) is often seen as a problem that affects older adults. However, 15% of middle-aged adults (i.e., 45–64 years) have functional impairment, and this percentage is growing.1,2,3,4,5,6,7,8,9 The reason for this increase is an area of active investigation, but risk factors include lower levels of education and lower economic well-being.9,10,11 Developing functional impairment in middle age is associated with adverse outcomes similar to those among older adults, including hospitalization and nursing home admission.12,13,14 Yet little is known about the experiences and clinical needs of middle-aged people who develop functional impairment.15
Developing functional impairment in adulthood is associated with poorer self-rated health compared to developing impairment in childhood or having congenital impairment.15,16 Moreover, middle-aged adults with functional impairment have worse self-reported health compared to both younger and older adults.15,16 While the reasons for these differences are unknown, they may be related to difficulty adapting to functional impairment in middle age17,18,19,20,21,22,23,24,25,26,27,28 or to life course factors such as changing work and family relationships. Developing impairment in middle age may also impact an individual’s perception of their aging process, including concerns that they are aging “prematurely.”29 Although prior qualitative studies have examined the experiences of adults of all ages who develop functional impairment,16,17,18,19,20,21,22,23,24,25,26,27,28,30,31,32 they have not specifically examined the experiences of middle-aged people.33
We conducted a qualitative study to examine the experiences and needs of adults who develop functional impairment during middle age. To explore the intersection between functional impairment and the aging process, we focused on adults aged 50–64, in whom aging-related chronic conditions are especially common.34 To inform interventions to improve clinical care for this population, we applied these findings to develop a conceptual model illustrating the impacts of impairment that develops in middle age.
METHODS
Study Design
We conducted qualitative interviews to understand the experiences and needs of patients who developed functional impairment in middle age. The institutional review boards of the University of California, San Francisco, the San Francisco Veterans Affairs Medical Center, and the University of Pennsylvania approved the study.
Setting and Participants
We recruited participants from four primary care practices in San Francisco: two community-based academic practices, a Veterans Affairs hospital-based practice, and a hospital-based academic safety-net practice; to ensure depth of understanding, we purposefully sampled from two clinics serving patients with lower socioeconomic status and two serving patients with average socioeconomic status. To identify participants, we obtained lists of patients aged 50–64 for providers in each practice, excluding patients without a telephone number and address. Providers reviewed lists to identify potentially eligible individuals. Eligibility criteria included English- or Spanish-speaking; having difficulty or needing help with one or more ADLs (bathing, dressing, toileting, transferring, eating, walking across a room); developing that difficulty in middle age (45–64 years); and having decision-making capacity. Potentially eligible patients received a letter including a study description, a consent form, and a toll-free opt-out telephone number. Patients not opting out within a week after the letter was sent were contacted by telephone.
During telephone screenings, study staff confirmed eligibility and excluded patients who were unable to communicate over the telephone or whom a caregiver identified as having cognitive impairment precluding an interview. We obtained informed consent using a teach-back method.35 Interested individuals were scheduled for in-person interviews.
Data Collection
The study team included three research assistants trained in qualitative methods (EX, MB, MJS), two medical anthropologists (FMN, KZ), and three clinician researchers (LK, MP, RTB). Between September 2017 and June 2018, EX, MB, and FMN conducted in-person interviews. FMN and RTB developed a semi-structured interview guide including open-ended questions about daily life, ability to perform ADLs and instrumental ADLs (IADLs, defined as cognitively complex activities such as using transportation or preparing meals), onset and etiology of functional impairment, and needs related to impairment. We pilot-tested the interview guide with the first five participants and revised it to reflect unanticipated topics and concepts.36 We conducted interviews until no new substantive information was obtained.37
We used a card sort activity to assess function. Cards included graphics and text describing ADLs and IADLs (shopping, preparing food, managing money, taking medication, doing housework, making phone calls, doing housework, using transportation). Participants categorized each activity as “easy,” “somewhat difficult,” or “difficult” to perform; those with difficulty reported if they needed help.38,39,40
Participants reported demographic characteristics (age, race/ethnicity, marital status), socioeconomic status (educational attainment, income), living situation (type of housing, number of people in the household), and self-rated quality of life (excellent, very good, good, fair, poor).41 Interviews lasted about one hour and were audio-recorded and transcribed verbatim.
Data Analysis
We used descriptive statistics to analyze demographic data. To classify etiology of functional impairment, we used International Classification of Diseases, 10th revision codes and grouped codes into broader categories. To analyze transcripts, we used qualitative thematic analysis with hybrid deductive and inductive coding.42 We developed deductive codes based on study aims and interview guide domains. First, EX, MB, and RTB independently reviewed three transcripts, applied deductive codes and developed inductive codes, and developed a preliminary codebook. Next, EX, MB, MJS, FMN, and RTB refined codes through serial review of transcripts to identify and develop themes. We discussed findings after each set of 3–5 independently coded transcripts. To resolve disagreements about the presence, scope, or definition of codes, we used discussion and consensus. During the analytic process, we developed a conceptual model to illustrate the impacts of functional impairment that develops in middle age. We used Rowe and Kahn’s Model of Successful Aging and Verbrugge’s Model of Disablement as frameworks for organizing themes related to adaptations, unmet needs, and consequences of impairment.43,44 We used ATLAS.ti to manage qualitative data (Version 8.2, Berlin, Scientific Software Development).
RESULTS
Participant Characteristics
Participants’ (n = 40) mean age was 57.6 years (SD, 3.7), 43% were women, and 50% were white (Table 1). Ten percent had less than a high school education, 15% had an annual household income < $10,000, and 20% lived in subsidized housing. Forty percent needed help with ≥ 3 ADLs, 28% needed help with 1–2 ADLs, and 32% had difficulty with ≥ 1 ADLs. The most common etiologies of functional impairment included injuries (33%), musculoskeletal conditions (23%), chronic pain (10%), and neurologic conditions (8%). Fifty percent of participants rated their quality of life as fair or poor.
Key Themes
Themes encompassed psychosocial and physical impacts of functional impairments and related adaptations (Table 2).
Psychosocial Impacts of Functional Impairment and Adaptations
Losses Associated with Functional Impairment Impact Sense of Identity
A 54-year-old man described how losing his ability to independently perform activities challenged his self-image: “It’s hard for me to accept the fact that I can’t do what I used to be able to do. And it disturbs me that I’m too damn young for this stuff.” A 53-year-old woman struggled with losing her autonomy, stating, “I’m already frustrated that I can’t open a water bottle…. I have to have somebody around.… I don’t like that feeling at all.”
Participants reported how functional impairment prevented them from fulfilling social roles. A 50-year-old woman noted the loss of the traditional role of an adult child helping a parent: “When I just came home from surgery, and my mom was with me…she would come to my room and say, ‘Would you like a snack?’…Deep inside of me, I said…, ‘No, I’m supposed be offering you a snack’…That was really hard. It was so depressing.” Another woman described the loss of her dual role as a worker and family caregiver: “I was a superwoman before the injury. I used to take care of both of my parents… and I worked full-time…. I was able to go here and there between my kids’ activity and full-time work.” Some participants described how losing their professional role represented a loss of identity. One 61-year-old woman explained, “One thing I really miss is being in the work world, working for the government, and doing service to people…. And what would make me feel better, [is] getting stronger to the point where I, again, could give back to the community…. To me, that’s a real important part of my life.”
Some participants noted changes in others’ perception of them after developing impairment. A 61-year-old woman described experiencing social exclusion: “I don’t go places a lot because I’ve been burned too many times in the past…. It’s made worse by the scooter and the disability because a lot of people don’t want to bother [talking to you] if you’re on a scooter or on a walker.” Other participants noted that others viewed them as needing assistance, which conflicted with their sense of self and independence. One 56-year-old woman reported, “When I start explaining to people…I’ve been operated on my back…suddenly they look at you a whole different way. And then [they say], ‘Oh, you shouldn’t be doing that’....Then I feel like, ‘No, you don’t have to pamper me.’”
Participants also described how functional impairment limited the amount of time spent outside their home. A 55-year-old woman reported how these limitations conflicted with how she had imagined her life: “My partner drives me to get a cup of coffee at my local coffee shop. And oftentimes that’s the only time I leave the house. If I’m having a relatively better time, I might…go to lunch, or maybe we’ll see a movie. But [my life is] pretty small….So I watch an inordinate amount of daytime TV, which kind of blows my mind. That was not my life plan.”
Coping Strategies Can Maintain One’s Sense of Identity
Common coping strategies included accepting limitations, comparing oneself to others, engaging in valued activities, adjusting expectations and standards, and maintaining social roles. A 61-year-old woman discussed accepting her impairment: “What I know now is to do what I can do. I prioritize what is it that I really want to do….The things I can control, I’m going to control, and recognize the things I can’t control. That’s the bottom line for me.” A 53-year-old woman viewed changing her attitude as a way to cope with functional decline: “If you take on the attitude that [functional impairment] is going to limit you, then…it’s a self-fulfilling prophecy.”
Some participants found inspiration to persevere by comparing themselves to others. A 50-year-old man recalled, “I had a… workout partner… Working next to a guy like that, you really can’t feel much pity [for yourself] because I could stand up… He literally had to… learn how to walk again. And… that kind of motivated me.”
Other participants coped with their loss of function by adjusting expectations. A 61-year-old woman explained, “I have my standards for how clean I want [my house] to be and I have to accept [my caregiver’s] standards…. Anytime there’s someone else doing your housework, it’s always on their standards and not yours.” Similarly, a 54-year-old man changed his standards of hygiene: “This past week I’ve taken two baths, which is pretty good….If I have to take a sink bath with a washcloth, I will....I remember as a young adult and as a kid growing up, man, I’d take three or four showers a day.”
Participants noted that consistent engagement in valued activities was crucial to maintain one’s identity and happiness. As a 55-year-old woman articulated, “You are what you do, who you interact with, where you go, what you see. And if you’re not doing any of those things, it’s pretty significant.” A 56-year-old woman explained, “Even with this… condition, I sometimes tell my husband to drive me to the beach... even parking lot… and not necessary to go… all the way down [to the] sands. So park the car, open the window, get the fresh air, and turn on the car music.... What I try to say is certain conditions stop us... but we need to also [change our] mindset ourselves to… find another happy way.”
Many participants noted that maintaining social roles was essential to preserve their identity, even as their functional abilities shifted. One 50-year-old woman was happy to be “able to do [her] daily thing again” after receiving surgery, such as “[being] a mother” and being “able to drop [her kids] to school.” Some participants created meaning from their functional impairment by pursuing new roles in community service. One 56-year-old man explained, “Because of my back problem, I got into the field of disabilities....I worked for almost 25 years for [city] and I created an organic gardening program for people with disabilities….My job helped me to stay active and live my life the way I wanted…and to help people.”
Functional Impairment that Develops in Middle Age Is Premature
Participants distinguished between functional impairment that occurs in middle versus older age. They noted that older people may have trouble with certain activities but are not “disabled,” because functional impairment is an expected phase of aging. In contrast, middle-aged participants identified as being “disabled.” As one participant articulated, “I had a disability. It started when I was 50…. I wasn’t older. I was... middle-aged.… Now, most people as they age, maybe they get arthritis in their hands, maybe they have it in their knees… but it’s part of aging.”
Other participants distinguished “natural” from premature aging. A 57-year-old woman explained, “I see [older people] walking down the street and getting in their exercise…. She… might be 70 or 80 years old, walking down the street, head up and just going. And I’m only 57 and I’ve got a cane. They are growing old gracefully and I’m growing old, breaking down.”
Some participants reflected on life experiences that possibly contributed to premature functional impairment. One 53-year-old woman reflected, “I’m worried about aging and [the chronic pain] getting worse as I age…. That leads me back to the psychosomatic stuff…. Did it all really occur because of this incredible stressful time in my life? And if it did, how do I get out of that?” A 61-year-old man blamed his occupation for his impairment: “My job was… extremely physical. I [was] lifting things that weigh 30, 40 pounds minimum… 20, 40 pounds over 40 years, that kinda adds up…. If steel, rubber, and brass wear out, what do you think bone is gonna do?”
Physical Impacts of Functional Impairment and Adaptations
A Lack of Accessible Environments Exacerbates Functional Impairment
Participants noted that the built environment was often not designed for those with impairments, leading to frustration. A 62-year-old woman explained: “Stairs are hard for me….Today I had to go up all the stairs at [the train station], ‘cause [neither the escalators nor elevators] worked, and I was like, really?” Another 50-year-old woman described the difficulty of needing assistance “any time [she has] to leave home,” stating, “I have to have somebody to lug my wheelchair up and down those stairs.”
Participants noted how inaccessible built environments exacerbated pain and physical limitations, leading to risk of injury. A 56-year-old man said, “The showers here [are] five foot in the wall and then I got to bend over trying to get in the shower… and... it has an effect on my back.” Other participants described how a lack of environmental modifications increased the risk of falling. One 60-year-old man with muscle weakness reported that the lack of restroom grab bars made it “very difficult [to stand] up from a sitting position [on the toilet],” explaining, “very loose support around me makes me take extra time to do it… so I don’t fall, which… has happened to me in the past.”
Behavioral Adaptations and Accommodations Can Help One Adjust to Functional Impairment
Many participants adapted to physical challenges by changing their behaviors and routines. Some participants described how making these changes made “little things feel much bigger,” as a 61-year-old woman described. For example, participants planned ahead for routine activities that would have previously required little thought. A 55-year-old woman recounted, “To get ready for the wedding... how do I start on Thursday to be ready for something that’s Sunday?... I’m gonna shave my armpits on Thursday... and then I’ll plan to do another thing. Like, I’m gonna break down stuff that [others] would just do in 10 minutes.” A 57-year-old woman explained how she divided activities into smaller tasks: “I might have to wipe off the table and I’ll sit there for a minute. Then I’ll sweep the floor sitting down.” One 56-year-old woman described splitting tasks among family: “Laundry day, my son and my husband do that. And then, the vacuum, my husband do that. So pretty much, I try to arrange my room. Not the whole household.”
Participants found resourceful ways to accommodate impairments using the built environment. A 50-year-old woman described how she “walked against a wall, [because I’d] be scared to fall down.” Other participants repurposed objects in innovative ways. One 54-year-old woman noted, “I use a shopping cart for a walker. So even if I’m only getting a couple of items, I still get a cart.” Other participants redesigned their environments to facilitate activities. A 54-year-old man detailed, “My recliner in my bedroom, I’ve taken 4x4s and lifted it up 4 inches, and my bed, so when I roll over… my legs are going straight down so I’m not having to start from [a horizontal position]. I’m trying to get myself halfway there.”
Intended Solutions for Functional Impairment Are Often Inadequate
Despite making adaptations, participants faced barriers in using equipment and services, leading to frustration, fear, and lack of control. For example, participants found that equipment intended to improve function was not always “user friendly.” A 62-year-old man recalled the inconvenience of transporting his wheelchair: “Medicare gave me a great big, huge heavy wheelchair a few years back that... we can’t even get down our steps.” Other participants noted that even with accommodations, fears of falling remained. A 62-year-old man detailed, “Bathing is a scary one…. I have grab rails and things, but it still can be scary… getting in and out of the bathroom, because that’s the most… dangerous. You can fall and hurt yourself.”
Participants reported that some “accessible” services failed to accommodate persons with disabilities. A 57-year-old woman recalled, “It’s a lot of work I need to do to take the bus. And then... [the] driver… [does not] want to use their lift. So, I said, never mind. I’ll [walk] with the walker even though it’s six hours.” Participants also reported that services could be unreliable. A 61-year-old woman described her fears when using paratransit: “Paratransit was busy that day. So I couldn’t… find out what time it was coming…. I could have gotten home on the bus from there. But what if it was nighttime? What if it was farther away where there’s no direct bus service? What if it was raining hard and they didn’t come? And it’s not the first time they stranded me.”
Conceptual Model of Functional Impairment in Middle Age
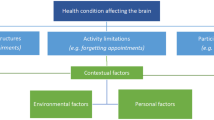
We used these findings to develop a model conceptualizing the impacts of functional impairment among middle-aged adults (Fig. 1). The model depicts how psychosocial and physical challenges lead to adaptations but can also result in unmet needs. In turn, unmet needs and inadequate adaptations lead to downstream health consequences. Reciprocally, health consequences compel participants to further adapt and can result in unmet needs. The model also highlights potential points where clinicians can intervene to prevent downstream health consequences.
Conceptual model of adaptations, unmet needs, and consequences of functional impairment that develops in middle age. Based on the results of qualitative analysis of interviews with 40 middle-aged adults with functional impairment, the model illustrates the relationship between the psychosocial and physical challenges of developing functional impairment in middle age, adaptations to these challenges, unmet needs resulting from barriers to adaptation, and downstream health impacts of unmet needs and inadequate adaptations to challenges. These relationships help to explain the impacts and adaptations that result from developing functional impairment in middle age and identify potential intervention points to address unmet needs. Specifically, providers can help patients maintain a sense of identity by making referrals for psychosocial support, and they can help patients address physical limitations by prescribing equipment or services.
DISCUSSION
In this qualitative study, middle-aged adults shared the psychosocial and physical impacts of functional impairment and how they adapted to these challenges. The inability to address challenges led to mental and physical health consequences, suggesting that understanding common unmet needs among middle-aged adults with functional impairment is necessary to deliver optimal care.
Consistent with prior studies among adults of all ages with congenital and acquired functional impairment, our study identified factors that caused conflict in participants’ identities. These included loss of independence17,18 and social roles,17 discrimination,19,20,21 and changes in how society viewed participants.17,22,23,24 Our study also revealed unique perspectives on the intersection of aging and functional impairment acquired in middle age. Participants viewed impairment in middle age as a disability or sign of premature aging, in contrast to “normal” and “natural” age-related functional decline among older adults. These beliefs reflect ageist ideas prevalent in the USA that aging represents decline or deterioration.45 These comparisons led some participants to blame themselves and regret choices that they perceived as contributing to their impairments.
Participants used coping strategies to reconcile conflict in their sense of identity. Several coping strategies were consistent with those identified previously in middle-aged and older adults, including acceptance,24,25,26,27,28 adjusting one’s attitude,24,27,33 continuing valued life activities,24,26 maintaining social roles,25,26 and adjusting standards.25,26 A unique coping strategy was social comparison, in which participants found solace and inspiration in those with more severe impairment. Although previous studies show that social comparison in people with disabilities is associated with worse mental health,46,47,48 participants in our study used social comparison to improve self-esteem and increase motivation.
The physical challenges that participants faced often stemmed from inaccessible built environments. Consistent with prior studies of middle-aged and older adults, participants changed their behavior in response to these challenges, including planning ahead25,27 and limiting activities.24 Participants also repurposed the environment and equipment to accommodate impairment. Despite making adaptations, participants faced persistent barriers, such as difficult-to-use equipment and unreliable paratransit. These barriers resulted in unmet needs and physical and psychosocial consequences. Physical consequences included pain, safety risks, functional decline, and restricted life space49,50 and led to negative emotions, including fear, denial, anger, depression, and self-blame.
These findings have clinical implications. As depicted in our conceptual model, primary care providers (PCPs) have an opportunity to disrupt downstream health consequences by identifying unmet needs and providing services to address them. PCPs may benefit from understanding the general coping processes involved in forming a “disability identity,” so they can better recognize unmet psychosocial needs and refer patients for additional psychosocial support.22 In fact, studies show that patients with spinal cord injuries who learn coping strategies adapt better to their impairment27 and exhibit lower levels of anxiety, depression, and anger.51
The persistent physical challenges faced by participants underscore the need for an iterative follow-up process by a multidisciplinary team of providers, social workers, and case managers to determine if services and supports are assisting patients as intended.52 Developing a reliable tool to identify unmet needs would help guide care teams in referring patients to appropriate services. Findings also point to structural barriers preventing full social participation by individuals with functional impairments,53 particularly inaccessible and unreliable transit options, which are heightened among those with limited financial resources.54 Providers may help address these structural barriers through advocacy for service and policy changes.
The points of intervention identified in our model are consistent with Rowe and Kahn’s Model of Successful Aging, which proposes that adapting to environmental, societal, and individual factors can promote quality of life for those aging with disabilities.43 Our conceptual model also expands upon aspects of Verbrugge’s Model of Disablement, which illustrates the progression from impairment to disability and the intrinsic and extrinsic factors affecting this process.44 Our model examines specific intrinsic and extrinsic factors that affect adaptation to functional impairment and how interventions can assist. Because many of these challenges and adaptations parallel those in older adults, our model may be generalizable to adults of all ages. Furthermore, these parallels suggest that middle-aged and older adults may benefit from similar interventions.
Our study has limitations. While our sample was racially diverse, the proportion of individuals identifying as Latino/Hispanic was lower than in the general California population. Thus, our findings may not be transferrable to more ethnically diverse populations. However, patients were recruited from a range of primary care settings and socioeconomic strata. To mitigate selection bias, PCPs reviewed lists of all patients aged 50–64. While it is possible that providers selected patients with severe or visible physical impairments, one-third of our sample had difficulty with ADLs rather than needing help, and our findings are consistent with research among individuals with varying etiologies and severity of impairments.17,18,22,25,26,28,33
In conclusion, participants noted psychosocial and physical challenges they faced as middle-aged adults with functional impairment and adaptations they made to address those challenges. They also shared downstream health consequences of unmet needs. For the growing population of middle-aged adults with functional impairment, eliciting and addressing unmet psychosocial and physical needs may help mitigate downstream health consequences, optimizing function and quality of life.
References
Melzer D, McWilliams B, Brayne C, Johnson T, Bond J. Socioeconomic status and the expectation of disability in old age: estimates for England. J Epidemiol Community Health. Apr 2000;54(4):286-92. https://doi.org/10.1136/jech.54.4.286
Grundy E, Holt G. Adult life experiences and health in early old age in Great Britain. Soc Sci Med. Oct 2000;51(7):1061-74. https://doi.org/10.1016/s0277-9536(00)00023-x
Gardener EA, Huppert FA, Guralnik JM, Melzer D. Middle-aged and mobility-limited: prevalence of disability and symptom attributions in a national survey. J Gen Intern Med. Oct 2006;21(10):1091-6. https://doi.org/10.1111/j.1525-1497.2006.00564.x
Martin LG, Freedman VA, Schoeni RF, Andreski PM. Trends in disability and related chronic conditions among people ages fifty to sixty-four. Health Aff (Millwood). Apr 2010;29(4):725-31. https://doi.org/10.1377/hlthaff.2008.0746
Martin LG, Schoeni RF. Trends in disability and related chronic conditions among the forty-and-over population: 1997-2010. Disabil Health J. Jan 2014;7(1 Suppl):S4-14 https://doi.org/10.1016/j.dhjo.2013.06.007
Crimmins EM, Beltrán-Sánchez H. Mortality and morbidity trends: is there compression of morbidity? J Gerontol B Psychol Sci Soc Sci. Jan 2011;66(1):75-86. https://doi.org/10.1093/geronb/gbq088
Freedman VA, Spillman BC, Andreski PM, et al. Trends in late-life activity limitations in the United States: an update from five national surveys. Demography. Apr 2013;50(2):661-71. https://doi.org/10.1007/s13524-012-0167-z
Zajacova A, Montez JK. Physical functioning trends among US women and men age 45-64 by education level. Biodemography Soc Biol. 2017;63(1):21-30. https://doi.org/10.1080/19485565.2016.1263150
Zajacova A, Montez JK. Explaining the increasing disability prevalence among mid-life US adults, 2002 to 2016. Soc Sci Med. 2018;211:1-8. https://doi.org/10.1016/j.socscimed.2018.05.041
Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112(49):15078-83. https://doi.org/10.1073/pnas.1518393112
Case A, Deaton A. Mortality and morbidity in the 21. Brookings Pap Econ Act. Spring 2017 2017;2017:397-476. https://doi.org/10.1353/eca.2017.0005
Brown RT, Diaz-Ramirez LG, Boscardin WJ, Lee SJ, Williams BA, Steinman MA. Association of functional impairment in middle age with hospitalization, nursing home admission, and death. JAMA Intern Med. 2019;179(5):668-675. https://doi.org/10.1001/jamainternmed.2019.0008
Iezzoni LI. Policy concerns raised by the growing U.S. population aging with disability. Disabil Health J. Jan 2014;7(1 Suppl):S64-8. https://doi.org/10.1016/j.dhjo.2013.06.004
Krahn GL, Walker DK, Correa-De-Araujo R. Persons with disabilities as an unrecognized health disparity population. Am J Public Health. Apr 2015;105 Suppl 2:S198-206. https://doi.org/10.2105/AJPH.2014.302182
Jamoom EW, Horner-Johnson W, Suzuki R, Andresen EM, Campbell VA, Measurement REPoHS. Age at disability onset and self-reported health status. BMC Public Health. 2008;8:10. https://doi.org/10.1186/1471-2458-8-10
Kim WS, Cho SI, Shin HI, Park JH. Identifying factors associated with self-rated health according to age at onset of disability. Disabil Rehabil. 2012;34(15):1262-70. https://doi.org/10.3109/09638288.2011.641656
Galvin RD. Researching the disabled identity: contextualising the identity transformations which accompany the onset of impairment. Sociol Health Illn. Apr 2005;27(3):393-413. https://doi.org/10.1111/j.1467-9566.2005.00448.x
Dewar A. Protecting strategies used by sufferers of catastrophic illnesses and injuries. J Clin Nurs. Sep 2001;10(5):600-8. https://doi.org/10.1046/j.1365-2702.2001.00536.x
Dunn DS, Burcaw S. Disability identity: exploring narrative accounts of disability. Rehabil Psychol. May 2013;58(2):148-57. https://doi.org/10.1037/a0031691
Trost Z, Agtarap S, Scott W, et al. Perceived injustice after traumatic injury: associations with pain, psychological distress, and quality of life outcomes 12 months after injury. Rehabil Psychol. Aug 2015;60(3):213-221. https://doi.org/10.1037/rep0000043
Silverman AM, Cohen GL. Stereotypes as stumbling-blocks: how coping with stereotype threat affects life outcomes for people with physical disabilities. Pers Soc Psychol Bull. Oct 2014;40(10):1330-40. https://doi.org/10.1177/0146167214542800
Forber-Pratt AJ, Lyew DA, Mueller C, Samples LB. Disability identity development: a systematic review of the literature. Rehabil Psychol. 2017;62(2):198-207. https://doi.org/10.1037/rep0000134
Riley D, de Anda D, Blackaller CA. The self-perceptions and interpersonal relationships of persons with significant physical disabilities: a qualitative pilot study. J Soc Work Disabil Rehabil. 2007;6(3):1-31. https://doi.org/10.1300/J198v06n03_01
Pallesen H. Body, coping and self-identity. A qualitative 5-year follow-up study of stroke. Disabil Rehabil. 2014;36(3):232-41. https://doi.org/10.3109/09638288.2013.788217
Cooper M, Bigby C. Cycles of adaptive strategies over the life course. J Gerontol Soc Work. 2014;57(5):421-37. https://doi.org/10.1080/01634372.2013.875972
King G, Cathers T, Brown E, et al. Turning points and protective processes in the lives of people with chronic disabilities. Qual Health Res. Feb 2003;13(2):184-206. https://doi.org/10.1177/1049732302239598
Livneh H, Martz E. Coping strategies and resources as predictors of psychosocial adaptation among people with spinal cord injury. Rehabil Psychol. Aug 2014;59(3):329-39. https://doi.org/10.1037/a0036733
Charmaz K. The body, identity, and self: adapting to impairment. The Sociological Quarterly. 1995;36(4):657-680. https://doi.org/10.1111/j.1533-8525.1995.tb00459.x
Rippon I, Steptoe A. Feeling old vs being old: associations between self-perceived age and mortality. JAMA Intern Med. Feb 2015;175(2):307-9. https://doi.org/10.1001/jamainternmed.2014.6580
Gayman MD, Turner RJ, Cui M. Physical limitations and depressive symptoms: exploring the nature of the association. J Gerontol B Psychol Sci Soc Sci. Jul 2008;63(4):S219-S228. https://doi.org/10.1093/geronb/63.4.s219
Du Mont J, Forte T. Perceived discrimination and self-rated health in Canada: an exploratory study. BMC public health. 2016;16:742. https://doi.org/10.1186/s12889-016-3344-y
Bogart KR. The role of disability self-concept in adaptation to congenital or acquired disability. Rehabil Psychol. Feb 2014;59(1):107-15. https://doi.org/10.1037/a0035800
Persson LO, Rydén A. Themes of effective coping in physical disability: an interview study of 26 persons who have learnt to live with their disability. Scand J Caring Sci. Sep 2006;20(3):355-63. https://doi.org/10.1111/j.1471-6712.2006.00418.x
Cigolle CT, Lee PG, Langa KM, Lee YY, Tian Z, Blaum CS. Geriatric conditions develop in middle-aged adults with diabetes. J Gen Intern Med. Mar 2011;26(3):272-9. https://doi.org/10.1007/s11606-010-1510-y
Sudore RL, Landefeld CS, Williams BA, Barnes DE, Lindquist K, Schillinger D. Use of a modified informed consent process among vulnerable patients: a descriptive study. J Gen Intern Med. Aug 2006;21(8):867-73. https://doi.org/10.1111/j.1525-1497.2006.00535.x
Lewis-Beck MS, Bryman A, Liao TF. The SAGE Encyclopedia of Social Science Research Methods. Sage Publications; 2004.
Patton MQ. Qualitative Research and Evaluation Methods. 3rd ed: Sage Publications; 2002.
Nicosia FM, Spar MJ, Neumann A, Silvestrini MC, Barrientos M, Brown RT. “The more they know, the better care they can give”: patient perspectives on measuring functional status in primary care. J Gen Intern Med. 2020;35(10):2947-2954. https://doi.org/10.1007/s11606-020-06075-8
Albert SM, Bear-Lehman J, Burkhardt A. Lifestyle-adjusted function: variation beyond BADL and IADL competencies. Gerontologist. Dec 2009;49(6):767-77. https://doi.org/10.1093/geront/gnp064
Baum CM, Edwards DF. Activity Card Sort. 2001.
Covinsky KE, Wu AW, Landefeld CS, et al. Health status versus quality of life in older patients: does the distinction matter? Am J Med. Apr 1999;106(4):435-40. https://doi.org/10.1016/s0002-9343(99)00052-2
Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. International Journal of Qualitative Methods. 2006 ;5(1):80-92. https://doi.org/10.1177/160940690600500107
Tesch-Römer C, Wahl HW. Toward a more comprehensive concept of successful aging: disability and care needs. J Gerontol B Psychol Sci Soc Sci. 2017;72(2):310-318. https://doi.org/10.1093/geronb/gbw162
Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. Jan 1994;38(1):1-14. https://doi.org/10.1016/0277-9536(94)90294-1
Gullete MM. Declining to decline: cultural combat and the politics of the midlife. University Press of Virginia; 1997.
Carrieri V. Social comparison and subjective well-being: does the health of others matter? Bull Econ Res. 2012;64(1):31-55. https://doi.org/10.1111/j.1467-8586.2011.00393.x
Dagnan D, Sandhu S. Social comparison, self-esteem and depression in people with intellectual disability. J Intellect Disabil Res. Oct 1999;43 ( Pt 5):372-9. https://doi.org/10.1046/j.1365-2788.1999.043005372.x
Paterson L, McKenzie K, Lindsay B. Stigma, social comparison and self-esteem in adults with an intellectual disability. J Appl Res Intellect Disabil. Mar 2012;25(2):166-76. https://doi.org/10.1111/j.1468-3148.2011.00651.x
Poranen-Clark T, von Bonsdorff MB, Rantakokko M, et al. Executive function and life-space mobility in old age. Aging Clin Exp Res. Feb 2018;30(2):145-151. https://doi.org/10.1007/s40520-017-0762-3
Poranen-Clark T, von Bonsdorff MB, Rantakokko M, et al. The temporal association between executive function and life-space mobility in old age. J Gerontol A Biol Sci Med Sci. 2018;73(6):835-839. https://doi.org/10.1093/gerona/glx217
Lustig DC. The adjustment process for individuals with spinal cord injury: the effect of perceived premorbid sense of coherence. Rehabilitation Counseling Bulletin. 2005 ;48(3):146-156. https://doi.org/10.1177/00343552050480030301
Canguilhem G. What is health? The ability to adapt. The Lancet. 2009;373(9666):781. https://doi.org/10.1016/S0140-6736(09)60456-6
Shakespeare T. Social models of disability and other life strategies. Scandinavian Journal of Disability Research. 2004;6:8-21. https://doi.org/10.1080/15017410409512636
Visagie S, Eide AH, Dyrstad K, et al. Factors related to environmental barriers experienced by persons with and without disabilities in diverse African settings. PLoS One. 2017;12(10):e0186342. https://doi.org/10.1371/journal.pone.0186342
Contributors
The authors do not have any additional contributors to report.
Funding
This work was supported by grants K76AG057016 (Dr. Brown), K23AG045290 (Dr. Brown), and K24AG067003 (Dr. Karliner) from the National Institute on Aging at the National Institutes of Health and by the American Federation for Aging Research (grant K76AG057016 to Dr. Brown).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior Presentations: This manuscript was presented as a poster at the 2018 Annual Scientific Meeting of the Gerontological Society of America in Boston, MA in November 2018.
Rights and permissions
About this article
Cite this article
Xu, E., Nicosia, F.M., Zamora, K. et al. When Functional Impairment Develops Early: Perspectives from Middle-Aged Adults. J GEN INTERN MED 38, 90–97 (2023). https://doi.org/10.1007/s11606-022-07541-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-022-07541-1